Carpal fractures and dislocations
INTRODUCTION
There is a dearth of literature relating to carpal fractures and dislocations in the elderly patient. This is to be expected, given that the vast majority of carpal injuries occur in a young and active population. The diagnosis of carpal injuries can be challenging in all patients, irrespective of age, with the diagnosis of suspected scaphoid fractures a continuing dilemma despite the various advanced imaging modalities now available. The diagnosis and management of carpal injuries in the elderly patient can be particularly challenging. Degenerative changes may potentially mask acute pathology and the demands of the patient are different to those of the younger population who normally present with these injuries.
The most common injury of the carpus is a fracture of the scaphoid. Although there are advocates for percutaneous fixation over casting for non- and minimally displaced scaphoid waist fractures in the younger patient, there is no evidence to suggest that this would be of benefit in the elderly population. Given the potential issues with carpal instability and non-union, displaced fractures and proximal pole fractures routinely require operative intervention. One of the most devastating carpal injuries is a perilunate dislocation or fracture-dislocation. Again, these are rare in the elderly and operative intervention is routinely necessary to try and regain wrist function and prevent disability.
The elderly patient will potentially attend with the chronic sequelae of a previous carpal injury, for example, the scaphoid non-union advanced collapse (SNAC) wrist. The management options in this situation can be difficult, as the customary treatment in the younger patient may not be appropriate or necessary in the elderly.
EPIDEMIOLOGY
There is limited literature documenting the epidemiology of all carpal injuries, with most of the data related to the epidemiology of scaphoid fractures. The literature consistently suggests that carpal fractures account for 2–3% of all fractures with an incidence of 37.5 per 100,000 adult individuals per year.1,2 The overall mean age ranges from 35 to 40 years with a male predominance.3,4 and 5 Data from Edinburgh suggest carpal fractures have a type A fracture curve with a bimodal distribution of younger males and older females.2 Only 7.7% of carpal fractures occur at ≥65 years of age and 1.5% in those ≥80 years of age.2 Alsawadi and Stanton reviewed the available epidemiological literature to determine the characteristics of scaphoid fractures in patients over 70 years of age and found the incidence in the literature ranged from 0.2 to 14 per 100,000 adult individuals per year.6 Previously published data from Edinburgh found there were 9 (total 151) fractures in patients over 70 years of age with an incidence of 12.9 per 100,000 adult individuals per year (Figure 27.1).7
Scaphoid and triquetral fractures make up more than 90% of all fractures of the carpus.3,4 and 5 Triquetral fractures are the second most common carpal fracture3,4 and 5 and commonly occur in an older population, with a mean age of 51 years and a type A fracture distribution curve. Fractures of the scaphoid, trapezium, hamate and pisiform occur at a mean age ranging from 29 to 43 years, the male predominance is 66–100% and a type B fracture distribution curve is seen (unimodal younger male).2 Studies have found that risk factors for a scaphoid fracture are youth and male gender.5,7,8
Hey et al. reported that 7% of patients sustain multiple carpal fractures, with almost 50% a perilunate fracture-dislocation.5 Fracture-dislocations are twice as common as a perilunate dislocation and displace dorsally in 97% of cases.9 Data from Edinburgh reported that perilunate dislocations have an incidence of 0.5 per 100,000 adult individuals per year, with a male predominance and occur in the younger patient with a mean age of 26 years.10 None were found in those ≥65 years of age. Open carpal fractures are known to be very rare.5,11
Mechanism of injury
Carpal fractures and dislocations are routinely secondary to an axial compression force to the wrist that results in hyperextension, causing shear forces across the dorsal structures and exerting tension to the palmar wrist structures.12,13 and 14 A fall from standing height onto the outstretched hand accounts for almost two-thirds of all injuries, with high energy mechanisms less common and more frequently seen in males, e.g. sports, assault and motor vehicle collision.3,4 and 5 As would be expected, high energy injuries are a risk factor for sustaining an associated injury with a carpal fracture, for example, a perilunate dislocation or fracture-dislocation.5,7 Hook of hamate fractures occur with racket sports and golf related injuries, while body or coronal fractures often occur in young men following a punch injury.15,16 It is proposed that carpal instability results from a high energy force to the wrist associated with hyperextension, ulnar deviation and intercarpal supination.12,17
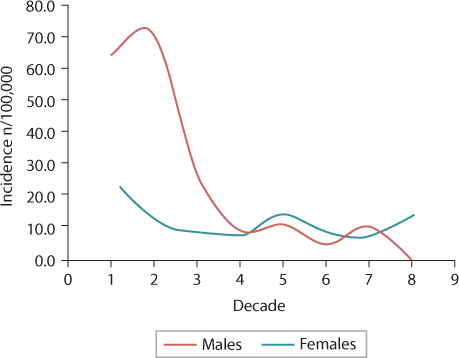
Figure 27.1 The incidence of scaphoid fractures in Edinburgh, 2007–2008. (Adapted from Duckworth AD, et al. J Trauma Acute Care Surg 2012;72(2):E41–5.)
CLASSIFICATION
Scaphoid fractures
Although there are numerous classifications for a fracture of the scaphoid, a constant criticism is that there is a lack of consideration given to the significant associated soft tissue injuries potentially seen. Furthermore, it is unknown whether these classifications are applicable to the assessment and management of the elderly patient.
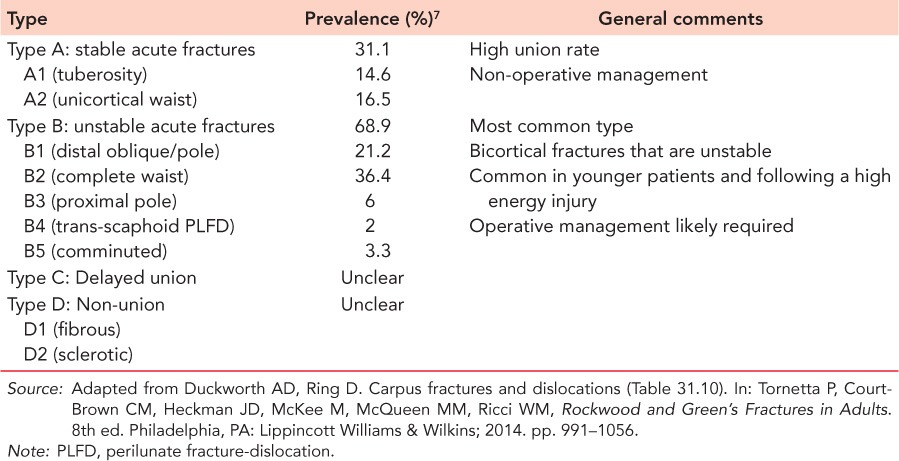
One of the most commonly employed classifications within the literature is the Herbert and Fisher classification (Table 27.1),18 which aims to identify the fracture types that require fixation. Other classifications include the:
AO/OTA classification,19,20 which divides fractures into location (distal pole, waist, proximal pole) and comminution
Russe classification,21 which uses the inclination of the fracture line to guide the risk of fracture instability
Mayo classification,22,23 which sets out criteria aimed at predicting instability and guiding management and includes fracture malalignment, >1 mm of fracture displacement,24,25 proximal pole fracture, perilunate fracture-dislocation, bone loss and/or comminution, a lateral intrascaphoid angle of >35 degrees and/or a dorsal intercalated segment instability (DISI) deformity.26
Table 27.1 The Herbert and Fisher scaphoid fracture classification
SCAPHOID NON-UNION
The Herbert and Fisher classification (Table 27.1)18 defines two types of scaphoid non-union:
Type D1: fibrous non-union, often with minimal deformity, symptoms and signs variable, risk of wrist arthritis small
Type D2: established sclerotic non-union, unstable, progressive (often humpback) deformity leading to SNAC.27
Lunate fractures and Kienböck’s disease
Acute fractures of the lunate were classified into five groups by Teisen and Hjarback28 according to the involvement of the palmar or dorsal pole, the body of the lunate and the character of the fracture, for example, horn avulsion, transverse, frontal or transarticular. Avulsion fractures frequently occur in the radial corner and body fractures are frequently transverse in the coronal plane.
Kienböck’s disease is the idiopathic avascular necrosis (AVN) of the lunate,29,30 which can sometimes be mistaken for a fracture on radiographs. Some have suggested that neglected lunate fractures29,30 or ischaemia following a perilunate dislocation or fracture-dislocation26 result in Kienböck’s, while others postulate that venous congestion is responsible.31 The Lichtman classification divides Kienböck’s disease into four stages with an aim to help guide treatment32:
No changes on plain radiographs
Increased density of the lunate
Lunate collapse ± fragmentation (subdivided according to position of scaphoid)
Radiocarpal arthritis
Carpal ligament injuries
The three systems commonly used for describing carpal instability are inherently related and can be useful in understanding the mechanism of injury and the treatment necessary. They can involve purely ligamentous, or ligamentous and bony pathologies. The three systems are:
Intercalated segment instability33,34 was originally described by Linscheid et al.33 and this system is based on the position of the lunate and related intercalated segment on standard lateral radiographs of the wrist:
DISI with lunate extension and capitate displacement dorsally:
Scapholunate angle >60 degrees, capitolunate and radiolunate angle >15 degrees
Causes – Scapholunate dissociation (SLD) and displaced scaphoid fractures
Volar intercalated segment instability (VISI) with lunate flexion and capitate displacement volarly (less common):
Scapholunate angle <30 degrees, capitolunate angle >30 degrees and radiolunate angle >15 degrees in volar direction
Causes – Lunotriquetral dissociation and complex multi-ligamentous disruption
Static versus dynamic35:
Static: Carpal instability is apparent on standard non-stressed radiographs of the wrist and is associated with multiple ligament disruption.
Dynamic: Carpal instability is apparent on stress testing and stress radiographs, with normal routine radiographs.
Dissociative versus non-dissociative (can be combined):
Dissociative instability results from an isolated injury to a major intrinsic ligament of the carpus, for example, scapholunate disruption or scaphoid fracture.36,37 and 38
Non-dissociative instability occurs when there is an injury between the carpal rows, that is, extrinsic ligament injury, for example, radiocarpal instability, Barton fracture-dislocation.38
SCAPHOLUNATE DISSOCIATION
SLD is the most common carpal ligament injury and involves a range of injuries to the scapholunate interosseous ligament, from simple sprains to scaphoid dislocation. Injury to the ligament results in dyskinesia between the scaphoid and lunate articulation, leading to progressive widening of the joint over time.39 Any classification system for SLD needs to consider the chronicity of the injury and whether it is a static or dynamic instability. Static scapholunate instability is often defined as the characteristic increase in the scapholunate gap and a scapholunate angle of greater than 60 degrees in a non-loaded wrist.40 Geissler et al. classified four grades of ligament injury based upon arthroscopic assessment41:
Ligament in continuity with normal carpal alignment but attenuated (midcarpal space) – non-operative management
Carpal malalignment (midcarpal space) – arthroscopic reduction and fixation
Carpal malalignment (both carpal spaces) with a 1 mm (probe) gap between bones – arthroscopy ± open reduction and fixation
Carpal malalignment (both carpal spaces), unstable with 2.7 mm scope passable between bones – open reduction internal fixation (ORIF)
An alternative classification by Kuo and Wolfe42,43 classifies the disruption into occult, dynamic, complete SLD, DISI deformity and a SLAC (scapholunate advanced collapse) wrist with an aim to guide management.
LUNATOTRIQUETRAL DISSOCIATION
Lunatotriquetral dissociation (LTD) is often stable and is less common than SLD.44 It includes:
Ligament sprains
Partial or complete ligament injury
Part of perilunate injury
Ulnocarpal impingement
Triangular fibrocartilage complex (TFCC) injury
Although LTD is not normally associated with degenerative changes over time, carpal kinematics are affected and a VISI deformity can occur, with chronic ulnar-sided wrist pain a cause of notable disability.45 It has been suggested that concomitant injury to the dorsal radiotriquetral ligament or palmar ulnocarpal ligaments needs to occur before a severe fixed deformity results.46
PERILUNATE DISLOCATIONS AND FRACTURE-DISLOCATIONS
These rare but devastating injuries are commonly classified according to the Mayfield classification and in terms of the greater (fracture-dislocation) or lesser (dislocation) arc injury patterns,12,17,47 with a dorsal trans-scaphoid perilunate fracture-dislocation most common.9,48,49 Lesser-arc perilunate dislocations are a pure ligamentous disruption around the lunate, while a greater-arc injury involves ligamentous injuries with an associated fracture of one or more of the bones around the lunate. Injury to the ligaments around the lunate normally starts radially and propagates to the ulnar side, with the distal row displaced in a dorsal or dorso-radial direction.26 Alternate classifications are the Witvoet and Allieu50 and Herzberg et al.9 classification systems. The Mayfield classification breaks the injury down into four stages according to the carpal keystone (the lunate)12,51:
Scaphoid fracture and/or SLD
Lunocapitate disruption
Lunotriquetral disruption
Perilunate dislocation
ANATOMICAL CONSIDERATIONS
Two rows of eight bones make up the carpus, with the proximal row including the scaphoid, lunate and triquetrum. The distal row is made up of the trapezium, trapezoid, capitate, hamate and pisiform. The proximal carpal row is known as the key intercalated segment, bridging between the bones of the forearm and the distal row of the carpus and the metacarpals33,52,53 and 54 which delivers movement, congruency and force transmission at the wrist joint.26,55,56 The intrinsic and extrinsic ligaments of the wrist are essential to allowing a degree of movement while maintaining stability.35,55,56 The intrinsic ligaments connect individual carpal bones to one another, while the extrinsic ligaments connect the carpal bones to the forearm bones and the metacarpals.26 Defining these ligaments can be difficult clinically as they often merge with the articular surface and capsule of the wrist, and a recent review of 58 anatomical studies found that all but one of the carpal ligaments are not described consistently.57
The oval ring theory53,58 considers the proximal intercalated segment, the variable geometry of the carpus with the lunate at the keystone that is anchored by interosseous ligaments to the scaphoid (radially) and triquetrum (ulnarly),33,52,53 and 54,59 along with the synchronous and reciprocating motion of the proximal and distal rows.26 The older and alternative columnar theory first put forward by Navarro breaks the carpus into radial (scaphoid, trapezium and trapezoid), central (lunate, capitate and hamate) and ulnar (triquetrum and pisiform) columns.60 Although this concept aids with the understanding of load transmission in the wrist, it is limited when considering the concept of synchronous motion.26
Neurovascular supply
The carpus is innervated by the anterior and posterior interosseous nerves, with the blood supply coming from intraosseous and extraosseous vessels from the dorsal and palmar vascular systems.61,62 An understanding of the vasculature of the carpus is essential when considering the risks of non-union and AVN, particularly when attempting to preserve the blood supply during surgical approaches to the wrist. As the blood supply to the carpus is thought to enter distally, this leaves the proximal carpal row vulnerable to an interruption of blood supply and potentially AVN.61,62 The risk of AVN is increased due to the single vessel supply of the scaphoid, capitate and 20% of the lunate, while the trapezoid and about half of all hamates do not have an intraosseous anastomosis.61,62 and 63,26 The risk of scaphoid AVN and non-union is associated with the predominantly retrograde blood supply from soft tissue attachments that supply two vascular pedicles originating from the scaphoid branches of the radial artery.26,61,64 Although the vasculature to the lunate is potentially compromised when performing a dorsal approach to the wrist, this is limited by the concurrent supply from the palmar radiocarpal arch.26
Operative anatomy: scaphoid
The scaphoid is located within the wrist joint at a 45-degree angle to the longitudinal and horizontal axes of the wrist.26 The ligamentous attachments are primarily found on the non-articular dorso-radial surface.26,57,65 For the volar approach to the scaphoid, an incision is made in line with the flexor carpi radialis (FCR) tendon from proximal to the scaphoid and extending approximately 5 cm across the transverse wrist crease to just distal to the distal pole of the scaphoid and is about 5 cm in length.26 The FCR is mobilized in an ulnar direction and the superficial radial artery is retracted. The wrist capsule should now be visible and is cut along the line of the scaphoid, with care taken to preserve as much of the radioscaphocapitate ligament as possible.
An open dorsal approach to the scaphoid is normally used for fractures of the proximal pole66 and utilizes a straight 3–4 cm incision over the dorsum of the wrist at the level of the scapholunate.26 The extensor pollicis longus (EPL) is normally left alone and the dorsal wrist capsule is then incised, with care taken throughout to preserve the dorsal ridge vasculature.
CLINICAL ASSESSMENT
A clear history is important when assessing carpal injuries as untreated fractures can present late with an established non-union, particularly with regard to the scaphoid. Wrist pain is the primary presenting feature of carpal fractures and dislocations. It is noted that the most reliable sign of carpal injury is well-localized tenderness, for example, injury to the scaphoid often presents with radial sided wrist pain and tenderness in the anatomical snuffbox (ASB).26,67 Associated swelling and ecchymosis of the carpus, with a reduced range of movement, is sometimes found in the acute phase following injury. A general guide suggests ligament injuries can be acute (within a month of injury), subacute (1–6 months after injury) or chronic (>6 months after injury) and is important when considering treatment options.
Injuries associated with carpal instability and/or dislocation may present with an obvious deformity to the wrist. Other potential signs of ligament instability include an audible click or clunk on moving/stressing the wrist and diminished strength with repetitive grip strength testing.26 Assessment of the contralateral wrist can be helpful, particularly in elderly patients who present with long-standing problems associated with instability. Although associated with poor diagnostic performance characteristics due to their infrequency, Table 27.2 presents some of the special tests that can be used in the diagnosis of carpal ligament injuries.
Although open injuries are exceedingly rare, assessment of the skin should always be carried out in the elderly patient. Distal neurovascular status should be assessed and documented, which is of particular importance following a dislocation or fracture-dislocation to the carpus. Anything from 15–50% of perilunate injuries will have symptoms and signs of median neuropathy,69 although ulnar neuropathy, arterial injury and/or tendon injury do occur.9,48 In the elderly patient, chronic presentations may be seen and these will likely present with increasing problems with nerve compression or tendon rupture.70 Tendon ruptures can also occur with a chronic presentation of a hamate fracture, for example, little finger flexor,71,72 while a lesion of the deep branch of the ulnar nerve can occur following a hook of hamate fracture or pisiform fracture.15,73,74
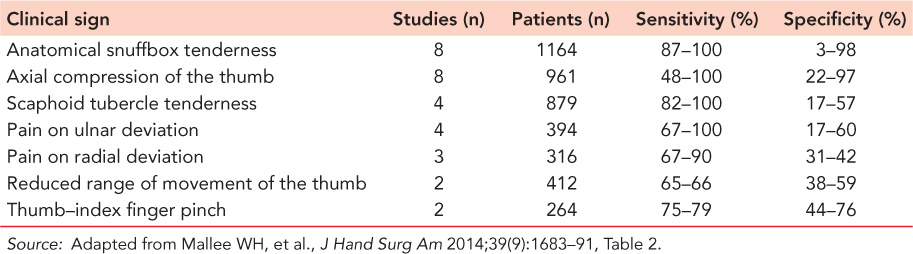
Scaphoid fractures
There continue to be numerous studies analysing the diagnostic performance characteristics of the various clinical signs employed in the diagnosis of scaphoid fractures, as no single sign has been reported to be sufficiently sensitive and specific.26,75,76 The literature initially reported the diagnostic performance characteristics of individual clinical signs,77 as well as subsequently documenting the change in these characteristics when clinical signs are combined.75 Mallee et al. reported the results of a systematic review and meta-analysis of 13 studies analysing 25 different clinical tests for a suspected fracture of the scaphoid and found that ASB tenderness was the most sensitive of the clinical signs but with poor specificity that results in the over-treatment of a number of patients.78 Other high-sensitivity tests were axial compression of the thumb, scaphoid tubercle tenderness and ASB pain on ulnar deviation of the wrist (Table 27.3). There are an insufficient number of scaphoid fractures in the elderly to determine if comparable results would be found in the older population.
Recent studies have attempted to develop clinical prediction rules combing demographic and clinical characteristics predictive of a true fracture.79,80 A recent large prospective study of 223 confirmed and suspected scaphoid fractures reported that that the strongest predictor of a true scaphoid fracture within 72 hours of injury was the absence of ASB pain on ulnar deviation of the wrist and pain on thumb–index finger pinch, with scaphoid tubercle tenderness most predictive at approximately 2 weeks post injury.80
Table 27.2 Clinical signs used in the detection of carpal fractures and carpal instability
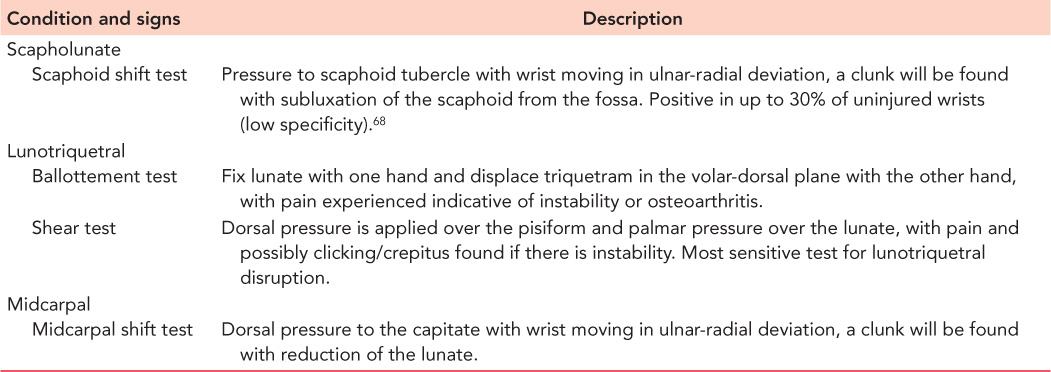
Table 27.3 The sensitivity and specificity for various clinical signs as determined by Mallee et al. for suspected fractures of the scaphoid
IMAGING
Standard four view radiographs of the scaphoid will identify the vast majority of carpal injuries and static instability of the wrist.81,82 These are:
Neutral posteroanterior (PA)
Lateral
45-Degree radial oblique (supinated anteroposterior [AP])
45-Degree ulnar oblique (pronated AP)
Important radiographic signs that can aid in the detection of carpal fractures and carpal instability are found in Table 27.4. PA and lateral views are useful in the assessment of fractures and fracture-dislocations of the carpus, as well as for determining carpal alignment and/or collapse (Figures 27.2 and 27.3). The neutral PA view is limited in the diagnosis of26:
Scaphoid fractures due to the overhang of the tubercle82,83
Triquetral avulsion fractures secondary to the normal superimposition of the lunate dorsal lip
Lunate fractures due to the palmar cortical line of the radial styloid
For suspected fractures of the scaphoid, the Ziter view, and carpal box or tunnel views can be helpful given that up to 30–40% of scaphoid fractures are not diagnosed on primary assessment and investigation with four view radiographs.14,26,81,84 An oblique pronated lateral view will move the triquetrum dorsal to the lunate and aid with diagnosis of triquetral fractures.85 Carpal tunnel views can aid in the diagnosis of tuberosity fractures of the trapezium,86 hamate hook fractures87,88 and pisiform fractures.87 The standard lateral view is useful for assessment of displacement and head rotation for fractures of the capitate. Trapezoid fractures, particularly coronal fractures, are rarely detected on standard plain radiographs89 and further imaging is used in more than 80% of cases.89 Always be sure to exclude a perilunate dislocation or fracture-dislocation as the evidence would indicate that 16–25% of perilunate injuries are initially missed,9,90,91 particularly the lesser-arc injury, commonly due to the lack of a bony injury and often the inexperience of the initial assessor (Figure 27.4). Delay in the management of these injuries is associated pain, stiffness, carpal tunnel syndrome and secondary osteoarthritis.9,90,91
Additional views that can help detect carpal ligament instability are flexion-extension and radio-ulnar stress views, and clenched fist views.38 Some would also advocate comparative radiographs of the contralateral uninjured wrist.92 It is important to assess the intercarpal, carpometacarpal and radiocarpal joint spaces, particularly on the neutral PA view and stress views as indicated. Although the normal distance is debated, a normal space is said to be ≤2 mm, with ligament disruption diagnostic at >5 mm (Figure 27.3).
Standard four view radiographs can be used in the assessment of carpal fracture displacement regarding step-off, translation, rotation and angulation.23 The lateral view is of particular importance (Table 27.4). Despite only moderate interobserver reliability reported using this technique,93,94 and 95 the prevalence of displacement and instability is low and it would seem sensible that in the elderly patient with no gapping or translation at the fracture site and no lunate dorsal angulation, further imaging is rarely required.
Advanced imaging
Advanced imaging is predominantly used for the diagnosis of suspected scaphoid fractures, assessing fracture displacement, and in the diagnosis of ligamentous injuries to the wrist. The need for such imaging in the elderly patient will likely be limited to displaced carpal fractures, symptomatic carpal instability and the assessment of symptomatic non-unions. The most commonly employed modalities include ultrasound, bone scintigraphy, CT, MRI and wrist arthroscopy. Fluoroscopy using stress manoeuvres is advocated by some for suspected ligamentous disruption,96,97 with arthrography very limited due to the high false positive and false negative rate.98,99
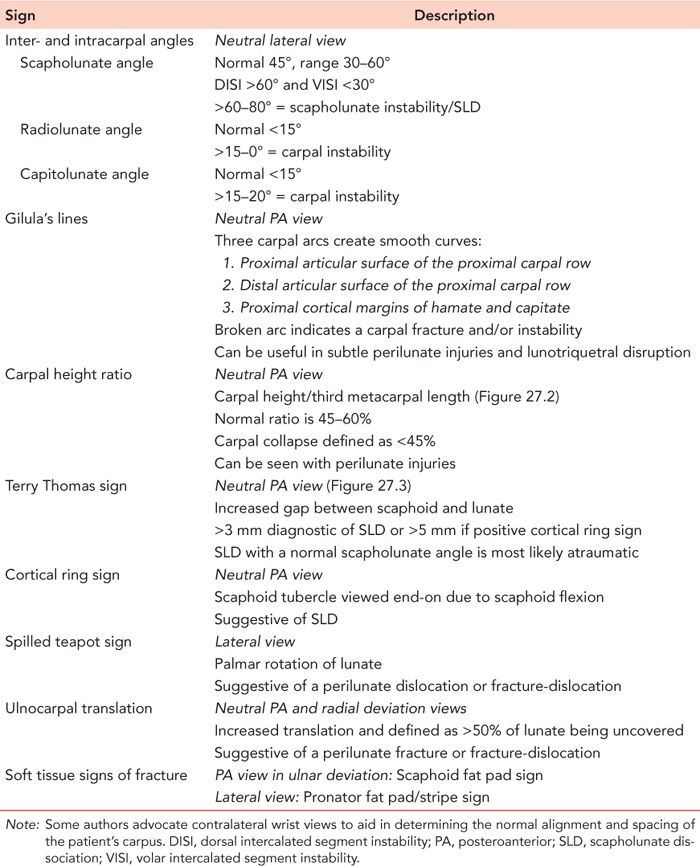
Table 27.4 Plain radiographic signs used in the detection of carpal fractures and carpal instability
The efficacy and necessity of the use of these imaging modalities in the elderly patient, particularly for the suspected scaphoid fracture, is unknown. Furthermore, there are two key issues regarding the interpretation of diagnostic performance characteristics for the various imaging modalities available for suspected scaphoid fractures. The first is the low prevalence of true scaphoid fractures among suspected fractures (5–20%), which dramatically lowers the probability that a positive test will correspond with a true fracture as false positives are nearly as common as true positives.8,14,26,100
A proposed solution to this is the use of clinical prediction rules, which have been documented to effectively guide patient management throughout medicine.101,102 The development and use of such rules for the suspected scaphoid fracture, including a combination of demographic and clinical risk factors, could potentially increase the prevalence of true fractures among suspected fractures.103,104 This would result in the use of advanced secondary imaging in higher risk patients, which may improve the diagnostic performance characteristics currently reported. The substantial influence of clinical prediction rules on the probability of a suspected scaphoid fracture has been already demonstrated in studies from Holland79 and Edinburgh.80 The second issue is the lack of a consensus reference standard for confirming a fracture,105,106 which means that an alternative method for calculating diagnostic performance characteristics (latent class analysis) is required.78,107

Figure 27.2 Carpal height ratio (L2/L1).

Figure 27.3 Terry Thomas sign with widening of the scapholunate distance, indicative of scapholunate dissociation.
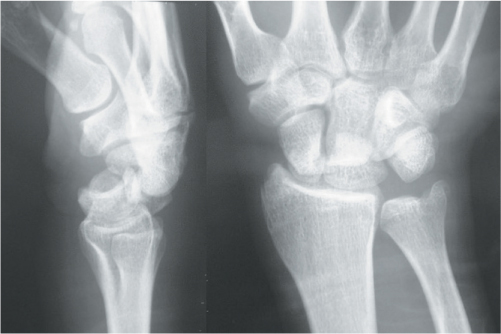
Figure 27.4 A trans-scaphoid perilunate fracture–dislocation of the carpus, with obvious disruption of Gilula’s lines on the posteroanterior view (see Table 27.4).
Ultrasound
Ultrasound can be used in the diagnosis of suspected scaphoid fractures and ligament injuries.26 It is non-invasive and inexpensive but is operator dependent. It has lower diagnostic performance characteristics than the other available methods when diagnosing a suspected scaphoid fracture, with sensitivity ranging from 37% to 93% and specificity ranging from 61% to 91%.8,108,109 and 110
Bone scintigraphy
Bone scintigraphy is used in the diagnosis of suspected carpal fractures and avulsion injuries.26 There are authors who advocate the use of bone scintigraphy for the suspected scaphoid fracture.111,112 However, it is felt by many that use is limited given the lower specificity when compared to both CT and MRI.113,114,115 and 116 This was recently confirmed in a Cochrane meta-analysis of six studies (11 studies in total) that reported a sensitivity of 99% but a specificity of 86% (Table 27.5).117
Computed tomography
CT is used in the diagnosis of suspected carpal fractures, for determining fracture displacement, and in the diagnosis of carpal malunion and non-union, and dynamic CT is used by some for determining the presence of ligamentous injuries.26,118,119 Scaphoid fracture displacement can be assessed on CT imaging using the lateral intrascaphoid angle, the AP intrascaphoid angle, the dorsal cortical angle and the scaphoid height to length ratio.120,121 The recent Cochrane review mentioned above analysed four studies to determine the diagnostic performance characteristics of CT for suspected scaphoid fractures and reported the lowest sensitivity at 72%, but with a specificity of 99% (Table 27.5).117 Studies have reported that CT is superior to standard radiographs for the diagnosis of scaphoid fracture displacement,122,123 with a step of ≥1 mm at the dorsal or radial cortices and a gap of ≥1 mm on sagittal or coronal views quoted.24,25
Table 27.5 The sensitivity and specificity for various imaging modalities as determined by Mallee et al. for suspected fractures of the scaphoid
Imaging modality (number of studies assessed) | Sensitivity (%) | Specificity (%) |
|---|---|---|
Bone scintigraphy (n = 6) | 99 | 86 |
CT (n = 4) | 72 | 99 |
MRI (n = 5) | 88 | 100 |
Source: Adapted from Mallee et al. Cochrane Database Syst Rev 2015;6:CD010023.
Magnetic resonance imaging
MRI is used for suspected carpal fractures, the diagnosis of AVN of the carpus and diagnosing ligamentous injuries.26 It is suggested by some that MRI is the gold standard investigation for suspected scaphoid fractures, with practical limitations including limited access and cost efficiency.8,116,124,125 Furthermore, given all these imaging modalities are being used in low prevalence situations such as the suspected scaphoid fracture, the positive predictive value of these tests is lower than expected and false positive MRI scans in healthy individuals have been reported in one study.103,126 Mallee et al. in their Cochrane review analysed five studies to determine the diagnostic performance characteristics of MRI for suspected scaphoid fractures and reported a sensitivity of 88% and the highest specificity at 100% (Table 27.5).117
WRIST ARTHROSCOPY
Wrist arthroscopy can be used in the diagnosis of suspected scaphoid fractures and fracture displacement, the assessment and management of non-union, as well as for determining the presence and grade of carpal ligamentous injuries and associated degenerative changes in the wrist.127,128,129 and 130 It is generally agreed that arthroscopy is the reference standard for diagnosing carpal ligament injuries. Buijze et al. reported on 58 consecutive scaphoid fractures that were managed with arthroscopy assisted operative fracture fixation and found a significant correlation between radiographic comminution and displacement, and instability found at the time of surgery.131 Use in the elderly patient is limited.
Associated injuries
Much of the literature regarding associated injuries is in relation to fractures of the scaphoid and it is not known if associated injuries are more common in elderly patients. Approximately 1 in 10 of all scaphoid fractures has a related injury and are associated with a high energy mechanism of injury.7,132 Almost 80% of associated upper limb fractures are of the proximal or distal radius. Radial head fractures are most commonly found,7,132 with distal radius fractures, perilunate dislocations and trans-scaphoid perilunate fracture-dislocations also seen.5,7
The literature has reported an increasing incidence of concomitant ligamentous injuries using wrist arthroscopy,133 although the clinical relevance of these injuries is unknown. An associated distal radius fracture can be indicative of a ligamentous injury and potential carpal instability.134 Hamate fractures or fracture-dislocations have been reported to be associated with a fracture of the metacarpals.135 Almost 25% of perilunate dislocations or fracture-dislocations will be seen in a multiply injured patient, with approximately 10% having a concomitant upper limb injury.9
TREATMENT
In the elderly patient, the aims of management for all carpal fractures and dislocations are to achieve a functional and stable wrist with minimal associated complications. Given that the vast majority of the carpal fractures and dislocations occur in younger patients, there is a scarcity of literature in relation to the elderly patient. As with all elderly trauma, the treatment choice should consider the clinical assessment of the patient and the complexity of the injury, but primarily should consider the baseline functional status and the pre-existing medical comorbidities of the patient, as well as the risks attached to any suggested surgery. Management options include non-operative, ORIF, fracture excision and fusion.
Non-operative
SCAPHOID FRACTURES
For suspected fractures of the scaphoid there are advocates for repeated clinical examination and radiographs at 10–14 days post injury, while others recommended early advanced imaging for example, CT or MRI, despite the potential issues with this. As has already been discussed, a few authors have promoted the use of clinical prediction rules that combine demographic and clinical risk factors that could target advanced secondary imaging in higher risk patients.79,80 Whatever pathway is employed, and pending the diagnosis being confirmed or refuted, a below elbow forearm cast (with or without thumb immobilization) or wrist splint with thumb immobilization is routinely applied.
Good results can be expected with the non-operative treatment of tubercle fractures of the scaphoid as they are normally benign avulsion fractures (Figure 27.5).136,137 and 138 There are advocates for a wrist splint for 1 month followed by mobilization, while others favour casting. Fractures managed without immobilization have been found to be associated with displacement and a fibrous union but are not associated with disability.139
For non-displaced or minimally displaced waist fractures (Figure 27.6) that are stable, non-operative management will attain a union rate of 95–99%,140 has a 3–20% rate of displacement while in cast,141,142 and is certainly seen by some as the management of choice for these injuries,136,137 and 138 particularly in the elderly patient. There are several systematic reviews and meta-analysis that have not found early surgery for these fractures to be superior to non-operative management.138,143,144 and 145

Figure 27.5 An oblique radiograph of the wrist demonstrating a displaced scaphoid tubercle fracture in a 72-year-old woman.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








