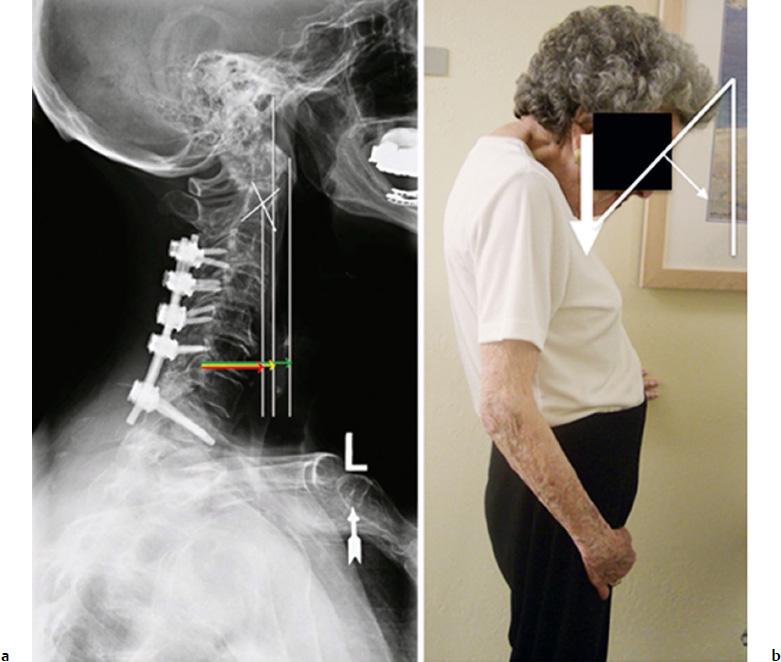
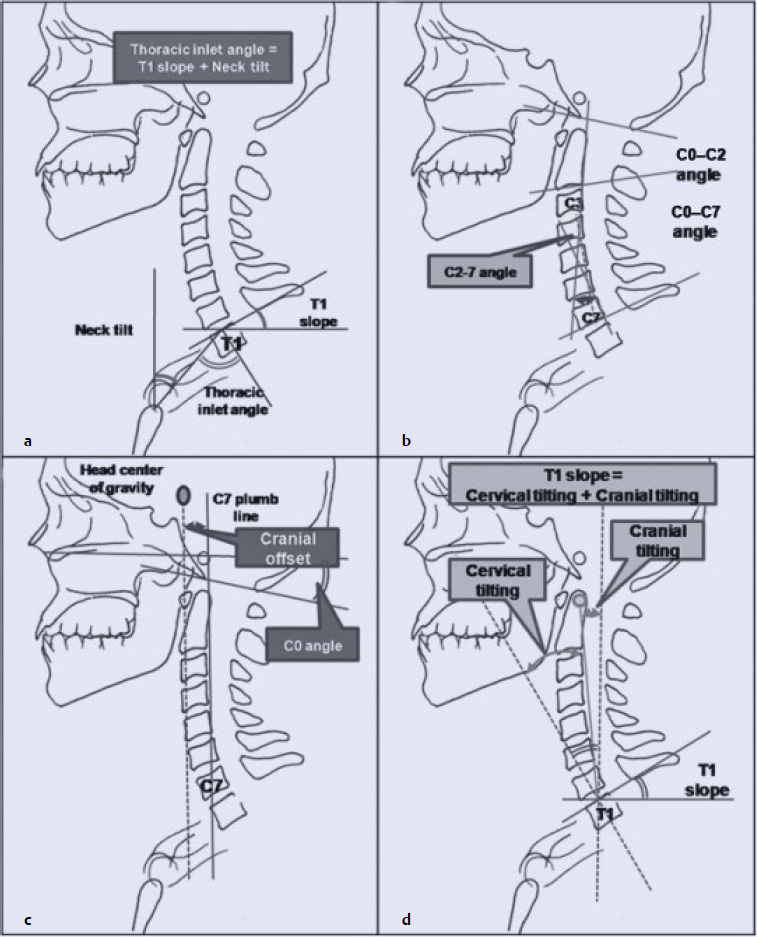
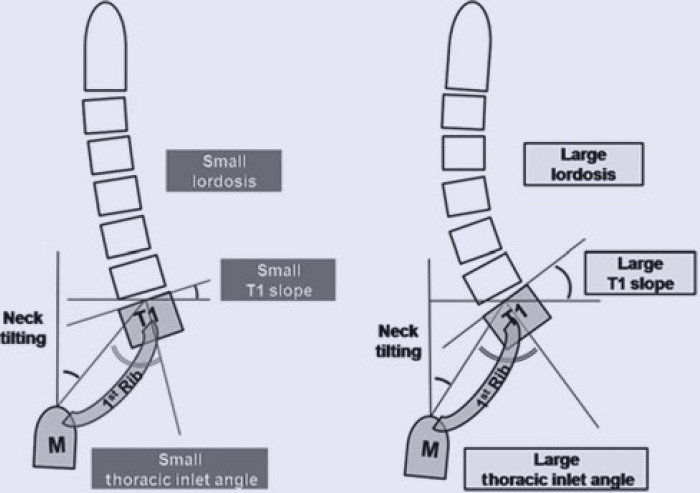
8 Cervical sagittal balance has been receiving increasing attention by researchers and spine surgeons in recent years. Cervical spine anatomy is very complex, and as such determining “normal” alignment has proven to be difficult. Despite this, many advances have been made regarding which measurements of the cervical spine are most important and how these measurements correlate with neurologic status, overall sagittal balance, and health-related quality-of-life (HRQOL) scores. This chapter discusses normal cervical alignment, cervical sagittal imbalance, the effect of sagittal malalignment on disability, and how to achieve optimal sagittal alignment in reconstruction. The cervical spine is a complex anatomic structure that functions to support the mass of the head while providing a range of motion that is greater than any other area of the spine, and protecting the spinal cord and accompanying neurovascular structures.1 The upper cervical spine, including the occipitoatlantal (C0–C1) and the atlantoaxial (C1–C2) joints, is anatomically distinct from the lower cervical spine. Unique upper cervical anatomic characteristics include the absence of intervertebral disks, the absence of the ligamentum flavum, and the unique osseous anatomy of C1 and C2. The coupled motion in the upper cervical spine results in 40% of total cervical flexion and extension and 60% of total cervical rotation.2 The lower cervical spine provides significant flexion and extension in the sagittal plane, with limited rotation and bending due to the inclination of the facet joints posteriorly. The cervical spine is arranged in a lordotic configuration, largely due to wedge-shaped intervertebral disks. This curvature is considered a primary curve of the spine because it is formed at about 10 weeks in utero.1 The cervical spine joins the thoracic spine at the relatively immobile thoracic inlet.1 When considering overall alignment, it is important to determine the forces acting on the cervical spine. The center of mass of the head in the sagittal plane is located ~ 1 cm above and anterior to the external auditory meatus and overlies the occipital condyles.1 As the head is tilted about this axis, increasing cantilever loads in the cervical spine are opposed by the paraspinous muscles. The stability of the cervical spine to support the mass of the head has been described as originating from three columns, one anterior and two posterior. The anterior column is composed of the vertebral bodies and intervertebral disks, whereas the two posterior columns consist of the articulating facet joints. The load of the head is transferred from the occipital condyle to the C2 vertebrae via the lateral masses of C1. At this point the load is divided into the anterior column via the C2–C3 disk and posterior columns via the C2–C3 articulating facet joints. The anterior column supports 36% of the load, whereas the two posterior columns support the remaining 64%. This contrasts with the lumbar spine in which the anterior loads are higher than posterior loads (67–82% and 18–33%, respectively).1 Cervical sagittal plane alignment can be described using angular parameters (“lordosis” or “kyphosis”) or translational parameters (“positive,” “negative,” or “neutral”). Angular and translational alignment parameters are closely interrelated. There are three methods of measuring overall cervical lordosis from a lateral radiograph: the four-line Cobb method, the Harrison posterior tangent method, and the Jackson physiological stress line method.3 C2–C7 Cobb angles are obtained by drawing a line parallel to the inferior end plate of C2 and another line parallel to the inferior end plate of C7. Perpendicular lines are drawn from each of these lines, and the angle subtended by their intersection is the Cobb angle. C1–C7 Cobb angles are created similarly, but with the superior line drawn through the posterior ring and anterior tubercle of C1.1 The Harrison posterior tangent method is completed by drawing tangential lines to the posterior aspects of all C2–C7 vertebral bodies and adding each segmental angle to determine the overall curvature.3 The Jackson physiological stress line method is a simplified version of the Harrison method that is performed by drawing tangential lines to the posterior aspects of the C2 and C7 vertebral bodies and determining the angle created by their intersection. Harrison et al3 compared the Cobb C1–C7 method, the Cobb C2–C7 method, and the Harrison method and concluded that all have high inter- and intraclass correlation coefficients between 0.7 and 1.0. Additionally, C1–C7 Cobb angles were shown to overestimate lordosis, whereas C2–C7 Cobb angles underestimated lordosis. Despite higher standard errors of measurement found with the Cobb method, it is still frequently used in assessing cervical lordosis and kyphosis. Segmental alignment is largely measured using end plate tangent lines with the Cobb method. Overall sagittal balance represents the position of the occiput relative to the thoracic inlet. There are several techniques to measure sagittal balance by measuring the horizontal distance from a vertical reference line to a fixed parameter on the thoracic inlet. Common locations used for plumb lines include the anterior margin of C1 (C1–C7 sagittal vertical axis [SVA]), the centroid of C2 (C2–C7 SVA), and the anterior portion of the external auditory canal (Center of Gravity of the Head [CGH]–C7 SVA).4 Common locations for the plumb line of C7 include the posterior aspect of the superior end plate and the centroid4,5 (Fig. 8.1). Another technique involves measuring the angular orientation of the occiput relative to the thoracic inlet. These techniques may be less susceptible to artifact due to patient height and body size. Cervical tilt is defined as the angle made by a perpendicular line from the center of the T1 superior end plate and a line from the center of the T1 superior end plate to the tip of the dens.6,7 Cranial tilt is defined as the angle formed by a line from the center of the T1 superior end plate to the dens and a plumb line drawn from the center of the T1 superior end plate6 (Fig. 8.2d). Evaluation of horizontal gaze can be important in patients with severe cervical kyphotic deformities, as gaze impairments in these patients can significantly impact quality of life. To measure horizontal gaze the chin–brow vertical angle (CBVA) is used.8 This is measured in the clinic or from a photograph of the patient standing with the neck in a neutral or fixed position. The CBVA is the angle subtended between a line drawn from the patient’s chin to the patient’s brow and a vertical line8 (Fig. 8.1). Fig. 8.1a,b Cervical sagittal vertical axis (SVA) measurements (a) and chin–brow vertical angle (CBVA) (b). (a) The green arrow represents the C1–C7 SVA (distance between a plumb line dropped from the anterior tubercle of C1 and the posterior superior corner of C7). The red arrow represents the C2–C7 SVA (distance between a plumb line dropped from the centroid of C2 and the posterior superior corner of C7). The yellow arrow represents the center of gravity to the C7 SVA (distance between a plumb line dropped from the anterior margin of the external auditory canal and the posterior superior corner of C7). (b) Representation of the CBVA measurement method portrayed on a clinical photograph of a patient standing with hips and knees extended while her neck is in a neutral or flexed position. The CBVA is defined as the angle subtended between a line drawn from the patient’s chin to brow and a vertical line.1 Recently, thoracic inlet angle (TIA), T1 slope, and neck tilt have been introduced as parameters to help correlate cervical sagittal alignment with thoracolumbar sagittal alignment (Fig. 8.2a).6,7 All of the following measurements are determined from lateral radiographs. Neck tilt is defined as the angle formed by two lines originating from the sternum, one that extends vertically and one that connects to the center of the T1 superior end plate. TIA is defined as the angle formed by a line perpendicular to the center of the T1 superior end plate and a line connecting the center of the T1 superior end plate and the upper end of the sternum. TIA is a constant measurement and is not affected by posture because of the previously mentioned rigidity of the thoracic inlet. T1 slope is the angle made by a horizontal line through the center of the T1 superior end plate and a line parallel to the T1 superior end plate. Using these measurements, a geometrically defined relationship can be made such that TIA = NT + T1 slope, which is similar to the relationship that exists at the lumbopelvic junction (pelvic incidence = pelvic tilt + sacral slope). The T1 slope is equivalent to the sum of the cervical tilt and cranial tilt.6,7 Fig. 8.2a–d Schematic drawing of cervical alignment parameters. (a) Thoracic inlet parameters. (b) Cervical spine parameters. (c) Cranial parameters. (d) Craniocervical alignment parameters.6 A consensus has yet to be reached concerning “normal” cervical alignment. Multiple studies have presented measurement data from asymptomatic populations with varied results.4–7,9–11 Hardacker et al5 reported an average total lordotic cervical curvature (occiput to C7) of –40 ± 9.7 degrees using the Cobb method from the foramen magnum to the inferior end plate of C7.5 Gore et al9 used the Jackson physiological stress line method to determine an average cervical lordosis (C2–C7) of 23 degrees in asymptomatic patients who did not demonstrate any areas of local kyphosis. Yukawa et al10 found an average C2–C7 lordosis of 13.9 ± 12.3 degrees using the Cobb method in 1,200 asymptomatic Japanese subjects. These values correlate with Harrison et al’s3 observation that C2–C7 Cobb measurements underestimate lordosis because of the orientation of the C2 inferior end plate. Additionally, Cobb measurements beginning above the body of C2 overestimate lordosis because 75 to 80% of total cervical lordosis occurs at the C1–C2 level.4,5 Differences in measurement technique may explain the differences between average lordosis measurements found in these studies; however, each study found a large range of asymptomatic lordotic angles. In fact, some studies have even shown overall kyphotic alignment in as many as 2 to 35% of asymptomatic patients.7 Multiple investigators have agreed that there is no significant difference in cervical lordosis between males and females.9,10 Additionally, it has been shown that average cervical lordosis does change significantly with age, tending toward more lordosis with increased age.5,9,10 Standard values for CBVA have not been evaluated in asymptomatic patients; however, postoperative CBVA values of +10 to –10 degrees have been well tolerated.1 These studies are also limited by differences in radiographic technique and the arm position (abducted versus adducted versus under traction). In contrast to the high variability seen in cervical lordosis angles, measurements of cervical sagittal balance by C2–C7 SVA have demonstrated a narrower distribution, on average 16.8 ± 11.2 mm (in this case measured from the center of C7 to a plumb line from the odontoid) in standing volunteers.5 The mean cranial offset (measured as the distance between the C7 plumb line and a plumb line from 8 mm anterior to the external auditory meatus) in asymptomatic volunteers has been shown to be 20 mm.6 These types of standard measurements mirror those that have previously been used in determining thoracolumbar sagittal balance. Glassman et al12 studied the relationship among a plumb line drawn from the center of C7, a plumb line from the posterior superior corner of S1 (C7–S1 SVA), and the outcome of thoracolumbar reconstruction. If the C7 plumb line was more than 5 cm anterior to the posterior superior corner of S1, this was defined as positive sagittal balance. A relationship was found between increasing positive sagittal balance and worsening HRQOL scores in patients with no prior surgery (Spearman rho values ranged between 0.207 and 0.292 depending on which HRQOL score was used). For the thoracolumbar spine, a C7–S1 SVA greater than 50 mm has traditionally been defined as sagittal malalignment because it is more than 2 standard deviations (2.5 cm) from normal alignment.1,4 A similar conclusion concerning the cervical spine has since been proposed by Tang et al,4 who reported that “a C2 plumb line greater than approximately 40 mm from the posterior superior aspect of C7 (in the standing position) suggests a clinical concern of cervical sagittal malalignment that may negatively impact HRQOL.” In this study, 113 patients were followed postoperatively after receiving single-stage long-segment posterior cervical fusion of three or more segments. The Pearson r value for C2–C7 SVA and Neck Disability Index (NDI) scores was 0.2015. A logistic regression model predicted the lowest p value (p = 0.011, ξ2 = 6.60) at a C2–C7 SVA value of 41 mm. Additionally, a linear regression predicted a threshold C2–C7 SVA value of 37 mm for an NDI score of 25 (r2 = 0.04, p = 0.037). The definition for cervical sagittal malalignment described by Tang et al is consistent with the normal C2–C7 SVA range reported by Hardacker et al.5 Lee at al6 analyzed asymptomatic patients and found that the average TIA, T1 slope, and neck tilt measurements were 69.5 ± 8.6, 25.7 ± 6.4, and 43.7 ± 6.1 degrees, respectively. Additionally, they found that the average cervical tilting and cranial tilting were 18 ± 6.6 and 7.7 ± 5 degrees, respectively. Significant correlations exist among TIA, the T1 slope, and the C2–C7 angle, which in turn correlate with the C0–C2 angle and cranial offset angle.6,11 TIA, unlike thoracic kyphosis, is a stable measurement that does not change with posture and thus is an important anatomic landmark to assist in evaluation of cervical sagittal balance. Additionally, a neck tilt in the upright position was preserved at about 44 degrees in the Lee et al study to minimize neck muscle energy expenditure. With neck tilt stable, T1 slope reliably increased or decreased in accordance with TIA by the equation TIA = NT + T1 slope. Increased TIA and T1 slope significantly correlated with increased C2–C7 lordosis, whereas decreased TIA and T1 slope correlated with decreased cervical lordosis6 (Fig. 8.3). Conceptually, we would expect that the alignment of the thoracolumbar spine would influence the alignment of the cervical spine. Significant correlations exist between pelvic parameters and thoracolumbar parameters, which in turn correlate with cervical alignment. Pelvic incidence has been shown to correlate with lumbar lordosis, which in turn correlates with thoracic kyphosis, which correlates with T1 slope and the C0–C7 angle but not with TIA or the C2–C7 angle7 (Fig. 8.4). However, pelvic incidence does not directly correlate with thoracic kyphosis (Fig. 8.4). Thus, lumbar lordosis appears to be dependent on both thoracic kyphosis and pelvic incidence, whereas thoracic kyphosis appears to be independent of pelvic incidence.7 Overall it appears that pelvic incidence and TIA are the main determining factors of global sagittal alignment, whereas lumbar lordosis and cervical lordosis act in more adaptive or compensatory roles. Cervical lordosis is important for maintaining horizontal gaze, as changes in cervical lordosis are not large enough on their own to maintain the head over the pelvis in cases of increased thoracic kyphosis.1 These correlations explain results from Smith et al13 that describe spontaneous reciprocal improvement in cervical hyperlordosis (specifically involving the T1 slope and C2–C7 SVA) following surgical correction of thoracolumbar sagittal malalignment. Because cervical alignment is inevitably tied to global spinal alignment, preoperative evaluation for cervical spine correction should include 3-foot standing radiographs to most effectively evaluate the global parameters listed above.1,8
Cervical Sagittal Balance: What Is Normal and What Is the Effect on Reconstruction Outcomes
 Introduction
Introduction
 Cervical Spine Anatomy
Cervical Spine Anatomy
 Measurements of Cervical Sagittal Alignment
Measurements of Cervical Sagittal Alignment
Measuring Cervical Angular Alignment
Measuring Cervical Sagittal Balance
Measuring Cervical Horizontal Gaze
Relationship Between Cervical Alignment and Thoracolumbar or Global Alignment
 Normal Cervical Sagittal Balance
Normal Cervical Sagittal Balance
Normal Cervical Angular Alignment
Normal Cervical Sagittal Balance
Reciprocal Relationships
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree