Thirty bones compose the foot and ankle complex. (This number includes the distal tibia and fibula and the two sesamoids at the first metatarsophalangeal joint.) The previous chapter described the expected radiographic appearance of each bone in the many views available. However, variations in their appearance are not uncommon. Variations typically are incidental findings and asymptomatic, although symptomatology or pathology may occur secondary to a skeletal variation. More common examples of the latter include the accessory navicular and tarsal coalition.
Several words are frequently used when referring to variations of the skeleton. Their definitions are as follows (from Dorland’s Illustrated Medical Dictionary1):
Accessory: supplementary to another similar and generally important thing.
Anomaly: marked deviation from the normal standard, especially as a result of congenital defects.
Os: bone; a general term that is qualified by the appropriate adjective to designate a specific type of bony structure or a specific segment of the skeleton.
Ossicle: a small bone.
Partite: having parts or divisions.
Sesamoid: a small, nodular bone embedded in a tendon or joint capsule.
Supernumerary: in excess of the regular or normal number.
Synostosis: the osseous union of two bones that are normally distinct.
Variant: something that differs in some characteristic from the class to which it belongs, as a variant of a disease, trait, and so forth.
The terms partite, supernumerary, and accessory bone in the following discourse are differentiated thus: Partite can pertain to either a normally existing bone or an accessory bone that is subdivided; supernumerary pertains to anomalous duplication of a normally existing bone; and accessory bone refers to those ossicles (not anomalous duplication) that are found in addition to the normally existing bones. Also note that although all sesamoid bones are ossicles, not all ossicles are sesamoid bones.
Variations can be expressed in several ways (Box 6-1). Examples of variations involving normally existing bones include variants of number, position, form (shape and size), density, and architecture. Accessory ossicles, in addition to the existing 30 bones, are not uncommon.
Variants of number include partite bones, supernumerary bones, and absence of bones. Bipartite sesamoids, for example, are common. Although rare, bipartite medial cuneiform and navicular bones may be encountered. Supernumerary bones include duplication of phalanges, metatarsals, and tarsal bones.
BOX 6-1 Expression of Variants in the Foot
Variations Involving Normally Existing Bones
Variants of number
Variants of position
Variants of form
Variants of density
Variants of architecture
Accessory ossicles
The axis of each bone has a characteristic position relative to the axes of adjacent bones. In the two-dimensional radiograph, this position can vary considerably among patients and depends heavily on foot type and the degree of pronation or supination during weight-bearing stance in angle and base of gait.2 Variations of position can predispose for future pathology.
Most variations of existing bones are variants of form. Variants of form concern the girth, length, and contour of a bone. Synostosis/coalition is also a variation of form. Other variants of form can be attributed to the position of the foot or ankle bones relative to each other and/or the image receptor. For example, the navicular bone frequently appears rectangular in a pes cavus foot but wedge shaped in a pes planus foot. Varying forms may also be encountered in weight-bearing studies secondary to pronation and supination (internal and external leg rotation, respectively; refer to Figure 5-1). Angle and base of gait positioning provide a means for minimizing the technical variation that may occur (described in Chapter 4). Positional changes are predictable, however, and the experienced interpreter can recognize these alterations and correlate them to normal radiographic anatomy.
Variants of density can mimic abnormal or pathologic processes. More commonly, this appears as a relative radiolucency or decreased density. Occasionally, focal areas of increased density are seen.
Each bone has its own characteristic shadows. These shadows represent cortex, trabeculae, and superimposed osseous landmarks in the adult skeleton and constitute the architecture of the bone. The outer margin of the bone is its external architecture, and the remainder is its internal architecture. Most architectural variants relate to the appearance of cortical bone and trabeculae. Variation of an osseous landmark’s superimposed shadow may correlate to variant size, shape, or position of that landmark.
Variations of the existing 30 bones are not the only variants one may encounter. Numerous accessory bones are commonly found in the foot and ankle. One may be an isolated finding or multiple ossicles can occur throughout both extremities.
Appreciation of normal radiographic anatomy and the summation of shadows concept (Chapters 5 and 9, respectively) are the first steps of image interpretation. The interpreter must then become familiar with the numerous variations of normal. Many of these variants appear unilaterally and can mimic fractures or other pathology. Bilateral studies, therefore, are not always useful for their differentiation and can be misleading. Furthermore, even if they are bilateral, they may be asymmetric in appearance. The purpose of this chapter is to present the gamut of radiologic variants that one may encounter in the adult foot and ankle.
VARIANTS OF NUMBER
Partite Sesamoids at the First Metatarsophalangeal Joint
It is common to see partite tibial and fibular sesamoids; they are typically bipartite. Partitioning may involve one or both sesamoids and be unilateral or bilateral. And, when bilateral, symmetry is not the rule.3 For example, if only the tibial sesamoid is partite in one foot, only the fibular sesamoid may be partite in the opposite foot. The tibial sesamoid is more commonly partite than the fibular sesamoid.4 The presentations (partitioning, shape, size, and number) are extremely variable and follow no specific patterns. For example, a bipartition may divide the sesamoid into equal or unequal halves; the division can be transverse (most common, Figure 6-1A), oblique, or, least common, longitudinal (Figure 6-1B).
It can be difficult to differentiate a fractured sesamoid from a partite sesamoid,5 especially in the dorsoplantar (DP) view. The presence of jagged edges alone is not a useful distinguishing feature, because both the bipartite and the fractured sesamoid can appear to have jagged edges. For example, a partite sesamoid that is complicated by degenerative joint disease has spurs that give the appearance of a jagged edge, similar to that of a fracture. More commonly, the prominent primary trabeculations that are normally seen in the first metatarsal distal metaphysis are superimposed on the sesamoids; these shadows can exaggerate the perception of a jagged fracture line. Nor can fracture be determined by the amount of separation between the two segments. It is not uncommon to see apparent “distraction” in the asymptomatic, untraumatized bipartition. Fracture is best differentiated from variant bipartition with the sesamoid isolated, that is, with no superimposition on the metatarsal head (this can only be accomplished with the sesamoid axial and lateral oblique or modified non–weight-bearing lateral—or Causton—views). Certainly correlation with clinical history is important in these instances. Bone scintigraphy and magnetic resonance imaging (MRI) may be valuable adjunctive studies for further differentiation of partition versus fracture versus symptomatic partition.
The sesamoids are initially evaluated with the dorsoplantar and sesamoid axial views. The lateral oblique view is valuable for assessing tibial sesamoid pathology (Figure 6-1C).6 The tibial and fibular sesamoids are superimposed on the first and second metatarsals, respectively, in the medial oblique view; this view generally does not provide any additional information apart from the dorsoplantar, lateral oblique, and axial views. The weight-bearing lateral view is useless for imaging the sesamoids; they are superimposed on each other in addition to other metatarsal and phalangeal bones.

FIGURE 6-1. Bipartite tibial sesamoid. A: Transverse partition. B: Longitudinal partition. C: Lateral oblique view for evaluating tibial sesamoid.
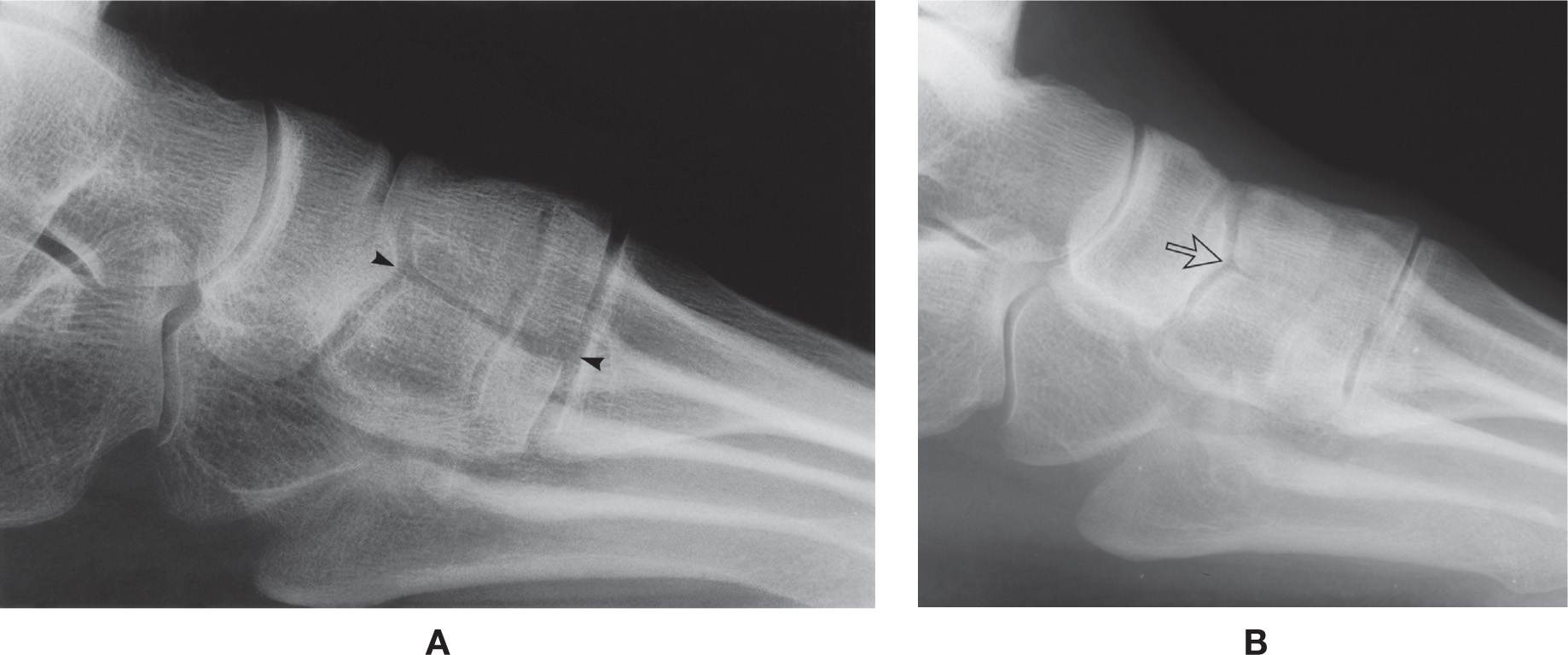
FIGURE 6-2. Bipartite medial cuneiform. A: Complete partition (arrowheads). B: Incomplete partition posteriorly (arrow).
Bipartite Medial Cuneiform (Os Cuneiforme I Bipartitum)
In rare instances, the medial cuneiform presents as two bones in the adult skeleton, a variant known as the bipartite medial cuneiform. They are more frequently found bilaterally and predominate in males.7 The partition classically divides the bone into upper and lower halves and is best seen in the lateral view (Figure 6-2A).
The classic bipartition, when present, is easily overlooked. It is fully superimposed on the remaining cuneiform bones and easily mistaken for other bone shadows. However, the transverse joint space identified in the center of the medial cuneiform is its characteristic radiologic feature. This arthrodial joint space typically is complete from anterior to posterior. Midfoot/arch pain may be associated with this entity.8,9
A variation may be encountered where the bipartition is incomplete. The medial cuneiform may be incompletely divided into two segments at its anterior and/or posterior margins but is “fused” centrally. Indentations are seen along the articular surfaces (Figure 6-2B).
Bipartite Navicular (Müller–Weiss Syndrome)
The few cases that have been reported as the bipartite navicular mimic a disorder referred to as Müller–Weiss syndrome. Interestingly, there is minimal to no overlap between these two entities when reported in the literature; in other words, reports of the bipartite navicular rarely mention Müller–Weiss syndrome, and vice versa. Are they the same, or not?
Müller–Weiss syndrome, which appears to occur spontaneously in the adult navicular, is of unknown etiology. The deformed navicular resembles osteonecrosis on MRI; however, most histopathologic studies have not been able to provide conclusive evidence of osteonecrosis.10 This syndrome is usually bilateral and occurs predominantly in females in their fourth to sixth decades.11 Bipartite navicular is also of unknown etiology, though some feel it may be a congenital anomaly.
Maceira and Rochera12 have presented a large cohort of cases; they propose that Müller–Weiss syndrome is related to delayed ossification of the navicular that becomes deformed secondary to abnormal force distribution on the bone. They have grouped the radiographic presentations of increasing deformity into five stages for didactic purposes, which, as Brailsford13 noted in 1939, are chronic and progressive. Generally speaking, stage 1 is a normal radiograph, with the talar axis bisecting the navicular and medial cuneiform bones; between stages 2 and 4, the talar axis moves superiorly then inferiorly, and the navicular bone fragments and subluxates off the talar head; in stage 5, there is greater subluxation, even dislocation of the navicular fragments such that the lateral and intermediate cuneiforms appear to articulate with the talar head. Ultimately, the progression of deformity results in osteoarthritis of the talonavicular joint.14
Classically, the division or partition separates the bone into a smaller superolateral segment and a larger inferomedial segment.15 Bipartite navicular, which appears similar to (or, is the same as) the “stage 3” Müller–Weiss syndrome, appears as follows: in the dorsoplantar view, the larger navicular segment has been described as being is shaped like a wedge15 or comma12 with its base medially and apex pointing laterally; the smaller segment is superimposed on the lateral cuneiform and cuboid (Figure 6-3A).
In the lateral view, the smaller segment is wedge-shaped, positioned along the dorsal aspect of the larger segment; its apex is directed inferiorly (Figure 6-3B).16 The smaller bipartite segment appears closely associated, possibly articulating, with the intermediate cuneiform superoposteriorly.
Computed tomography (CT) is valuable for confirming the navicular’s bipartite nature.17
Supernumerary Bones
Anomalous duplication of a bone is rare (Figure 6-4). The phalanges are most frequently affected. Metatarsal duplication is usually incomplete or dwarfed unless accompanied by tarsal duplication.
Absence of Normally Existing Bones
On rare occasion one or several normally existing bones may be absent. The absence of a single bone may not be obvious clinically and is identified incidentally with radiographs; primary examples include absence of the tibial or fibular sesamoid18 and absence of a lesser toe middle phalanx (Figure 6-5A,B). Absence of a sesamoid and aphalangia may be either bilateral or unilateral. Neither is associated with symptomatology. In contrast, anomalous absence of multiple bones can present with gross deformity. A classic example is the so-called claw or lobster foot (Figure 6-5C).
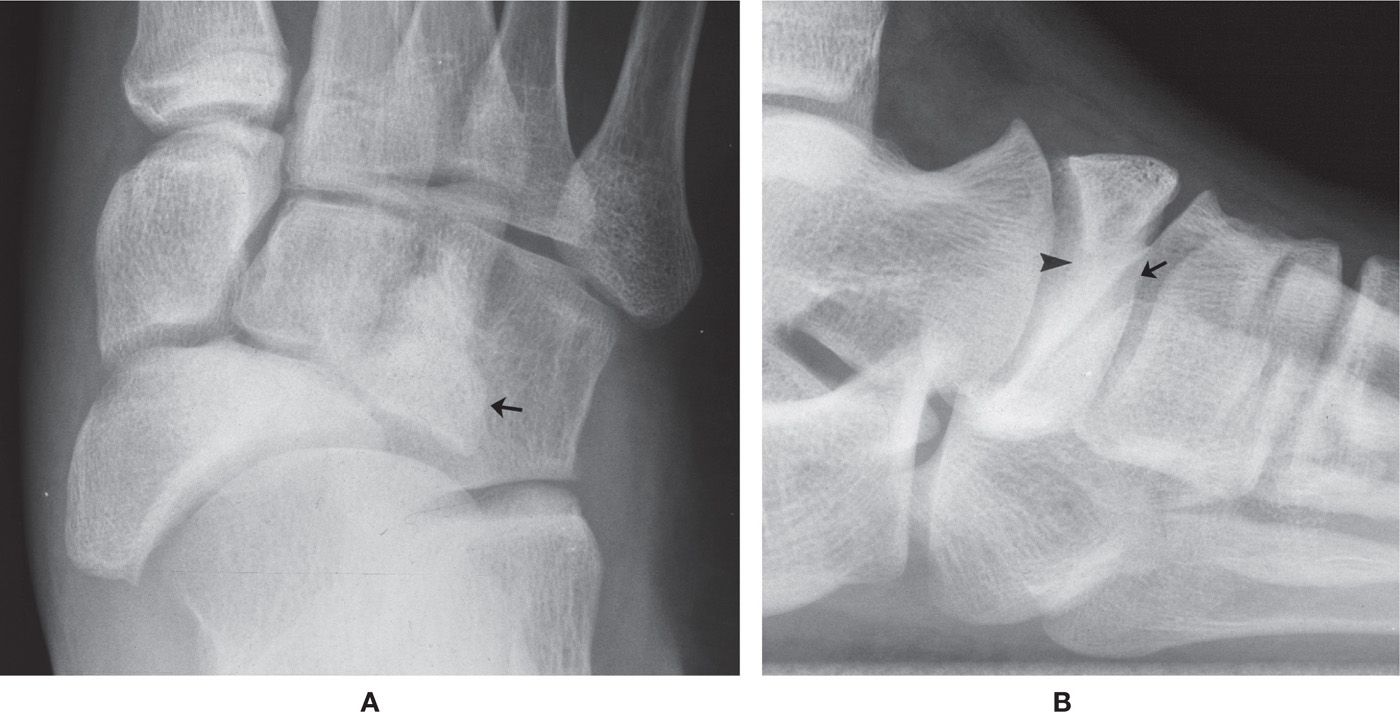
FIGURE 6-3. Bipartite navicular. A: DP view: comma-shaped larger medial segment; the arrow identifies the smaller superolateral segment. Also note the medial subluxation of navicular relative to talar head. B: Lateral view: partition is not clearly seen (arrowhead); odd presentation of the lateral cuneiform-navicular articulation (straight arrow).

FIGURE 6-4. Supernumerary bones. A: Duplicate distal and middle phalanges, second toe (a unilateral finding). B: Duplicate hallux (a unilateral finding). C: Duplicate fifth metatarsal and toe (a bilateral finding).
VARIANTS OF POSITION
Each bone has a characteristic position in the foot and ankle. This is best assessed in the dorsoplantar and lateral views with the foot bearing weight in its angle and base of gait. The axis of any particular bone lies at a particular position relative to other bones. All three anatomic planes should be considered when evaluating position. Unfortunately, with two-dimensional radiographs it is difficult to fully appreciate position in all planes. The frontal plane position of most foot bones cannot be directly evaluated radiographically; assessment, therefore, requires logical analysis and reasoning while looking at both the dorsoplantar (transverse plane) and lateral (sagittal plane) views.
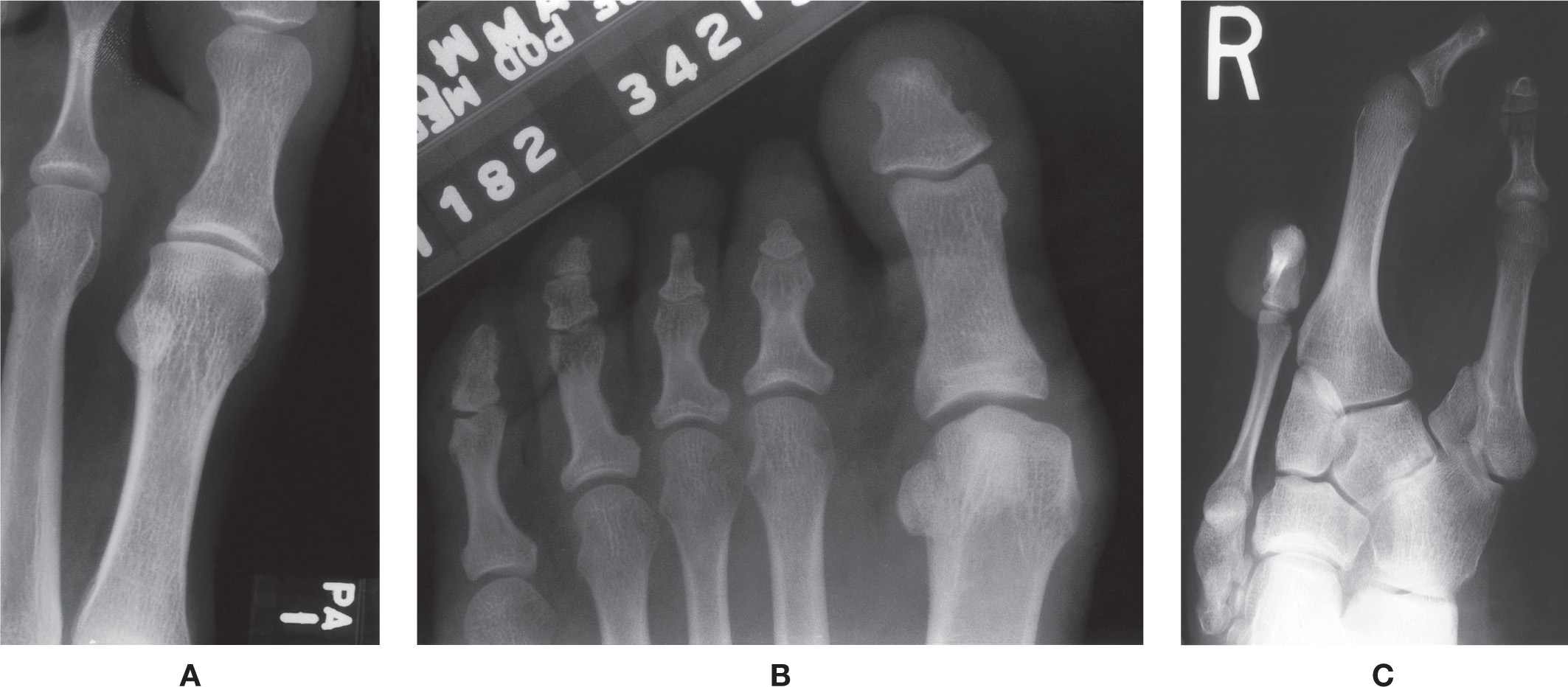
FIGURE 6-5. Absent normally existing bones. A: Tibial sesamoid (a bilateral finding). B: Middle phalanges (a unilateral finding). C: Cuneiforms, metatarsals, and toes (a bilateral finding).
Position variants predispose the patient to future symptomatology and pathology. Normal and abnormal position of foot bones, including foot structure, and their relationships to biomechanics, are discussed in Section 4 (Chapters 12 and 13).
VARIANTS OF FORM
Distal Phalanx
Variations of the ungual tuberosity may be encountered in the dorsoplantar view. Its entire outer margin may be irregular or spiculated (Figure 6-6), simulating the reaction associated with inflammatory processes (e.g., chronic nail infection or psoriatic arthritis). Another variation is absence of the medial or lateral margin; absence of both margins simulates the whittling of bone associated with forefoot neuropathic arthropathy. Occasionally, the entire ungual tuberosity may be absent or appear atrophic. In a lesser toe, for example, the distal phalanx may appear triangular.

FIGURE 6-6. Varying presentation of the ungual tuberosity. Multiple distal indentations (arrowheads). (Also note the enlarged basal inferomedial tubercle, the superimposed sclerotic anterior aspect of the flexor tuberosity, and an os interphalangeus.)
Spur formation is occasionally seen along the posteroinferior, medial, and lateral margins of the ungual tuberosity. It will be seen in the dorsoplantar and lateral views. The lateral interosseous ligaments insert along these margins.19,20 A spur may be seen superiorly in the lateral view; this “mechanical” subungual spur may be related to hallux limitus.21
Occasionally, variation of the length or girth of a distal phalanx is encountered. The phalanx may be increased or decreased in length or girth. Increased girth can many times be attributed to the flexor tuberosity that may be enlarged or hypertrophied (Figure 6-7A,B). This is best identified in the isolated hallux lateral view. A wavy contour that mimics a periosteal reaction is infrequently seen along the shaft’s medial and lateral margins (Figure 6-7C). “Whiskering” (small spurs along the diaphysis) may also be seen as a normal variation that is suggestive of psoriatic arthritis.
Variations of the hallucal distal phalanx base may also be encountered. The size of the basal inferomedial tubercle, for example, varies considerably, ranging from absent to large radiographically (Figures 6-8 and 6-6, respectively). A recent investigation of this bony excrescence proposes that it probably represents a reaction of normal bone to repeated forces occurring during gait.22 The lateral interosseous ligaments that run between the base and ungual tuberosity originate from the inferomedial and inferolateral basal tubercles. It infrequently calcifies, and spur formation may be noted at the entheses.
Occasionally, variation of the lesser toe distal phalanx base is seen. The base commonly flares medially and laterally in the dorsoplantar view. Often it appears quite pronounced relative to the narrow shaft. In rare instances, the lateral aspect of the hallux distal phalanx base appears absent.

FIGURE 6-7. Varying presentations of the distal phalanx shaft. A: Enlarged flexor tuberosity (lateral view). B: Enlarged flexor tuberosity (dorsoplantar view, a bilateral finding). C: Wavy medial and lateral margins mimicking periosteal reaction (a bilateral finding).
Middle Phalanx
The shape of the lesser toe middle phalanx may be either square or rectangular. The margins of a rectangular middle phalanx may appear either flat or indented (concave). The head of a middle phalanx occasionally is angulated laterally relative to its shaft, resulting in angulation of its respective distal phalanx (Figure 6-9).
Proximal Phalanx
The proximal phalanx is a short, tubular bone. Variations in its length and girth are frequently encountered. For example, the phalanx may be shorter in length and wider in girth. This variant more frequently affects the lesser toes (Figure 6-10), although it also can involve the hallux. In contrast, a decreased diaphyseal girth may be seen. One example is the spool-shaped proximal phalanx.23 The medullary canal may even appear obliterated in exaggerated cases.
Occasionally, a proximal phalanx head is enlarged. This finding primarily involves the fifth digit and usually accompanies the clinical presence of an adductovarus contracture with a heloma durum overlying the hypertrophied head. A small exostosis may be seen along the head’s superolateral aspect. A remnant of the phalangeal cleft (a variant of normal development) may be identified in a similar location. Rarely, the hallux proximal phalanx head is enlarged.
A wavy contour and associated increased girth are commonly encountered along the medial and lateral margins of a lesser toe’s diaphysis (Figure 6-11A); this corresponds to the diaphyseal ridge, which may be misinterpreted as a periosteal reaction. Its size varies considerably, and it may or may not be seen on all lesser digit proximal phalanges of the same patient. Two structures insert along the diaphyseal ridge: the wing of the extensor hood apparatus and the fibrous flexor sheath. Rotation of the digit obscures its visualization. A different type of cortical thickening and irregular contour is infrequently seen along the medial and/or lateral margins of the hallux proximal phalangeal distal diametaphysis (Figure 6-11B).

FIGURE 6-8. Varying presentation of the distal phalanx base: Absent tubercles (a bilateral finding). Compare to the enlarged tubercle in Figure 6-6.
Sesamoids
The size of a sesamoid bone is fairly constant, although infrequently an enlarged or atrophic sesamoid may be encountered. The two sesamoids are equal in size in approximately 50% of the time; the tibial sesamoid is larger in 35%, the fibular in 15%.4 They typically have smooth and regular margins. Occasionally, however, small protuberances resembling spurs may be seen along their posterolateral margins in the absence of any degenerative process or enthesopathy elsewhere. Rarely, a sesamoid may be much smaller than normally expected and when compared to its mate (Figure 6-12). Coalition of the two sesamoids has been reported.24
Metatarsals
Metatarsals have a characteristic length pattern in the dorsoplantar view (Figure 6-13A). Typically, the anterior end of the second metatarsal is most distal, followed by the first and third metatarsals (the anterior ends of the latter two bones are nearly at the same position distally). The anterior end of the fourth metatarsal is more proximal relative to the third metatarsal, and the fifth is most proximal. Many variations are encountered regarding the lengths of each metatarsal relative to one another, some appearing longer and others shorter than the normal pattern described earlier (Figure 6-13B). The short fourth metatarsal is typically anomalous.

FIGURE 6-9. Varying presentation of the middle phalanx. Lateral aspect of second toe middle phalanx is significantly shorter than the medial aspect, resulting in angulation of the distal phalanx laterally. Note also the square middle phalanges of the third and fourth toes.

FIGURE 6-10. Short proximal phalanx third and fourth toes (a bilateral finding).

FIGURE 6-11. Varying presentations of the proximal phalanx shaft. A: Phalangeal ridge (arrowheads, second, third, and fourth toes). B: Increased girth along the anterior aspect of the medial shaft (arrow) simulating a periosteal reaction. Present bilaterally.

FIGURE 6-12. Varying presentation of the sesamoids: Smaller tibial sesamoid (bilateral).
The first metatarsal head can have varying presentations. The shape of the distal articular surface may be round (most common), be flat, or demonstrate a central ridge (Figure 6-14A,B). The medial and superior aspects of the first metatarsal head vary in size and can be quite enlarged and hypertrophied. An enlarged tubercle may be seen medially at the diametaphyseal margin. The superolateral tubercle is occasionally seen along the superior aspect of the first metatarsal neck in the lateral view (Figure 6-14C).
Regarding the lesser metatarsals, the head may (rarely) be flat distally with associated increased girth. The tubercles along the superomedial and superolateral aspects of their heads can be hypertrophied and prominent, visible in the medial oblique and dorsoplantar views, respectively. The neck’s girth is consequently increased laterally when the superolateral tubercle is enlarged (Figure 6-15A), and may simulate an old, healed fracture. The anatomic groove located between each tubercle and the anterior articular surface may be exaggerated in radiographic appearance (Figure 6-15B). The posteroinferior articular extensions of the lesser metatarsal heads may be pronounced in size; this finding, although superimposed, will be identified in the dorsoplantar view (Figure 6-15C). A lesser metatarsal head may bow or angulate medially relative to the shaft, which is typically symmetrical and bilateral.
Variations of the girth, contour, and form of a metatarsal shaft are encountered. The girth, for example, may be increased (Figure 6-16A) or decreased. Infrequently, a metatarsal shaft is overtubulated (over constricted) and appears extremely narrow (Figure 6-16B). Anatomic variations have been described that would correspond to this radiographic presentation.25 Increased girth of a metatarsal shaft may be secondary to Wolff’s law (increased stresses result in bone formation and remodeling). An example is the enlarged second metatarsal shaft associated with a short first metatarsal (also known as the Morton’s foot).26 Occasionally, the cortex along the inferolateral aspect of the first metatarsal shaft proximally appears thickened. This site correlates anatomically to the insertion of the peroneus longus tendon. Lateral bowing of a metatarsal, especially the fifth, will be also seen. Increased girth of the fifth metatarsal midshaft medially may accompany this finding and is symmetric bilaterally (Figure 6-16C).

FIGURE 6-13. Variation of metatarsal length. A: Normal. B: Short second metatarsal.
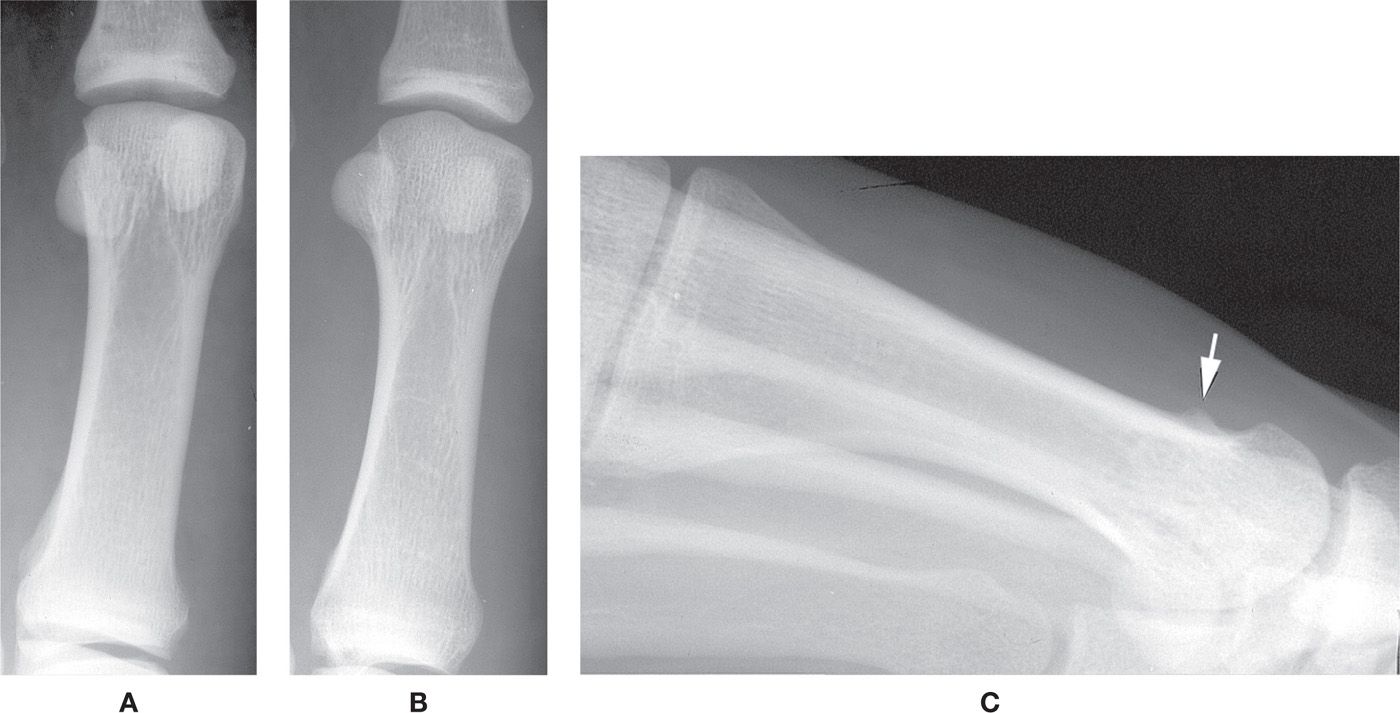
FIGURE 6-14. Varying presentations of the first metatarsal head. A: Flat. B: Combined flat/ridge. (For comparison, an example of the round metatarsal head is seen in Figure 6-13B.) C: Prominent lateral tubercle (arrow).
Along the margins of the metatarsal bases variations may be seen that could be mistaken for pathology. The medial and lateral aspects of the lesser metatarsal bases normally are irregular; this finding is exaggerated by a deep groove located along the inferior and anterior aspects of the articular facet for the adjacent metatarsal. It is especially evident along the lateral aspects of the second-, third-, and fourth metatarsal bases (Figure 6-17A). A pronounced articulation is occasionally seen between the bases of the first and second metatarsals (Figure 6-17B); the articulations between the lesser metatarsal bases are rarely visible. A tubercle may be found, along the first metatarsal base medially, which provides insertion for the tibialis anterior tendon (Figure 6-17C). Another tubercle might be seen superiorly. The size of the fifth metatarsal tuberosity is variable. It may appear absent, elongated posteriorly, or project laterally.
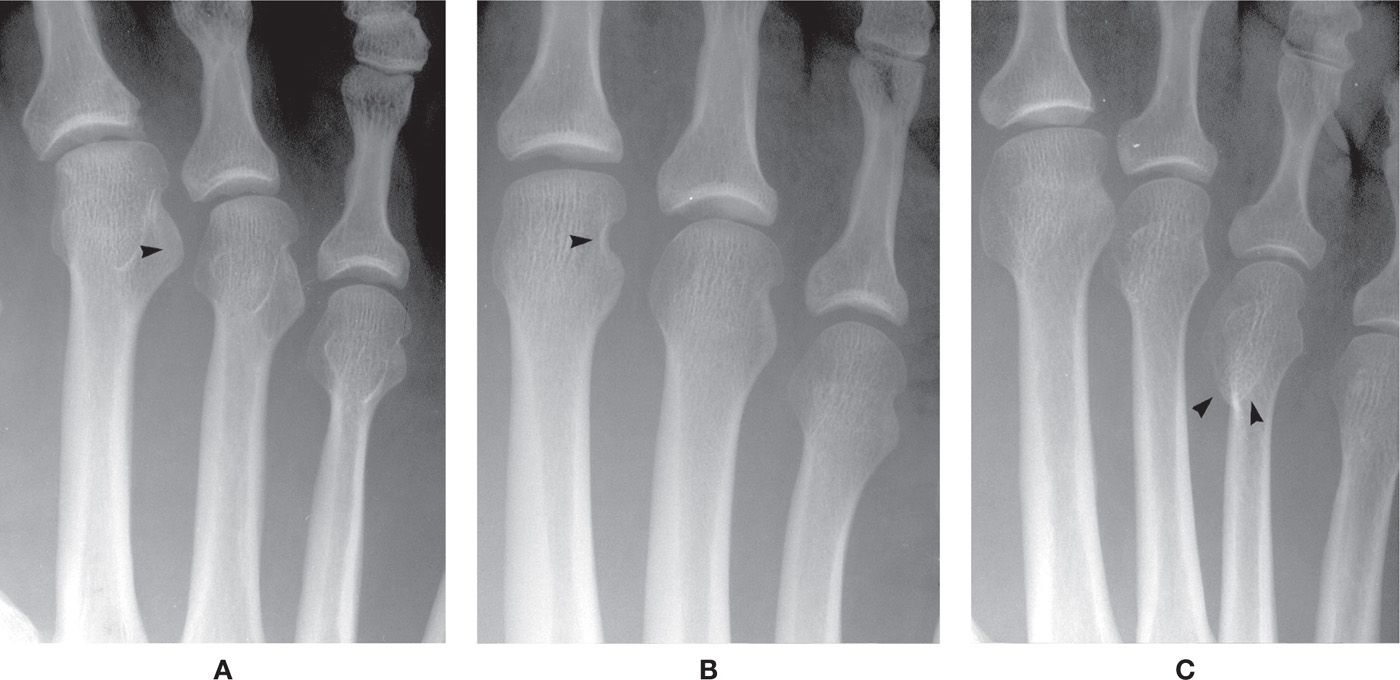
FIGURE 6-15. Varying presentations of the lesser metatarsal heads. A: Enlarged superolateral tubercle (arrowhead), second metatarsal (a bilateral finding). B: Exaggerated notch between superolateral tubercle and anterior articular surface (arrowhead), second metatarsal (a bilateral finding). C: Enlarged and elongated plantar-medial condyle (arrowheads), fourth metatarsal.
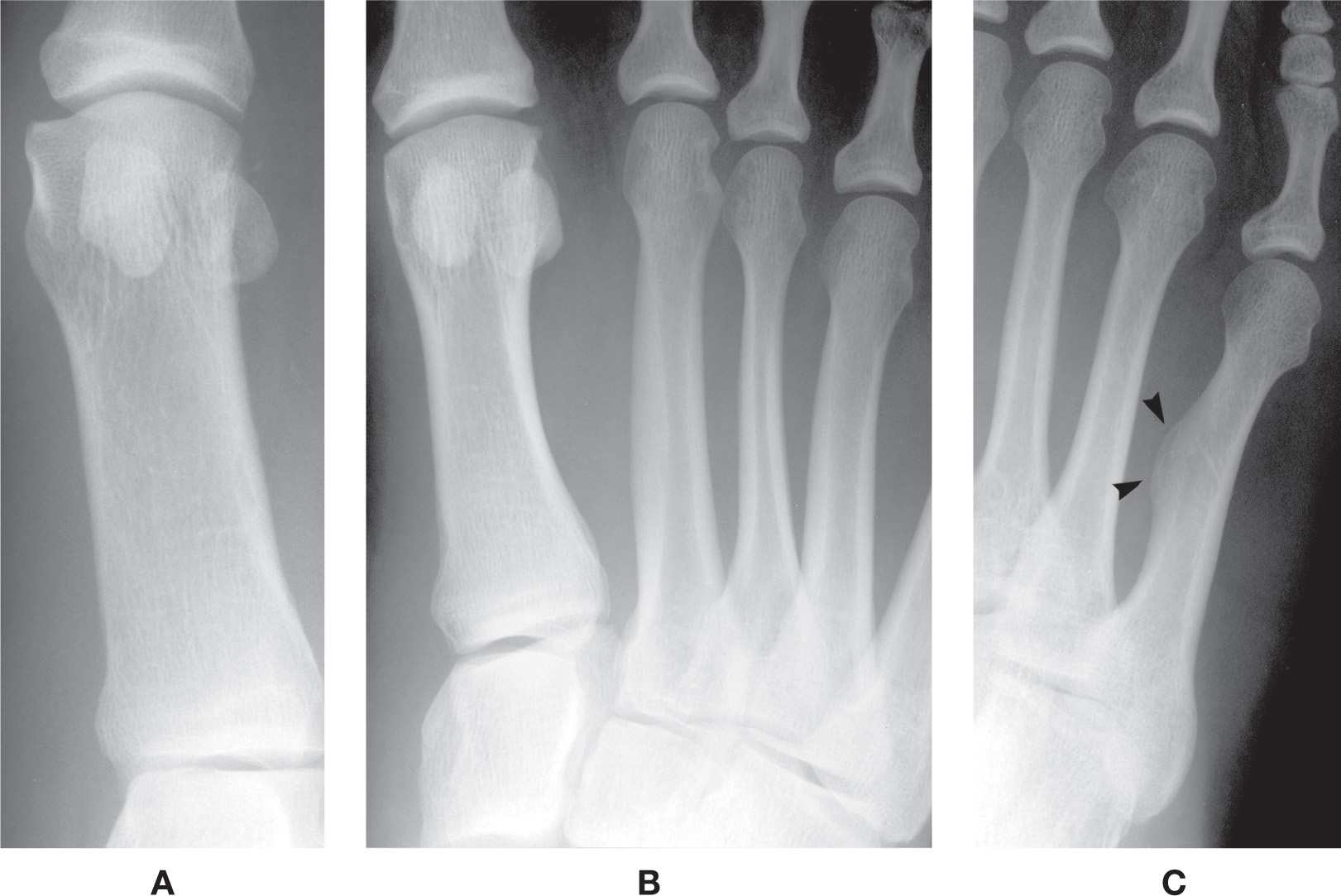
FIGURE 6-16. Metatarsal variants of form. A: Increased girth (first metatarsal). B: Decreased girth third metatarsal, increased girth second metatarsal. C: Fifth metatarsal bowing with cortical thickening (arrowheads). A variant of density, radiolucency of the fifth metatarsal head medially, is also seen.
Variant articular surface shapes can also be encountered in the DP view. The cuneiform articular surface of the first metatarsal base may be flat or even concave. Occasionally, the lateral cuneiform articular surface of the third metatarsal is also concave, but, in most cases, it cannot be clearly identified because adjacent structures are superimposed.
Cuneiforms, Cuboid, and Navicular
Variability regarding the shape or form of the medial cuneiform is primarily positional in nature, but its form along the medial surface can vary. (The complete and incomplete bipartite medial cuneiforms are discussed earlier in the sub-section Variants of Number.) One specific variant finding not related to position is a tubercle along the medial surface seen in the dorsoplantar view (Figure 6-18). The size of this tubercle varies, from small to large, and its position is inferomedial and typically situated closer to the first metatarsal articular surface, although it can also appear more posteriorly. It probably provides a gliding surface or “guide” for the tibialis anterior tendon, similar in function to the peroneal tubercle for the peroneal tendon.
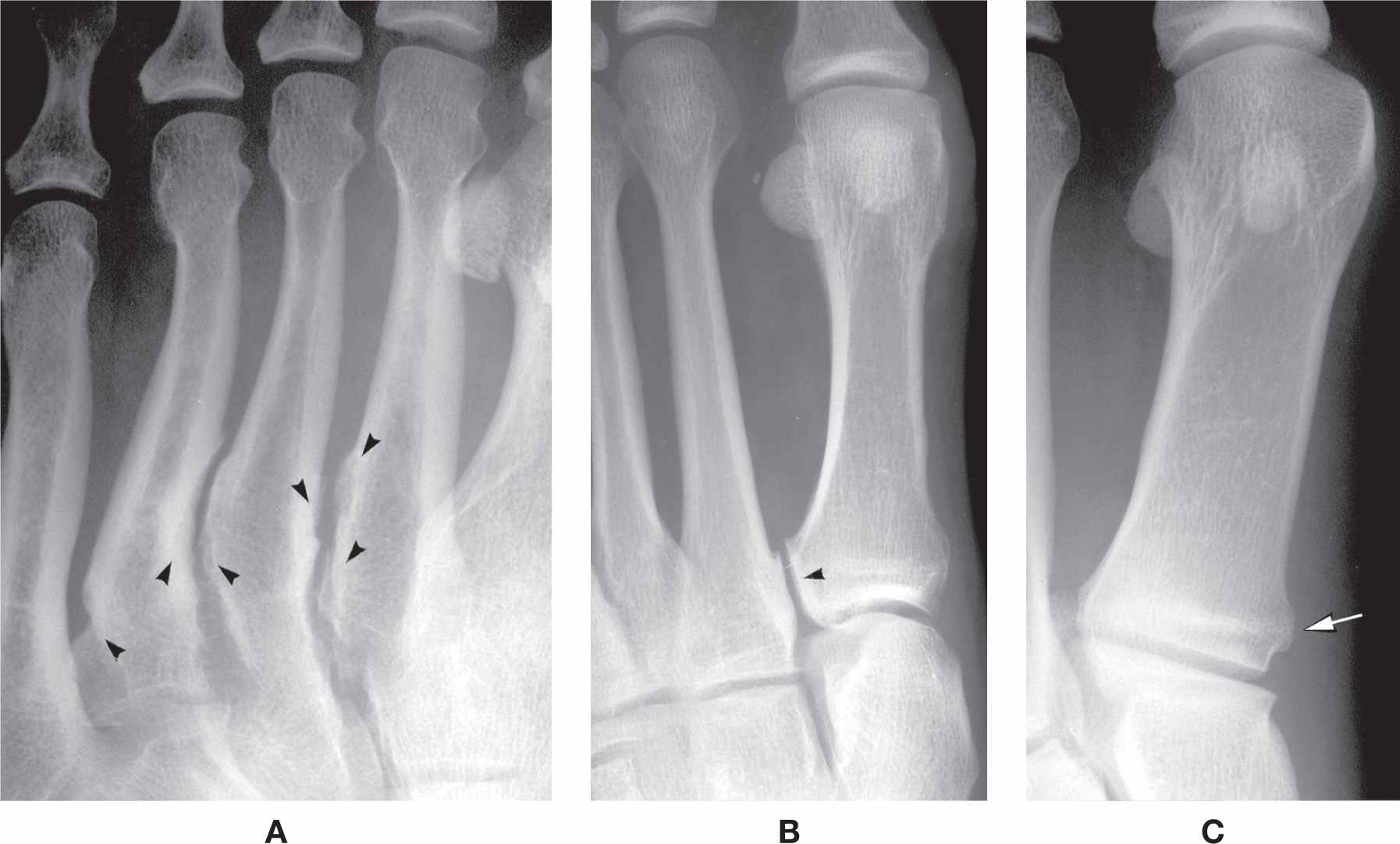
FIGURE 6-17. Varying presentations of the metatarsal base. A: Exaggerated, irregular intermetatarsal surfaces (arrowheads) between bases and proximal shafts (a bilateral finding). B: Articulation between first- and second metatarsal bases (arrowhead) (a bilateral finding). C: Tubercle for tibialis anterior tendon insertion (arrow) (a bilateral finding).

FIGURE 6-18. Tubercle along the medial surface of the medial cuneiform (arrowhead).
Superimposition of the midfoot bones is normally seen in the dorsoplantar view. This could lead to the misdiagnosis of a cubocuneiform coalition. Although trabeculations appear continuous between the two bones, the superimposed shadows of their articular margins can still be identified. This latter finding would not be seen if it were a true coalition.
The cuboid has few variations to note. Its combined articular surface for the fourth and fifth metatarsals is typically flat or nearly flat; infrequently, it has a prominent triangular ridge centrally separating the two articular surfaces, best seen in the medial oblique view (Figure 6-19). The anteromedial corner of the cuboid frequently juts medially toward the cuneiform, simulating an osteophyte or spur.
Most variants of navicular form are identified along its medial margin in the dorsoplantar or lateral oblique views. The navicular occasionally appears wedge-shaped (its lateral half is narrow relative to the larger medial half in the dorsoplantar view), although it more frequently is somewhat rectangular. The tuberosity may be large, small, or absent in some individuals. When the tuberosity is elongated, it appears to wrap around the talar head. The elongated tuberosity may be related to a fused accessory navicular ossification center (see sub-section Accessory Navicular). A large tubercle is infrequently seen along the navicular medial surface anterior to the tuberosity (Figure 6-20). In yet other patients, the tuberosity may have an anomalous location medially; it classically is situated posteromedially. The medial margin of the navicular’s medial cuneiform articular surface may be pronounced and extend anteriorly. A similar spurlike extension may be seen in the lateral view projecting anteriorly along the intermediate cuneiform articular surface. Variant form of the navicular simulating a bipartite navicular may be associated with a pronounced superoanterior margin. Finally, a tubercle may be visible in the medial oblique view for the cuboid articular surface.

FIGURE 6-19. Cuboid variant of form: Ridge separating fourth- and fifth metatarsal articulating surfaces (arrowhead).

FIGURE 6-20. Navicular variants of form: Tubercle along medial surface anterior to the tuberosity (arrow).
Talus
The talus is best isolated in the lateral view. Its form is fairly consistent; however, occasionally it varies. The neck, for example, may be short or elongated. Less frequently, the body may appear flattened and the head/neck enlarged. Rarely, the head appears flattened.
Spurs are frequently seen along the superior aspect of the talar head or neck. Anatomically, a small ridge is normally present along the superior surface at the junction of the talar head and neck that parallels the navicular articular surface; the talonavicular and talotibial joint capsules and ligaments insert here.27 This ridge may be enlarged as a variation of normal (Figure 6-21). A spur is frequently identified on the talar head that is continuous with the navicular articular surface; this is an osteophyte, a feature of talonavicular joint osteoarthritis, and is found in association with limited range of tarsal joint motion. However, its formation may be related to a prior injury.

FIGURE 6-21. Prominent ridge along the talar head/neck superiorly (arrowhead).
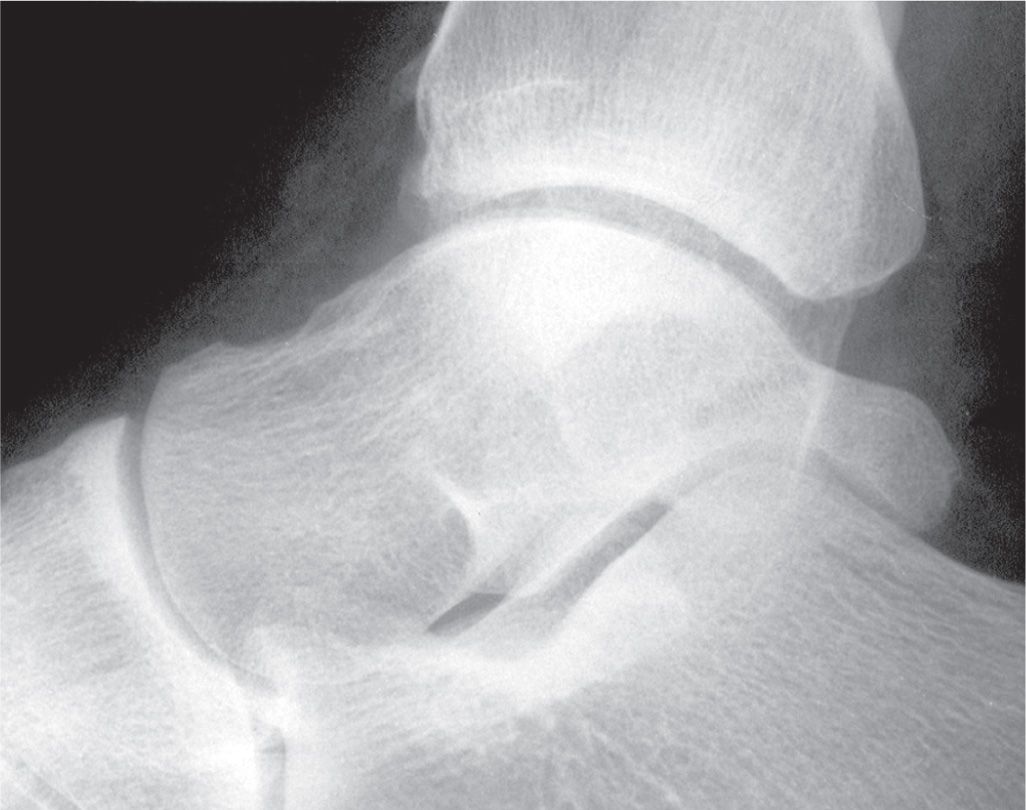
FIGURE 6-22. Variant of talar posterolateral process: Prominent trigonal process.
The talar posterolateral process is continuous with the tibial articular surface of the talar dome in the lateral view and presents as a small protuberance. The process may be elongated and extend posteriorly. This has also been referred to as the trigonal process or Stieda’s process and probably represents a fused accessory ossification center (Figure 6-22) (see sub-section Os Trigonum).
The talar dome normally has a semicircular outline in the lateral view. If the ankle joint axis is not positioned perpendicular to the x-ray image receptor, however, the medial and lateral shoulders of the dome are not aligned and give the appearance of a flattened talar dome (Figure 6-23). This appearance usually is positional in nature and is seen with a supinated/cavus foot in the weight-bearing lateral view.

FIGURE 6-23. The appearance of this “flattened” talar dome is purely positional in nature. Note that the fibular malleolus (F) is posterior in position relative to the tibial malleolus (T).
Calcaneus
The form of the calcaneus is fairly constant. However, occasionally, the overall shape appears somewhat rectangular and/or expanded, with distortion of its normal distinctive curves and lines. For example, the calcaneal length may appear elongated or foreshortened, the latter being the result of an enlarged posterior segment (Figure 6-24). Localized hypertrophy of the bursal projection (the posterosuperior aspect of the calcaneus) may or may not be associated with clinical symptomatology (Haglund disease and/or retrocalcaneal bursitis). The inferior surface rarely appears perfectly flat (Figure 6-25). The anterior process may be enlarged and extend superiorly in the lateral view in the presence or absence of a calcaneonavicular coalition (Figure 6-26).
A projection of bone is rarely seen along the medial aspect of the calcaneus in the ankle anteroposterior view. This variation articulates with an extension from the talar medial process and has been called the “assimilated os sustentaculum tali” because of its location. Anatomically, it is found along the posterior aspect of the sustentaculum tali. It may be identified as a bony palpable protuberance clinically and has been associated with symptomatology.28 This probably represents an extra-articular talocalcaneal coalition (see discussion of synostosis and coalition later in this chapter).
The tubercles and tuberosities are occasionally enlarged and prominent. An enlarged peroneal tubercle or retrotrochlear eminence is infrequently seen along the lateral calcaneal body in the dorsoplantar and calcaneal axial views (Figures 6-27A,B).29 The anterior tuberosity may also be enlarged (Figure 6-27C). Occasionally, the lateral tubercle may appear hook-shaped with a foramen, probably the result of variant development (Figure 6-27D).
Radiographically, the middle and anterior articular surfaces for the talar head appear continuous (this is only appreciated with the medial oblique view). Variations include a separate articular surface for the anterior subtalar joint and absence of an articulation completely (Figure 6-28).
The superior surface of the sustentaculum tali typically is flat in the lateral view; rarely, it appears curved. Also, the posterior aspect of the sustentaculum should not be continuous or articulate with the posteromedial talar process in the lateral view. Continuity is indicative of osseous coalition, articulation, or fibrocartilaginous union (see discussion of tarsal coalitions later in this chapter).
Distal Tibia and Fibula
Form variants of the distal tibia or fibula are infrequent. For example, the tibial and fibular malleoli are occasionally elongated (Figure 6-29A). An extended tibial malleolus anterior colliculus may be related to ossification of the deltoid ligament at its enthesis. Elongation of the fibular malleolus may be accompanied by a hooklike extension at its inferior tip. Another variant of form is the presence of an enlarged tubercle or process along the medial aspect of the tibial malleolus (Figure 6-29B) or the posterior aspect of either the tibial posterior malleolus or the fibular malleolus (Figure 6-29C,D).

FIGURE 6-24. Variation of calcaneal form/length. A: Elongated with normal contours. B: Short with enlarged posterior segment.

FIGURE 6-25. Flattened inferior calcaneal surface (arrowheads).

FIGURE 6-26. Variation of the anterior process: Enlarged and projecting superiorly (arrowheads), simulating an “anteater” calcaneus.
COALITION (SYNOSTOSIS/SYNCHONDROSIS/SYNDESMOSIS)
Union between two bones may be osseous, cartilaginous, or fibrous. Several terms have been used to describe these enigmas. The term synostosis, defined earlier, pertains to osseous union between two normally distinct bones. The term coalition is used more loosely and can pertain to osseous, cartilaginous (synchondrosis), or fibrous (syndesmosis) union; it is frequently applied to anomalous union of tarsal bones. The term ankylosis refers to consolidation of a joint because of disease, injury, or surgical procedure. (e.g., Fibrous or bony ankylosis may be seen as an end-stage presentation of inflammatory joint disease.) And fusion is defined as the operative formation of an ankylosis.1
Synostosis of a lesser toe distal interphalangeal joint is the most common synostosis seen in the foot and is almost always an incidental finding. Partial synostosis or bridging may be incidentally seen between metatarsal bones or at metatarsocuneiform joints. Tarsal coalitions, in contrast, are frequently associated with clinical symptomatology. This most likely is a result of faulty biomechanics and of limited range of motion between the affected bones.
Superimposition of two adjacent bones may mimic a synostosis. This can easily be distinguished by visually tracing the outer, articular margin of each bone. If their outlines can be identified, there is no synostosis. It is not recommended to use “continuity of the trabeculae across a joint” in determining whether or not a synostosis exists. This finding is often misleading when bones are superimposed on one another.
Interphalangeal Joint Synostosis
Proximal interphalangeal joint synostosis rarely occurs. However, synostosis of the lesser toe distal interphalangeal joint is frequently encountered in the foot (Figure 6-30). The fifth toe is most commonly affected. In decreasing order of frequency, distal interphalangeal joint synostoses of the fourth, third, and second digit occasionally are seen. Generally they are found bilaterally; and, fourth toe distal interphalangeal joint (DIPJ) synostosis will be accompanied with fifth toe DIPJ synostosis, third toe DIPJ synostosis will be accompanied with fourth and fifth toe DIPJ synostosis, and so on. A lesser digit that is clinically contracted (e.g., hammer toe or mallet toe) radiographically appears as if it lacks a joint space, and simulates a synostosis. However, if the articular margins of the distal phalanx base and middle phalanx head can be visually traced and identified, then there is no synostosis. They are superimposed on each other and will collectively have an increased density relative to the remainder of each bone. The radiodensity of a synostosis is homogeneous and similar to the middle and distal phalanges; no outline for the base or head can be visualized.
Intersesamoid Coalition
A rare instance of synostosis between the first metatarsophalangeal joint tibial and fibular sesamoids was reported by Saxby et al.24 in 1992.
Intermetatarsal Coalition
Partial coalition between two metatarsals (rare) may or may not be entirely osseous and is frequently associated with other anomalies.
Metatarsocuneiform Coalition
It is extremely rare to see synostosis between metatarsal and tarsal bones, especially the first cuneometatarsal joint.30 When present, they may be partial or complete (Figure 6-31). The incomplete can be fibrocartilaginous and, when so, will appear as osteoarthritis.
Tarsal Coalition
Synostosis may be seen between any two tarsal bones, but the most commonly encountered coalitions are calcaneonavicular and talocalcaneal.31 Talonavicular, calcaneocuboid, intercuneiform, cubonavicular, and cubocuneiform coalitions are rarely seen (Figure 6-32).
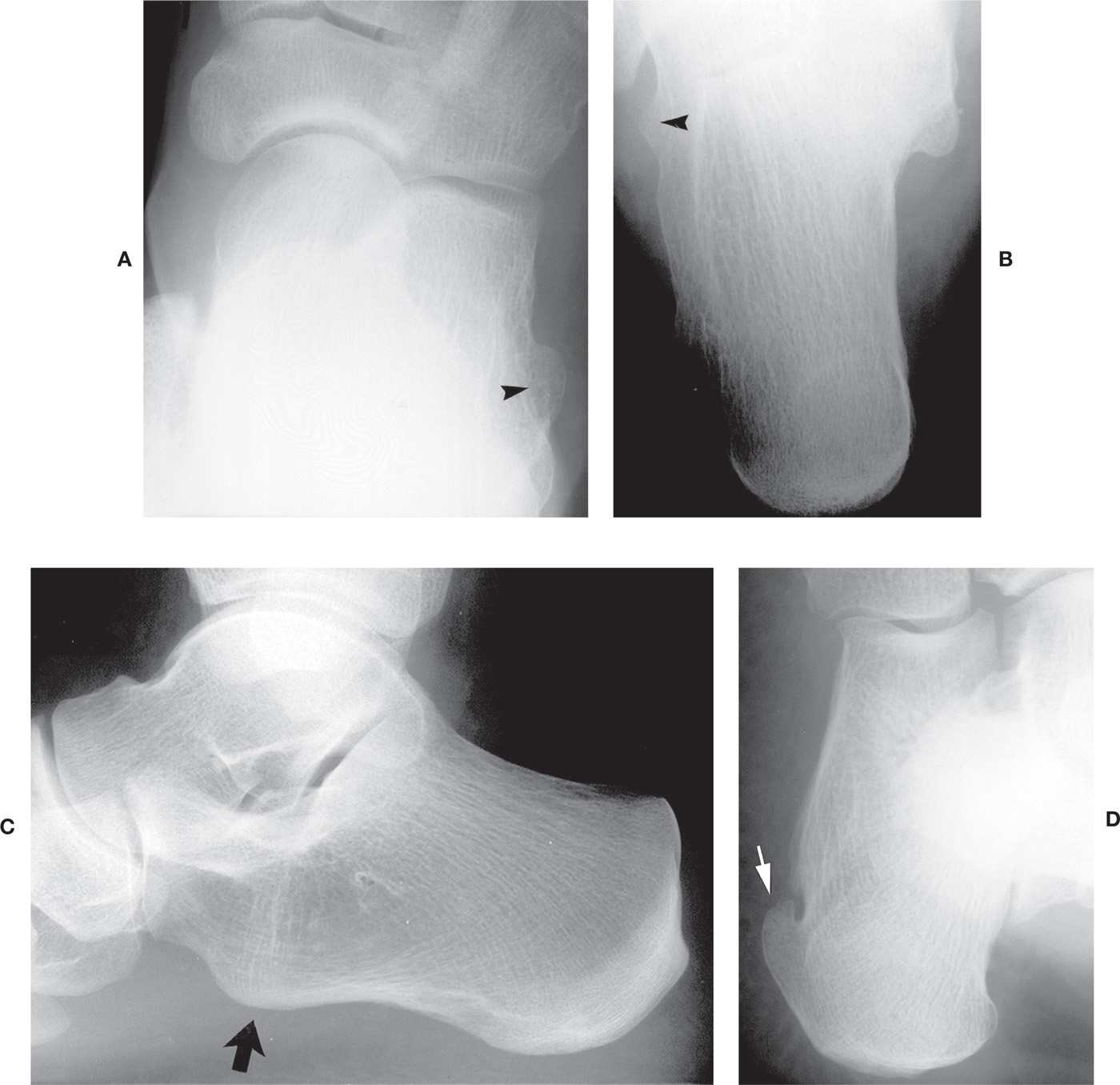
FIGURE 6-27. Variant calcaneal tubercles and tuberosities. A: Enlarged and prominent peroneal tubercle (arrowhead), dorsoplantar view. B: Large peroneal tubercle (arrowhead), axial view (different patient from A). C: Large anterior tuberosity (arrow) (lateral view). Also note the variant increased density that runs between the medial tubercle inferiorly and the Achilles tendon enthesis posteriorly. D: Incomplete hook-shaped lateral tuberosity (arrow) and resultant foramen.
In Asian countries, the isolated naviculocuneiform coalition is reported to be relatively common.32 The medial naviculocuneiform coalition, diagnosed by CT, was plantar (incomplete) and histologically comprised of fibrocartilaginous tissue in a large group of patients; the dorsal half of the joint was normal. Radiographically, the predominant finding is osteoarthritis, which is best seen in the dorsoplantar and lateral oblique views (Figure 6-33A,B). An incomplete synostosis may also be seen (Figure 6-33C,D).
The calcaneonavicular coalition (also known as calcaneonavicular bar) is clearly visible in the medial oblique view (Figure 6-34A,B) and the diagnosis is usually straightforward. The calcaneonavicular coalition can also be recognized in the lateral view, though superimposed, as an extension or elongation of the anterior calcaneal process superiorly (Figure 6-34C); this finding has been referred to as the “anteater nose sign.”33,34 In the literature, this has also been referred to as the “TLAP” or “too long anterior process” of the calcaneus.35 The appearance of the calcaneonavicular coalition in the medial oblique view varies, depending on the type of union. The superomedial aspect of the anterior calcaneal beak and inferolateral aspect of the navicular are continuous as one bony structure if there is osseous coalition or synostosis (Figure 6-34A). However, the fibrous or cartilaginous calcaneonavicular coalition is more frequently encountered. In this case, the two bones are in close apposition and appear to articulate with one another. The apposing margin of each bone may be quite irregular and sclerotic, resembling degenerative arthritis (Figure 6-34B). In contrast, the two bones are occasionally found in close anatomic relationship to one another, yet no obvious articulation or marginal sclerosis is identified. Although this latter presentation represents a variant form, it is questionable whether or not it may be a true calcaneonavicular coalition.

FIGURE 6-28. Subtalar joint variation. A: Absent anterior subtalar joint (arrowheads). B: Separate facet for anterior subtalar joint (arrowheads).
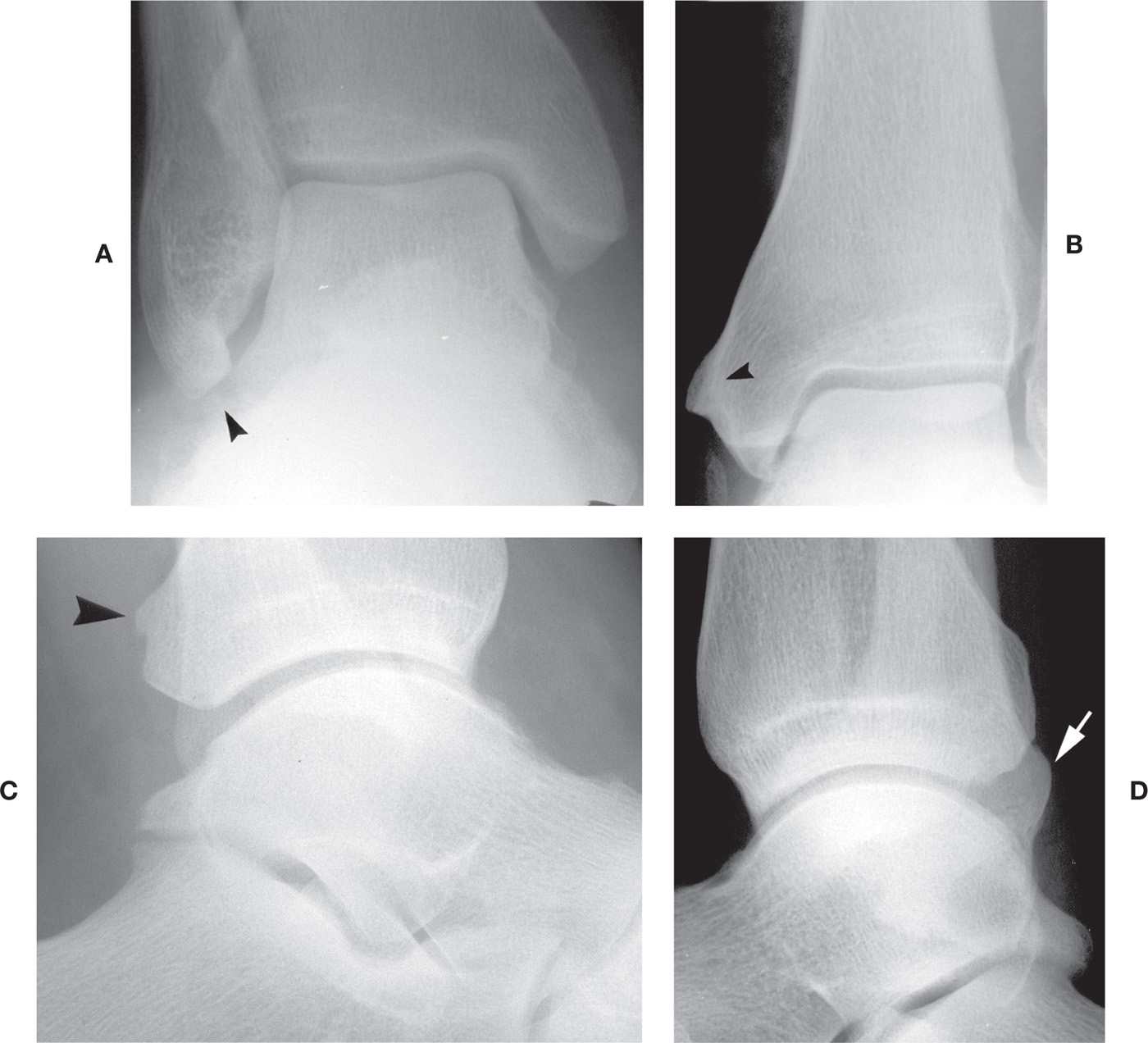
FIGURE 6-29. Distal tibial and fibular variants of form. A: Elongated fibular malleolus (arrowhead). B: Tubercle along medial aspect of tibial malleolus (arrowhead), a bilateral and symmetrical finding. C: Small tubercle along posterior surface of distal tibia (arrowhead), found bilaterally. D: Prominence of the posterior aspect of the distal fibula (arrow), a bilateral finding.

FIGURE 6-30. Interphalangeal joint synostosis: Third-, fourth-, and fifth toe DIPJs.

FIGURE 6-31. Intermediate cuneiform–metatarsal coalition. This finding was bilateral and symmetrical.

FIGURE 6-32. Rare intertarsal synostoses. Talonavicular coalition: A: Lateral view. B: Medial oblique view. Lateral cuneiform–cuboid coalition: C: Medial oblique view; there also is a fibrocartilaginous calcaneonavicular coalition.
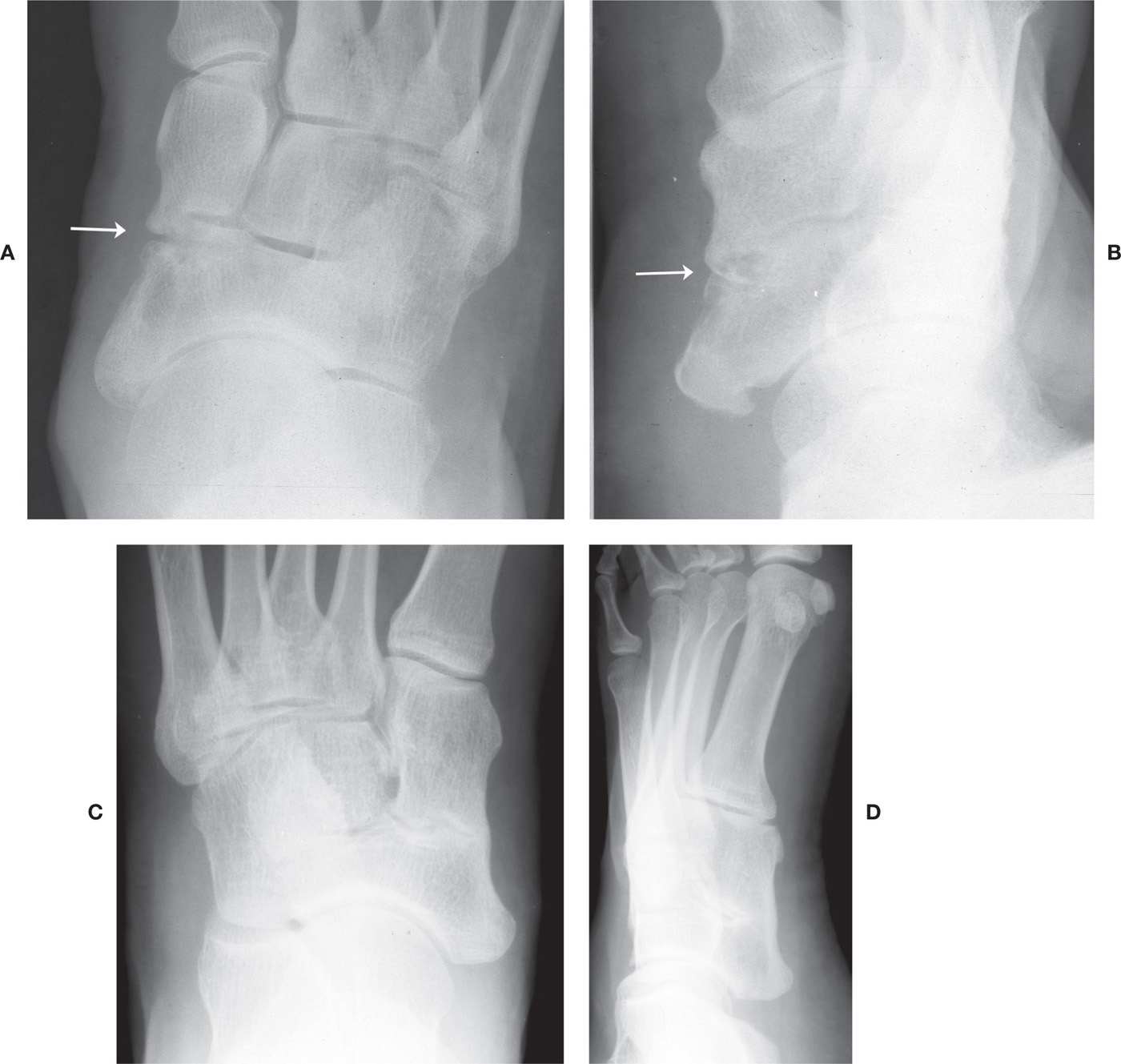
FIGURE 6-33. Incomplete medial cuneiform–navicular coalition. Fibrocartilaginous (arrow): A: DP view. B: Lateral oblique view. Synostosis (in a different patient): C: DP view. D: Lateral oblique view.
Lysack and Fenton36 have proposed four types of calcaneonavicular morphology that may be encountered in the medial oblique view: (1) the normal presentation where there is a wide gap between the two bones and no suggestion of articulation or union; (2) a short gap between the two bones, similar to an articulation, with widening and flattening of the calcaneus, and the adjacent margins are smooth and well defined (a synchondrosis); (3) a narrow articulation between the two bones that demonstrates irregular, rough, and poorly defined margins (syndesmosis); and (4) osseous union (synostosis) between the two bones. (See Figures 6-28A,B for examples of types 1 and 2; types 3 and 4 are demonstrated in Figures 6-34B,A, respectively.) It has also been suggested that the os calcaneus secundarius, found at the same site, is related to the formation of the calcaneonavicular coalition.37
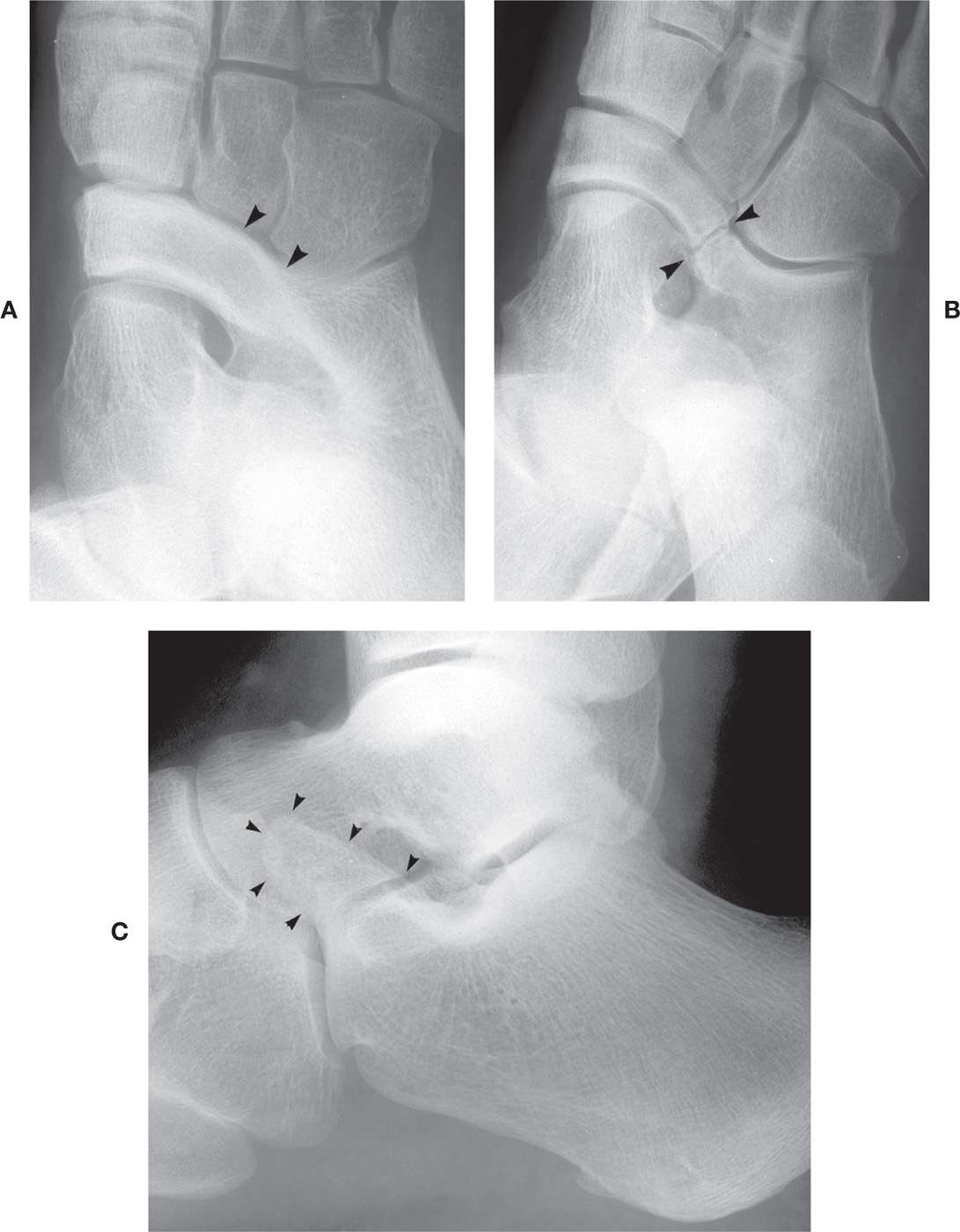
FIGURE 6-34. Calcaneonavicular coalition. A: Osseous (arrowheads) (medial oblique view). B: Fibrocartilaginous (arrowheads) (medial oblique view). C: “Anteater” calcaneus (arrowheads) (lateral view).
Based on three-dimensional anatomy using CT, Vidyadhar et al.38 classified calcaneonavicular coalition into four types (the cuboid form—its “medially extending prominence”—is described from a plantar perspective): Type I, the forme fruste, either the cortical tip of the calcaneus was irregular or an ossicle was present between the calcaneus and navicular, accompanied by slight blunting of the cuboid; Type II, the syndesmosis, narrowing of the nonossified gap between the calcaneus and navicular bones accompanied by further blunting of the cuboid extension; Type III, the synchondrosis, accompanied by distinct “squaring off” of the cuboid bone; and Type IV, the synostosis, accompanied by an absent (“no longer visible”) cuboid medial prominence. In their series of 37 patients demonstrating 69 coalitions (32 were bilateral), the distribution for Types I through IV was 28%, 23%, 45%, and 4%, respectively.
Identification of a calcaneonavicular coalition is best visualized if the foot is oblique 45° relative to the x-ray image receptor (the medial oblique view). If less than 45° is attained, there is superimposition of the anterior calcaneus and navicular, mimicking a calcaneonavicular coalition. Proper foot position can be determined by examining the relationship of the cuboid and lateral cuneiform in the radiograph. If the two bones are separate and distinct (such that the cuboid is wholly isolated), the oblique position was performed properly. If not, a distinct space is not seen between the two bones; this should not be misinterpreted as coalition.
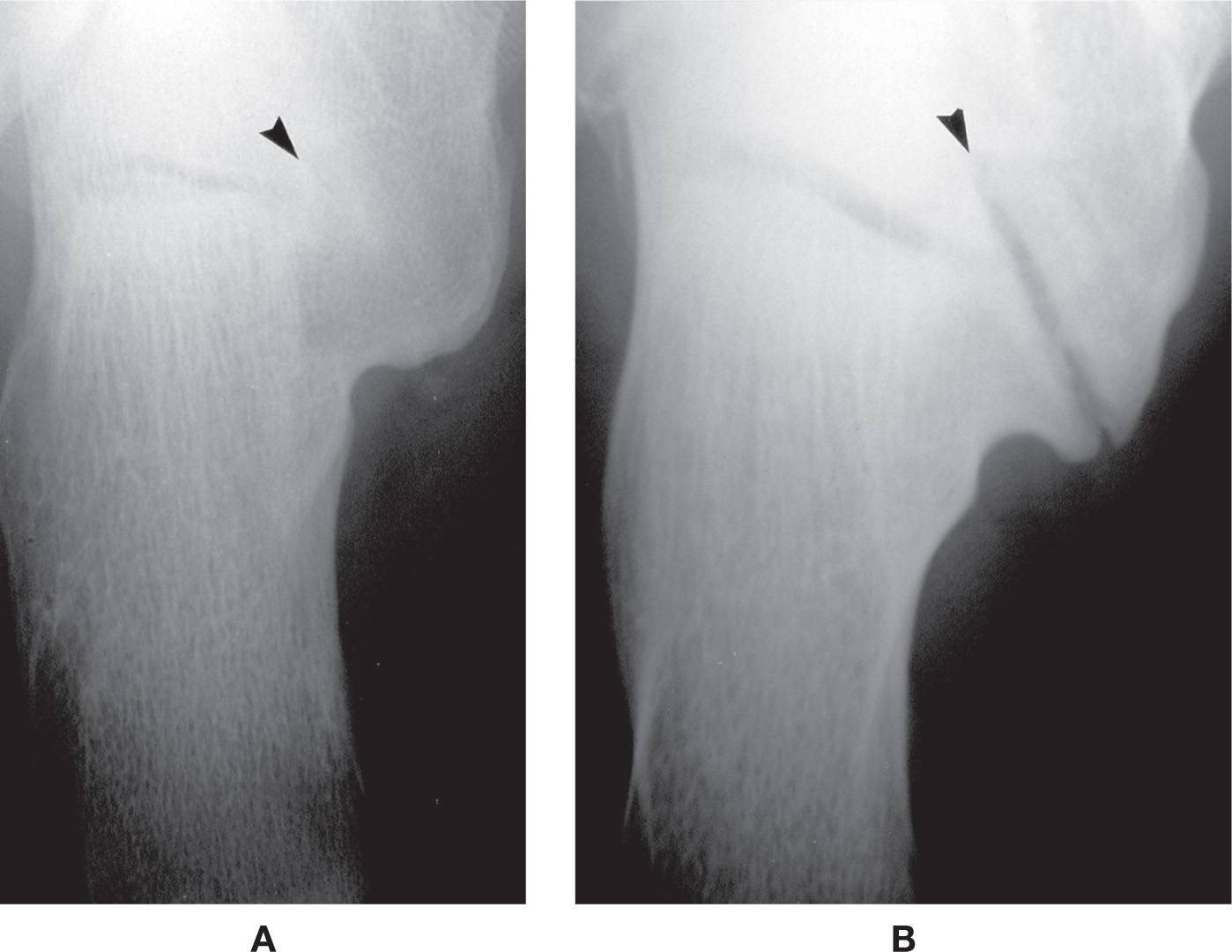
FIGURE 6-35. Middle talocalcaneal coalition (obliquely oriented) calcaneal axial view. A: Osseous (arrowhead). B: Fibrocartilaginous (arrowhead).
The talocalcaneal coalition receives the most attention in the literature of all the tarsal coalitions. Coalition of the middle talocalcaneal joint region is the most frequently encountered of the three possible talocalcaneal coalitions, anterior, middle, and posterior. Anatomically, the middle talocalcaneal coalition is either extra-articular (located between the posterior aspect of the sustentaculum tali and the talar body) and/or intra-articular.18 It may either be complete, nearly complete, incomplete, or rudimentary.39 Varying radiographic findings, therefore, can be attributed to variant presentations.40
Radiographically, the complete middle talocalcaneal coalition is best appreciated in the axial (Harris–Beath) view.41 The joint space is obliterated if osseous coalition is present (Figure 6-35A). If fibrocartilaginous, the middle talocalcaneal joint will be obliquely oriented (at approximately 45°), accompanied by gross joint space narrowing and subchondral sclerosis (Figure 6-35B). The os sustentaculi may rarely be identified in association with middle talocalcaneal coalition and, like the os calcaneus secundarius, has been suggested to contribute to the formation of coalition.42
Although it is not obvious in the lateral foot view, specific radiographic findings may be identified, leading to its diagnosis. Normally the shadows of the sustentaculum tali and the talar posteromedial process are separate and distinct. In contrast, if osseous middle talocalcaneal coalition is present, the inferior margins of these structures are continuous with one another (Figure 6-36). This finding has been coined the “C sign.”43 Absence of the C sign, however, does not negate diagnosis of coalition, especially in patients that have smaller lesions or are not yet skeletally mature.44 If fibrocartilaginous, one will see an articulation between these two anatomic landmarks that is irregular and sclerotic, mimicking a joint with osteoarthritis. In either case, associated findings include a rounded or flattened talar lateral process inferiorly (it normally is pointed). A spur or “beak” along the superior aspect of the talar neck (at the ridge) has also been associated with talocalcaneal coalition.27 But this latter finding is not a reliable indicator of coalition, because it can be seen when coalition is not present and vice versa. If necessary, CT and MRI can be used to further characterize the coalition’s location, character, and size, especially for preoperative assessment.31
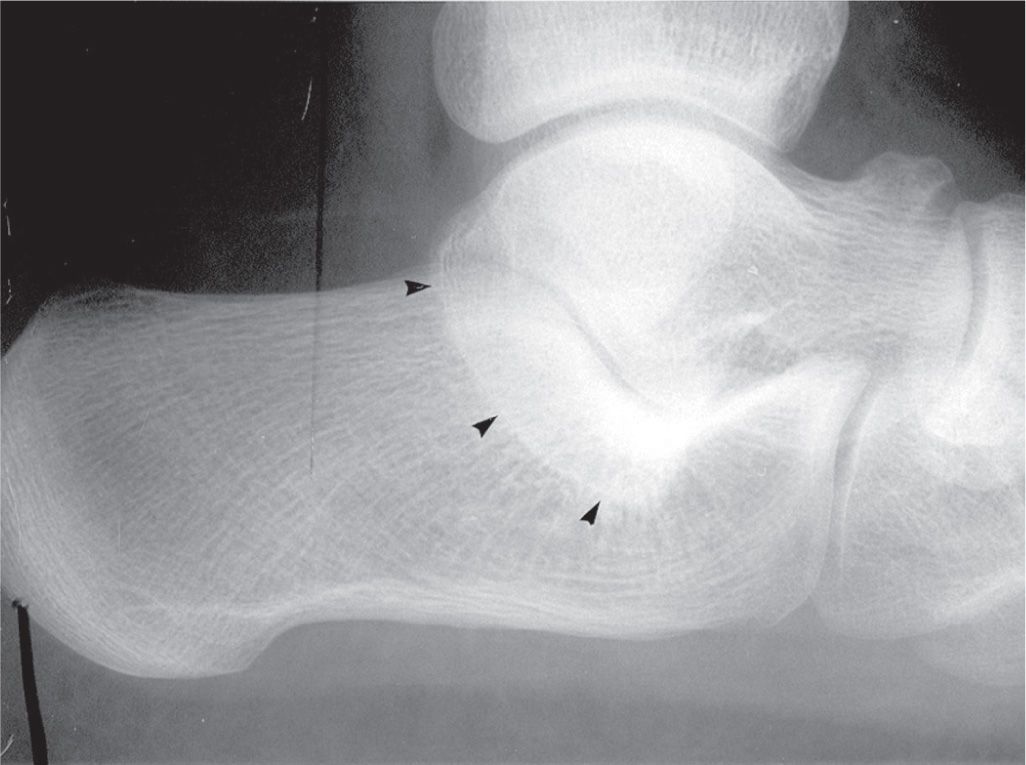
FIGURE 6-36. Middle talocalcaneal coalition: “C sign” (continuity between sustentaculum and talar posteromedial process, marked by arrowheads); associated findings are also seen (rounded lateral talar process and talar head beak).
Anterior and posterior talocalcaneal coalitions are rare. The anterior talocalcaneal coalition is identified in the medial oblique view. As already noted with the calcaneonavicular coalition, however, anterior talocalcaneal coalition is mimicked by superimposition of the two bones if the foot is not positioned properly. The posterior talocalcaneal coalition can be seen in the calcaneal axial view; however, CT may be necessary to make the diagnosis.
VARIANTS OF DENSITY
Radiolucencies
Varying degrees of radiolucency may be encountered at several anatomic locations. They are found in the absence of any clinical symptomatology, appear bilaterally in most instances, and are variations of normal radiographic anatomy. For example, a central radiolucency may be seen in the hallux proximal phalanx diaphysis that mimics a geographic, solitary lytic lesion (Figure 6-37A). Another example of a variant radiolucency is found in the medial aspect of the navicular in the dorsoplantar view, adjacent to the tuberosity (Figure 6-37B). It typically is bilateral and symmetric. A larger area of radiolucency is occasionally encountered in the body of the calcaneus in the lateral view (Figure 6-37C). The arrangement of trabeculae in this area is such that three patterns of stress trabeculae surround an oval or triangular central radiolucency, often referred to as the neutral triangle. Occasionally, the margins of this radiolucency are well defined, simulating a unicameral bone cyst.
Other sites where variant radiolucency is encountered include the metatarsal heads and the distal fibula. The medial aspect of the fifth metatarsal head is commonly radiolucent (Figure 6-37D). It simulates inflammatory joint disease, especially early rheumatoid arthritis. However, the subchondral bone plate is well defined and continuous when viewed with magnification. A similar radiolucency may be seen in the medial aspect of the remaining lesser metatarsal heads.

FIGURE 6-37. Variant decreased densities. A: Hallux proximal phalanx diaphysis. B: Medial aspect of navicular. C: Calcaneal neutral triangle. D: Fifth metatarsal head medially and the geographic decreased density in the second metatarsal head (a bilateral presentation).
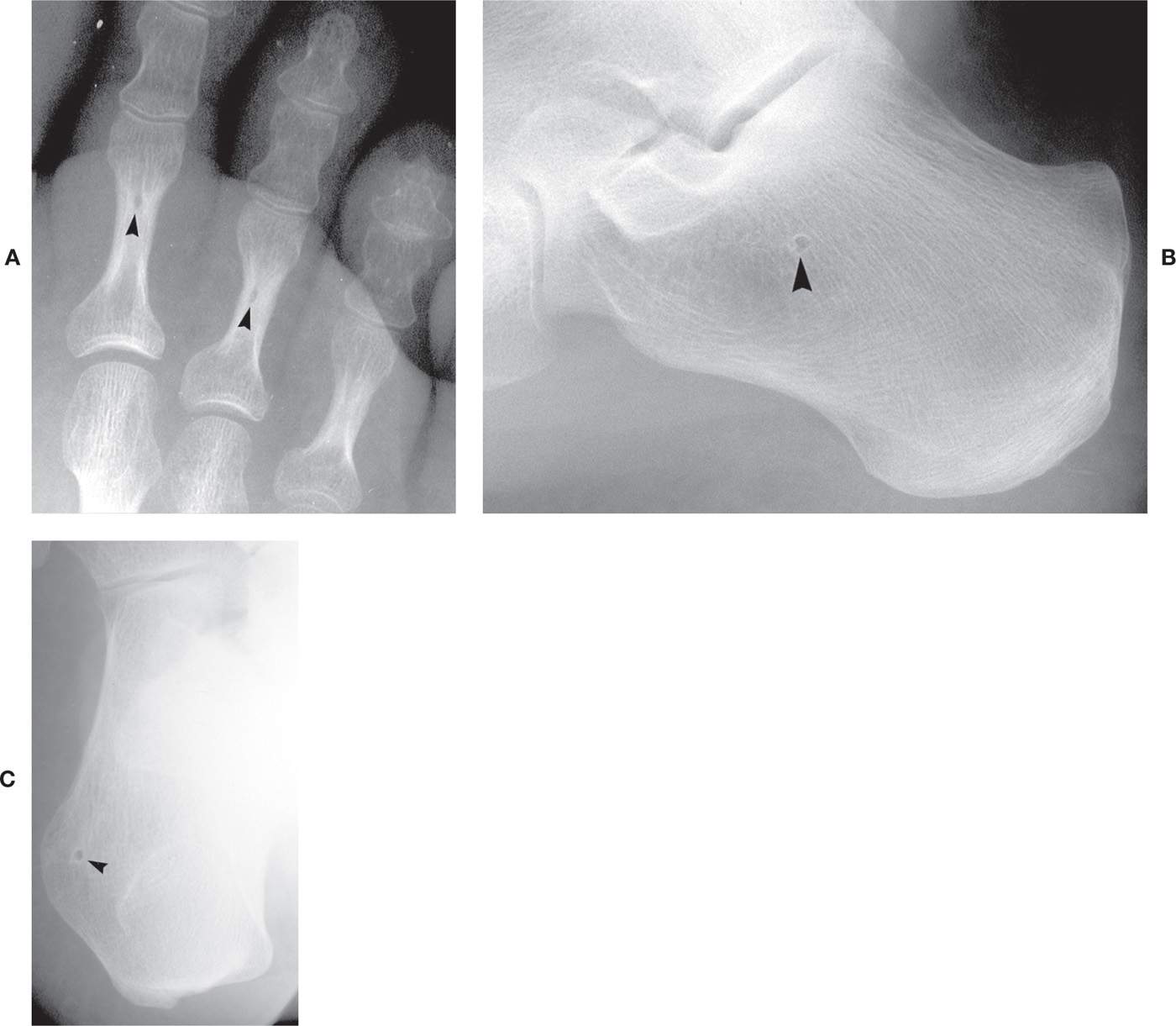
FIGURE 6-38. Variant “punched-out” radiolucent densities (arrowheads). A: Second and third toe proximal phalanx distal diametaphyses. B: Calcaneal body, central location. C: Calcaneal lateral tuberosity, small.
Small, well-defined, and round “punched-out” radiolucencies are occasionally seen. It is not uncommon to see a tiny, round lucency in the distal metaphysis of the lesser toe proximal phalanx that is central in location (Figure 6-38A). A similar finding may be encountered in the calcaneal body, in the “neutral triangle” (Figure 6-38B). Another round radiolucency is infrequently found adjacent to the calcaneal lateral tuberosity in the medial oblique view (Figure 6-38C); this has been referred to in the literature as a nutrient foramen,45 although it could also represent a developmental defect or incomplete ossification of the apophyseal growth center (compare to Figure 6-27D).
Increased Densities
A common variant of increased density appears as a solitary, geographic increased (cortical) density found in cancellous bone (Figure 6-39). This tumorlike lesion might be found in any foot bone and has been referred to as a bone island (also known as enostosis and endosteoma). Bone islands are incidental findings and are not associated with clinical symptomatology. A superimposed accessory sesamoid bone may simulate a bone island.
Some increased radiodensities correspond to osteologic landmarks. For example, a curvilinear sclerosis may be seen in the hallux distal phalanx base in the dorsoplantar view that corresponds to the anterior margin of the flexor tuberosity (see Figure 6-6). Another sclerotic density is commonly seen in the body of the calcaneus in the lateral view, superior to the medial tuberosity (Figure 6-39C). This curvilinear density corresponds to the inferior margin of the lateral tuberosity; its position and outline vary among patients.
Occasionally, the lower one-third of the posterior calcaneus is sclerotic relative to the body (Figures 6-27C and 6-39C). This sclerosis extends from the Achilles tendon enthesis to the medial and/or lateral tubercle inferiorly. It appears to represent accentuation of the stress trabeculae as well as superimposition of the margin of the convex posteroinferior calcaneus.
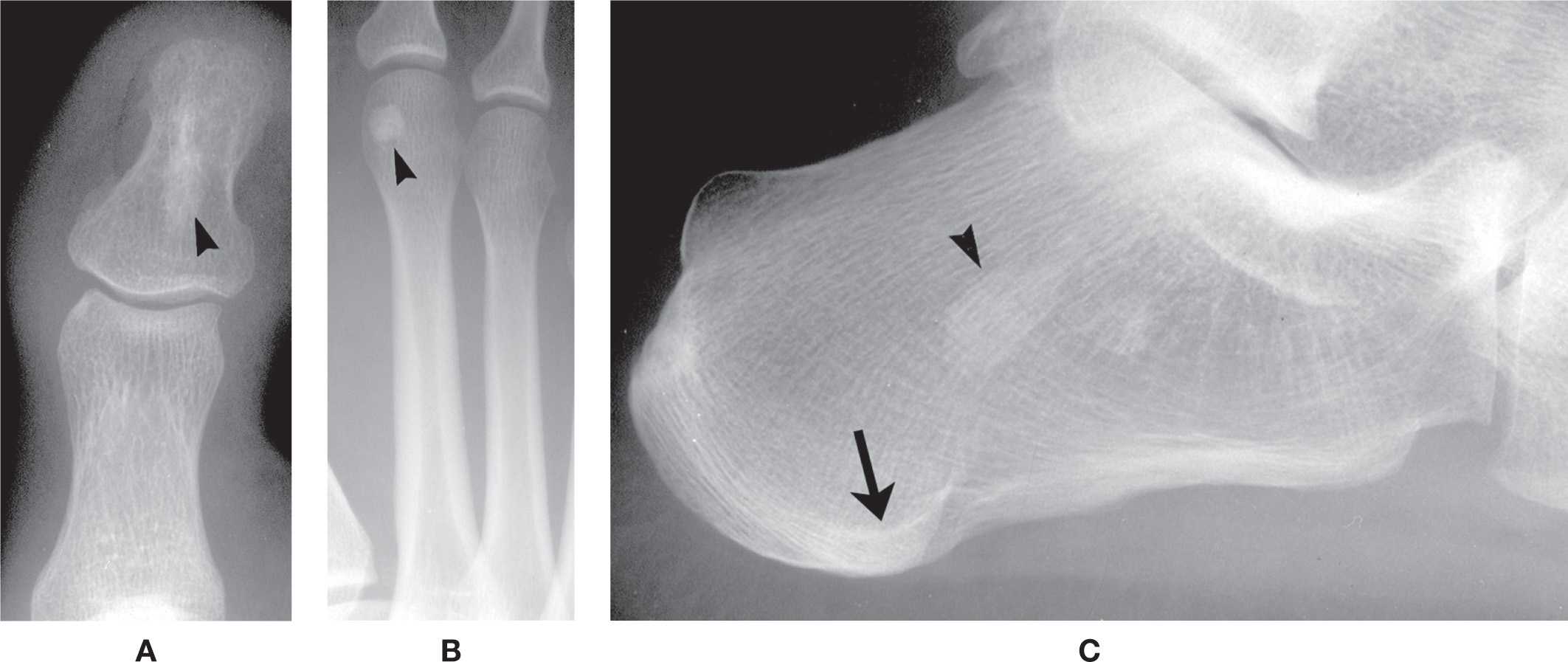
FIGURE 6-39. Variant increased densities in cancellous bone: Bone island. A: Hallux distal phalanx (arrowhead). B: Second metatarsal head (arrowhead). C: Central calcaneus (arrowhead). The semicircular increased density (arrow) in the medial tubercle is the superimposed lateral tubercle; it continues to the Achilles tendon enthesis posterosuperiorly as prominent trabeculations.

FIGURE 6-40. “Gun-barrel” presentation of distal phalanx due to positioning.
A severely contracted digit may be positioned such that its phalangeal shaft is parallel to the central x-ray beam in the dorsoplantar view. The resultant image may appear as an intense, radiodense circle, corresponding to the diaphyseal cortex. This has been coined the “gun barrel sign” because it mimics the appearance seen when looking down the barrel of a gun (Figure 6-40).
Superimposed soft tissue structures may present interesting findings. For example, an infrequent finding is the appearance of a well-defined increased density in the anteroposterior ankle view that runs vertically through the center of the ankle joint; its width spans at least half the width of the talar dome and widens superiorly. This shadow corresponds to the superimposed Achilles tendon (Figure 6-41).

FIGURE 6-41. Achilles tendon shadow (outlined by arrowheads) superimposed on distal tibia and talus in anteroposterior ankle view.
VARIANTS OF ARCHITECTURE
Cortical Bone
The cortex normally is radiopaque and homogeneous in density. Both the subperiosteal and endosteal surfaces should be smooth, continuous, and well defined. The combined thicknesses of the mid-diaphyseal cortices (medial and lateral) should equal 50% to 75% of the bone width. It is not uncommon, however, to see variations in the appearance of the cortex. Uniform increased thickness of the cortices may give the appearance of a “disappearing” medullary canal (Figure 6-42A). Also, the contour of a lesser metatarsal’s external margin may be irregular or wavy (but nonuniform) along its subperiosteal surface that can involve one or multiple bones (Figure 6-42B); this finding is predominantly located along the proximal one-half diaphysis and is an incidental finding. The differential diagnosis might include hypertrophic osteoarthropathy and melorheostosis.
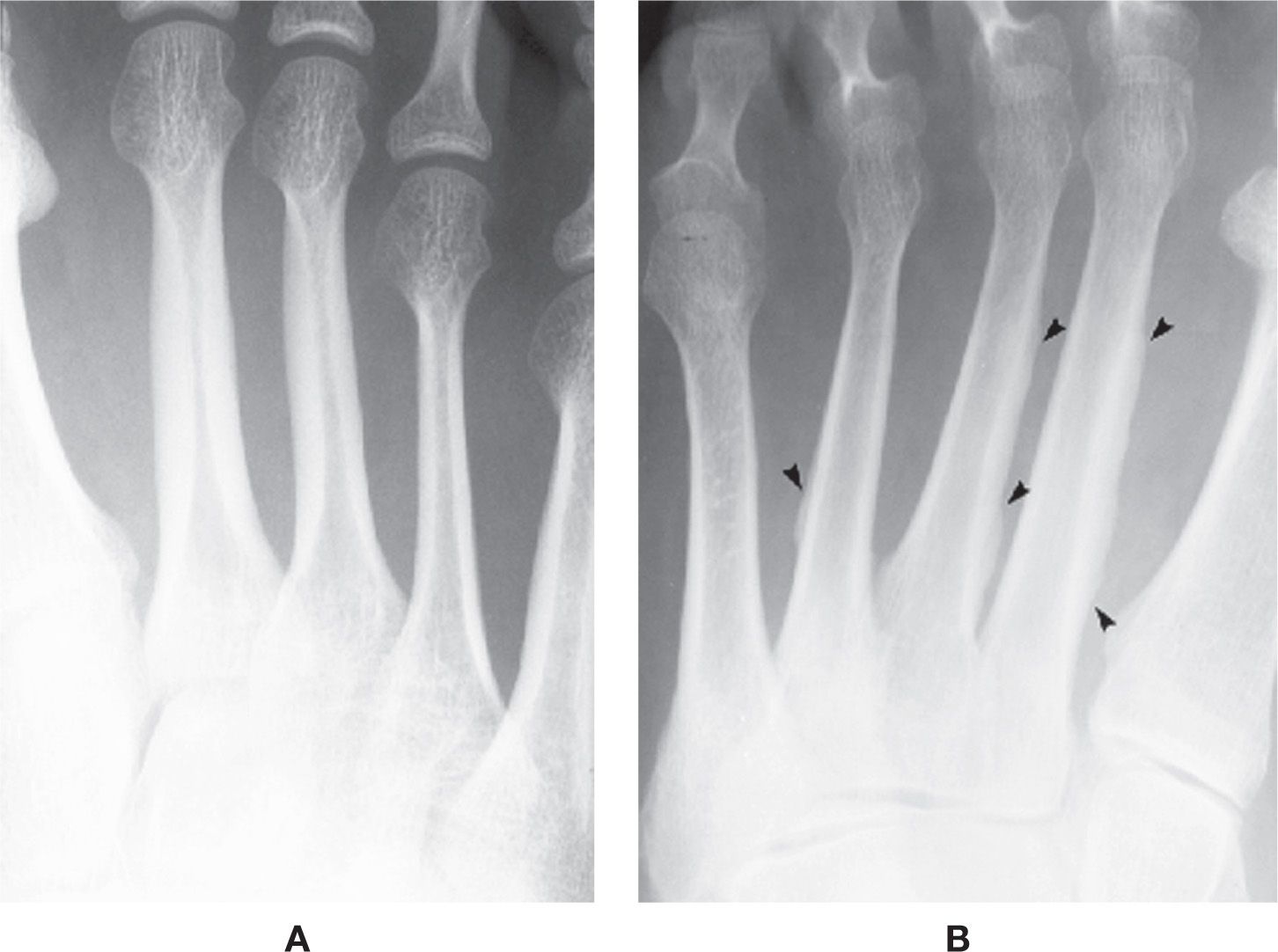
FIGURE 6-42. Variant architecture: Cortical bone. A: Symmetrical cortical thickening, periosteal and endosteal, second and third metatarsals. B: Asymmetrical and wavy periosteal, cortical thickening (arrowheads) of the second, third, and fourth metatarsals.
Cancellous Bone
The trabecular pattern in the distal metaphysis of the first metatarsal is commonly coarse in appearance (Figure 6-43A). These thickened trabeculae are normal and (if a solitary finding) do not represent osteopenia. The superimposition of these trabeculations on the sesamoids can simulate a fracture of the latter. A rare finding is a mosaiclike pattern of trabeculations, which is a generalized finding especially noticeable in the first metatarsal. A similar pattern may involve the phalanges (Figure 6-43B).
Transversely oriented trabeculae are occasionally encountered in the medullary portion of tubular bones (Figure 6-43C). These may be related to bone bars (reinforcement lines) in older patients but may present in younger adults.
ACCESSORY OSSICLES
Numerous accessory ossicles are present in the foot. Although their anatomic locations are fairly consistent, the morphology of these ossicles can be quite complex and diverse. It is not uncommon to find them unilaterally. When present bilaterally, their size, shape, or number is frequently asymmetric. These presentations certainly can confound interpretation of radiographs, especially when they are found in areas associated with clinical symptomatology. It is, therefore, important that the interpreter be able to recognize the typical and atypical presentations of these enigmas.
Os Interphalangeus
The os interphalangeus, also referred to as the interphalangeal “sesamoid,” is classically found along the inferior aspect of the hallux interphalangeal joint. It is rare to see this ossicle at the interphalangeal joints of the lesser toes. The position of the os interphalangeus is either central (more common, Figure 6-44A) or eccentric (Figure 6-44B); it may be round or oval in shape. Rarely, an ossicle may be encountered along the superior aspect of an interphalangeal joint (Figure 6-44C).
The centrally located os interphalangeus has long been considered a sesamoid bone because of its location in the plantar capsule that attached to the flexor tendon.16 (McCarthy et al.46 identified its location as in the joint capsule and the flexor hallucis capsularis interphalangeus; however, identification of this muscle has not been reproduced in the literature.47) Recent studies have reported that the ossicle is not a true sesamoid bone: it is intra-articular, positioned along the dorsal surface of the joint capsule that is separated from the tendon by a bursa; when the ossicle is absent, the bursa is not present and the flexor tendon is attached to the capsule.47,48 It also may appear as a pair (Figure 6-44D).
The eccentric os interphalangeus appears to have a different genesis from that of the centrally located ossicle. During development, the basal epiphysis of the distal phalanx occasionally has multiple ossification centers. A segment of this ossification center may remain separate into adulthood and persist as the eccentric os interphalangeus. A defect in the adjacent phalangeal base is frequently observed that corresponds to the size and shape of the unfused ossification center in this case. Rarely, the ossicle is adjacent to a defect along the proximal phalanx head. The eccentric os interphalangeus may also be the sequella of an old, unhealed fracture (i.e., nonunion). However, the majority of these patients do not recall any history of trauma, and many times the radiographic finding is bilateral in presentation.
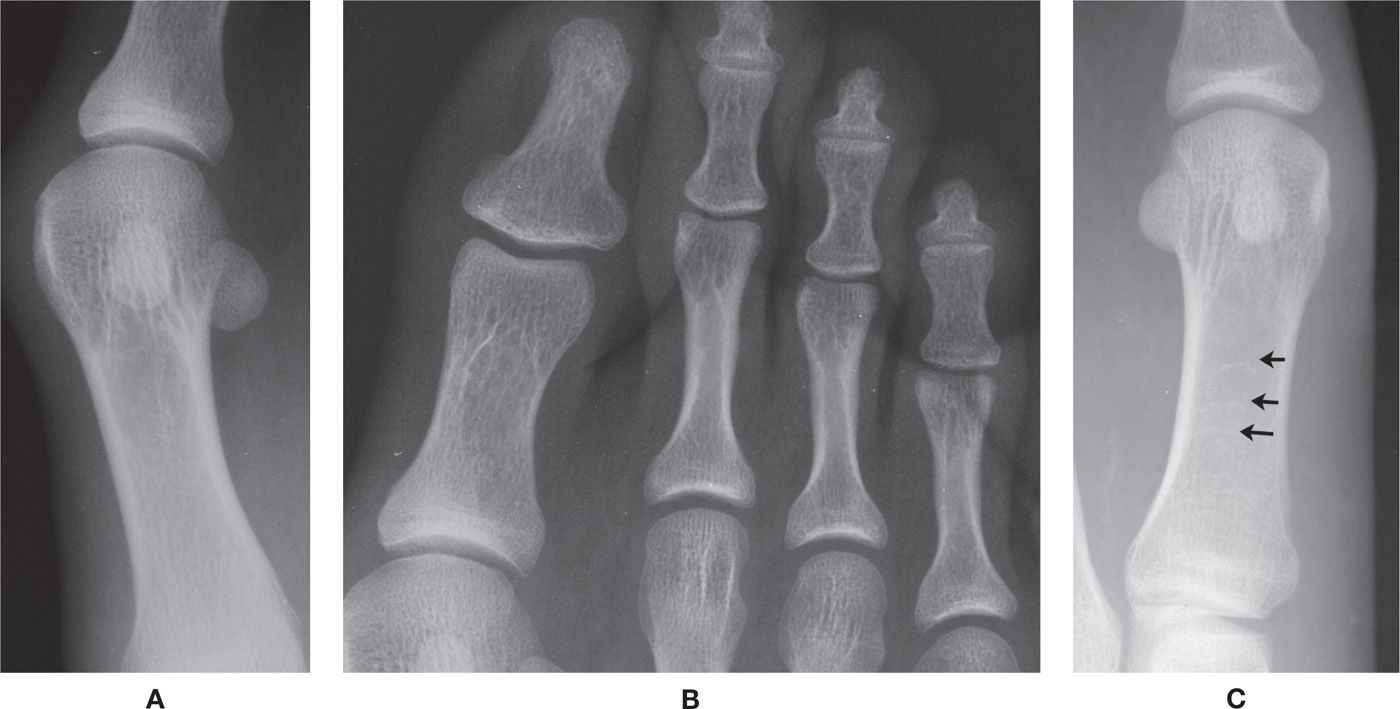
FIGURE 6-43. Variant architecture: Cancellous bone. A: First metatarsal distal metaphysis. B: Mosaiclike presentation in phalanges. C: Transverse trabeculations (arrows) in first metatarsal diaphysis.
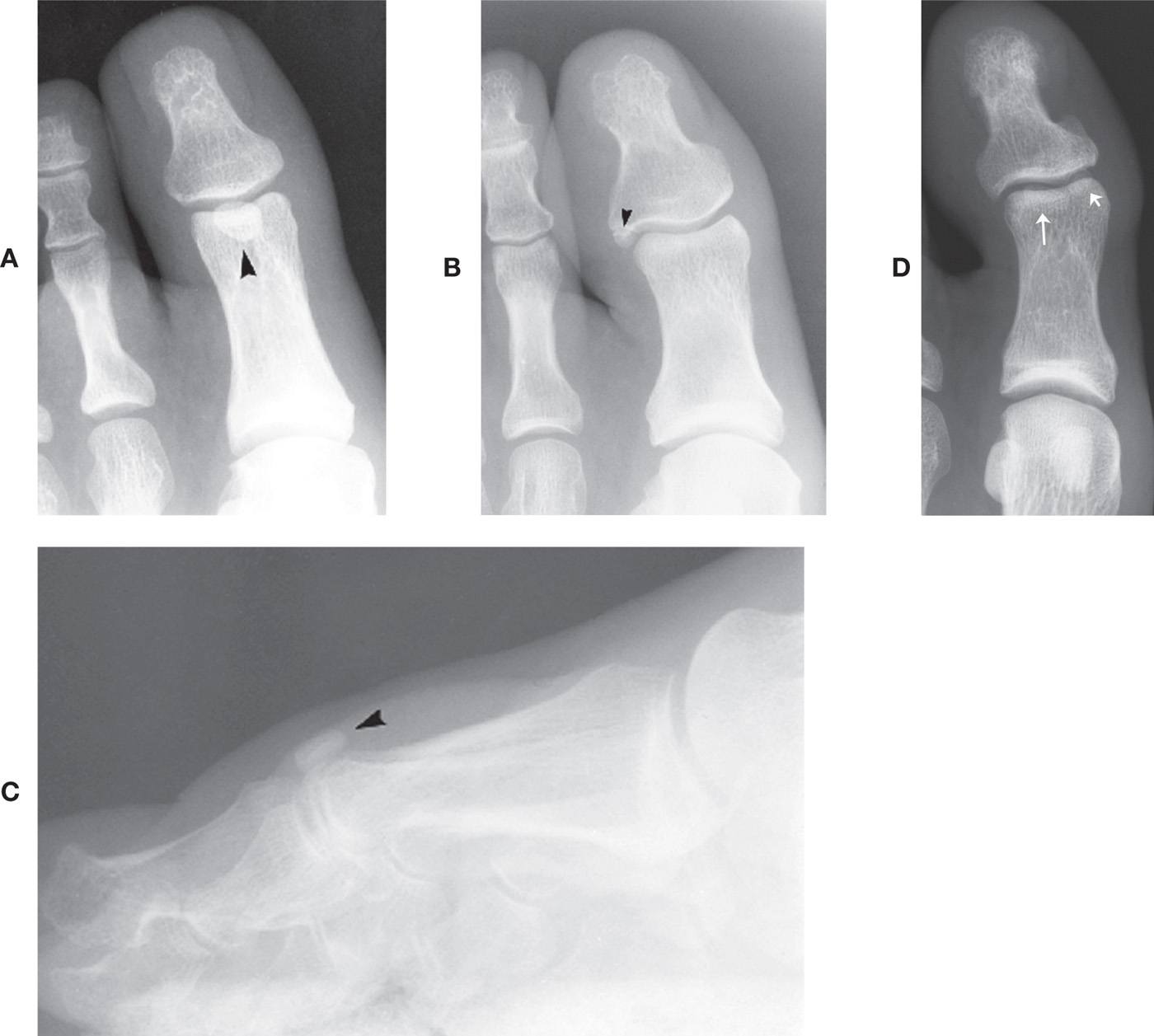
FIGURE 6-44. Os interphalangeus. A: Central location (arrowhead), large (DP view). B: Eccentric position (arrowhead), laterally. C: Rare superior position (arrowhead) isolated in lateral view. D: A pair (arrows).
The os interphalangeus can be identified in either the dorsoplantar or isolated lateral view of the hallux. Its transverse-plane position is best determined with the dorsoplantar view. It is superimposed on the proximal phalanx head and appears as a fairly well-defined oval of increased density. The os interphalangeus can be clearly identified with the lateral view if the hallux is isolated from the lesser digits. The lateral or medial eccentric os interphalangeus can be isolated with the medial oblique or lateral oblique view, respectively.
Accessory Sesamoids
A pair of sesamoid bones is consistently found at the first metatarsophalangeal joint. This occurs almost without exception. In addition, sesamoid bones may also be found along the inferior aspects of any lesser metatarsophalangeal joint, in varying combinations, and are known as accessory sesamoids (Figure 6-45A). For example, accessory sesamoids may appear at one, two, three, or all four lesser metatarsophalangeal joints as a single entity or in pairs. They appear circular or oval in shape and vary in size; rarely, they are bipartite. They frequently are bilateral, but may be asymmetrically distributed.
Accessory sesamoids are best isolated in the sesamoid axial view (Figure 6-45B). A solitary sesamoid is usually only medial, superimposed on the medial aspect of the metatarsal head in the dorsoplantar view, and seen along the inferomedial aspect of the metatarsophalangeal joint in the axial view.
Os Intermetatarseum (Os Intermetatarsale I)
The os intermetatarseum is situated superiorly between the first- and second metatarsal bases. Case et al.49 have described three types: freestanding, articulating, and fused. The freestanding os intermetatarseum does not articulate with the first or second metatarsal or the medial cuneiform (Figure 6-46A,B), as does the articulating type. The fused form is most rare and has been described united with either the first or second metatarsal or the medial cuneiform (Figure 6-46C).
The os intermetatarseum is best seen in the dorsoplantar view. It can occasionally be seen in the lateral view superiorly, although it typically is superimposed on the first metatarsal base. This ossicle may be round, oval, kidney-shaped, or linear, or may even resemble a rudimentary metatarsal. Its size also varies. Calcification of the perforating branch between the dorsal and plantar metatarsal arteries may simulate an os intermetatarseum. An os intermetatarseum is rarely encountered at the second lesser metatarsocuneiform joint (also known as the os cuneometatarsale II dorsale50) (Figure 6-46D). The os intermetatarseum is infrequently the cause of foot symptomatology.51–54
A sesamoid has been reported in the extensor hallucis brevis tendon at the level of the first metatarsocuneiform joint.55 The lateral radiograph of this lesion looks similar to that of the os intermetatarseum, although the location of the former is slightly more superior.
Os Cuneometatarsale I Tibiale
The os cuneometatarsale I tibiale is located adjacent to the first metatarsocuneiform joint medially (Figure 6-47).56
The os cuneometatarsale I tibiale plantare is a different ossicle that is located inferior to the joint.5 When present, it may be seen with the lateral view; however, due to its small size and superimposition by other structures, it might be difficult to visualize.
Tibialis Anterior Tendon Sesamoid
A sesamoid may infrequently be found in the tibialis anterior tendon near its insertion onto the first metatarsal base (Figure 6-48). It is located adjacent to either the first metatarsocuneiform joint or the medial cuneiform57 and is best seen in the dorsoplantar and, if located adjacent to the insertion site, lateral oblique views. More specifically, O’Rahilly56 describes this sesamoid as being adjacent to the facet along the cuneiform anteromedially for the tendon. This sesamoid may be either round, oval, or linear in shape. It may also be bipartite.

FIGURE 6-45. Accessory sesamoids. A: Dorsoplantar view (arrowheads identify multiple accessory sesamoids: one at the second, third, and fourth metatarsophalangeal joints; a pair is seen at the fifth metatarsophalangeal joint). B: Sesamoid axial view, different patient.
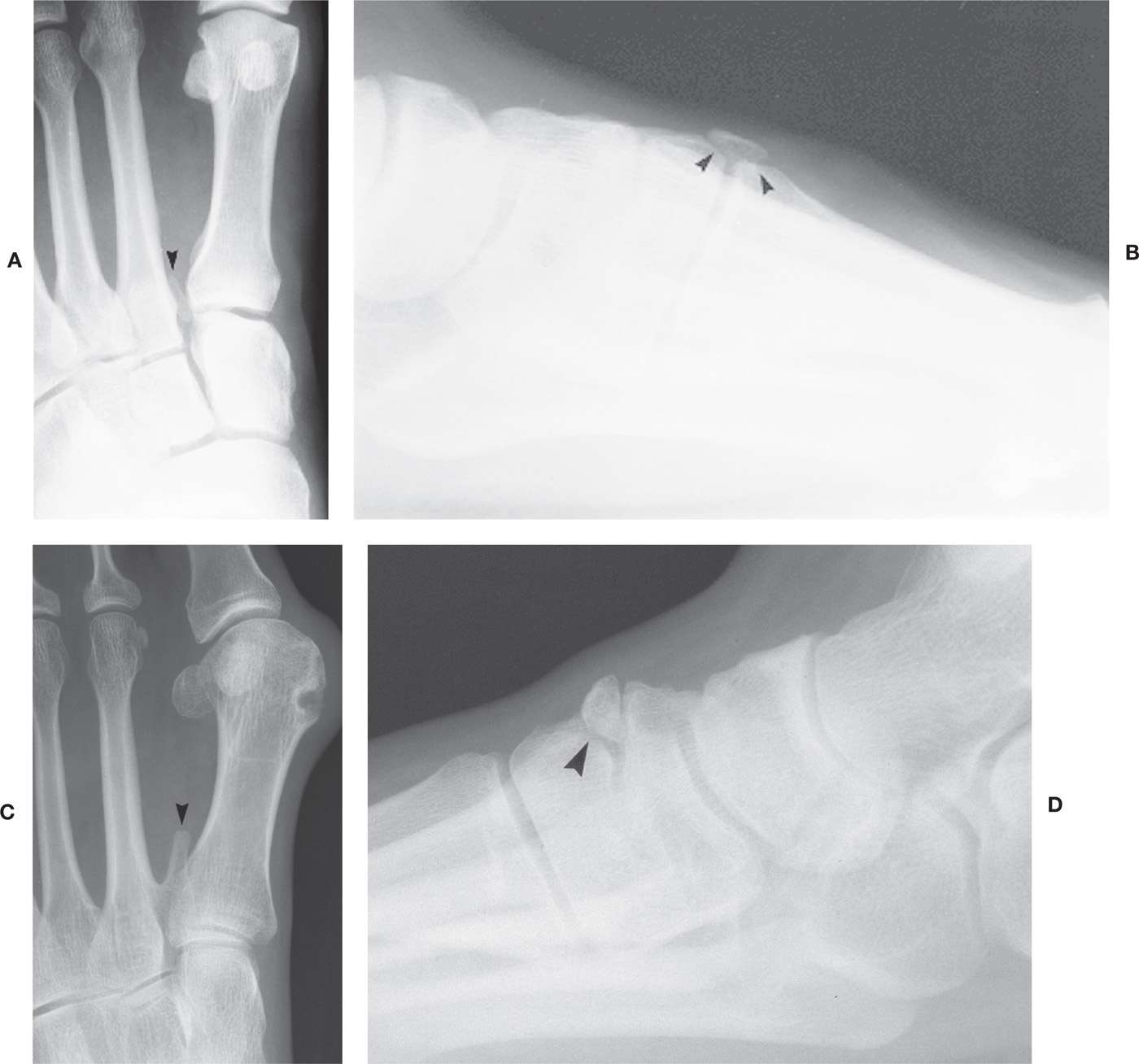
FIGURE 6-46. Os intermetatarseum (arrowheads). A: Long, linear. B: Large, triangular shape isolated in lateral view. C: Fused form. D: Rare position at second metatarsocuneiform joint.
Os Paracuneiforme (Os Cuneonaviculare Mediale)
This rare ossicle has been described or illustrated as being located either medial to the medial cuneiform or to the naviculocuneiform 1 joint (Figure 6-49).56,58
Os Intercuneiforme
This very rare ossicle has been reported along the posterosuperior aspect of the medial cuneiform.59 Dwight60 and Geist61 describe this ossicle as being small and wedge-shaped, located between the medial and intermediate cuneiforms (Figure 6-50).
Os Uncinatum (Os Unci)
The os uncinatum ossicle was identified inferior to the lateral cuneiform, adjacent to the third metatarsal.56 It may be free or appear as a hooklike prominence off the lateral cuneiform.
Os Cuboid
Zimmer observed an ossicle between the anterior aspects of the cuboid and lateral cuneiform, adjacent to the fourth metatarsal base (Figure 6-51).62 He questioningly names it “os cuboid?” in the figure caption, for lack of a better term. This rare entity appears to provide an articular surface for the fourth metatarsal base medially.

FIGURE 6-47. Os cuneometatarsale I tibiale (arrowhead).

FIGURE 6-48. Tibialis anterior tendon sesamoid (arrowhead): Adjacent to medial surface of medial cuneiform.
Os Cuboideum Secundarium
This extremely rare ossicle is found in the plantar aspect of the foot between the navicular and lateral cuneiform posteroinferiorly; proximally it articulates with the talus and calcaneus.63 It may also have contact with the navicular. Only three have been reported in recent literature.64–66 Even though the original description refers to its position between the navicular and cuboid inferiorly,63 the cases reported by Gaulke and Schmitz64 and Kaufman and Stacy65 show the ossicle directly beneath the cuboid and not near the navicular.

FIGURE 6-49. Os Paracuneiforme (arrow).

FIGURE 6-50. Os intercuneiforme (arrow) (bilateral and symmetrical).
Os Vesalianum
There has been debate in the literature as to whether or not the small ossicle (or “sesamoid”) located at the tip of the fifth metatarsal tuberosity briefly mentioned by Vesalius67 in his 1543 text was truly accessory or supernumerary and not the remnant of prior trauma or simply the normally occurring apophysis.56,68–70 In a paper by Burman and Lapidus,71 their “impression from the study of the literature is that there is no bone that can be called os vesalianum.” In 1928, Holland70 stated that the apophysis “is a good example of the bone which has so often been wrongly described as the Bone of Vesalius.” For example, Geist61 shows two cases of children with open physes, and he identifies the apophysis as the os Vesalii.

FIGURE 6-51. Os cuboid (arrowhead).
Holland70 describes three different ossicles that can occur at this site: the true epiphysis (or apophysis) seen only in childhood; a separate ossification that persists into adulthood and makes up nearly the entire tuberosity; and a small ossicle at the tip of the existing tuberosity. He proposes two options: either all three ossicles be referred to as the “Bone of Vesalius” or the term be restricted to a small ossicle at the tip of the tuberosity. The literature rarely ever refers to the true apophysis as an os vesalianum; therefore, the persistent apophysis should not be referred to as the os vesalianum either. Kohler and Zimmer state that the persistent apophysis of the fifth metatarsal tuberosity “does not represent a true os vesalianum,”62 an opinion also echoed by Birkner.50 Furthermore, Sarrafian states that the os vesalianum be differentiated from four entities: the ossifying apophysis, fracture, the ununited apophysis, and the sesamoid within the peroneus longus tendon (os peroneum).16 He further notes, “The os vesalianum is located just proximal to the tip of the well-developed tuberosity of the fifth metatarsal.”
Based on this survey of the literature, the ossicle located at the posterior tip of the fifth metatarsal tuberosity is known as the os vesalianum (Figure 6-52). The presence of this ossicle is quite rare, and it typically presents as a small, rounded calcific density. It is best seen in the medial oblique view. Ossification of the peroneus brevis tendon and old, unhealed (nonunion) avulsion fracture of the tuberosity tip may look similar to the os vesalianum.
Persistent Fifth Metatarsal Apophysis
The fifth metatarsal tuberosity apophyseal ossification center may remain separate into adulthood (Figure 6-53). This is known as a persistent apophysis and is occasionally misidentified as the os vesalianum.72 It is large in size and appears to articulate with the metatarsal base. It is clearly identified with the medial oblique view and is frequently bilateral and symmetrical.

FIGURE 6-52. Os vesalianum (arrowhead) (lateral view).

FIGURE 6-53. Persistent fifth metatarsal apophysis (arrowhead).
Os Peroneum
The os peroneum is a sesamoid bone found in the peroneus longus tendon. It varies not only in size, but also in number. It commonly is partite. The os peroneum is classically situated beside the cuboid bone just proximal to where the tendon runs along the peroneal sulcus, but its position varies considerably. It is best isolated in the medial oblique view (Figure 6-54). The os peroneum generally is superimposed on the cuboid in the lateral and dorsoplantar views. However, it may be identified in the lateral view if its position anatomically is more distal in the tendon; at this location, it articulates with the anterior aspect of the cuboid’s inferior tuberosity.
The os peroneum may infrequently be found at a more proximal location, adjacent to the calcaneocuboid joint or anterior calcaneus. This latter entity may easily be misinterpreted as an avulsion fracture. Location of the os peroneum adjacent to the calcaneus as opposed to the cuboid may be variation73 or may indicate a ruptured peroneal tendon with posterior sesamoid displacement.74 Recent literature has reported friction syndrome complicated by fatigue fracture,75 tendon rupture through a bipartition,76 and degenerative joint disease77 of the os peroneum.
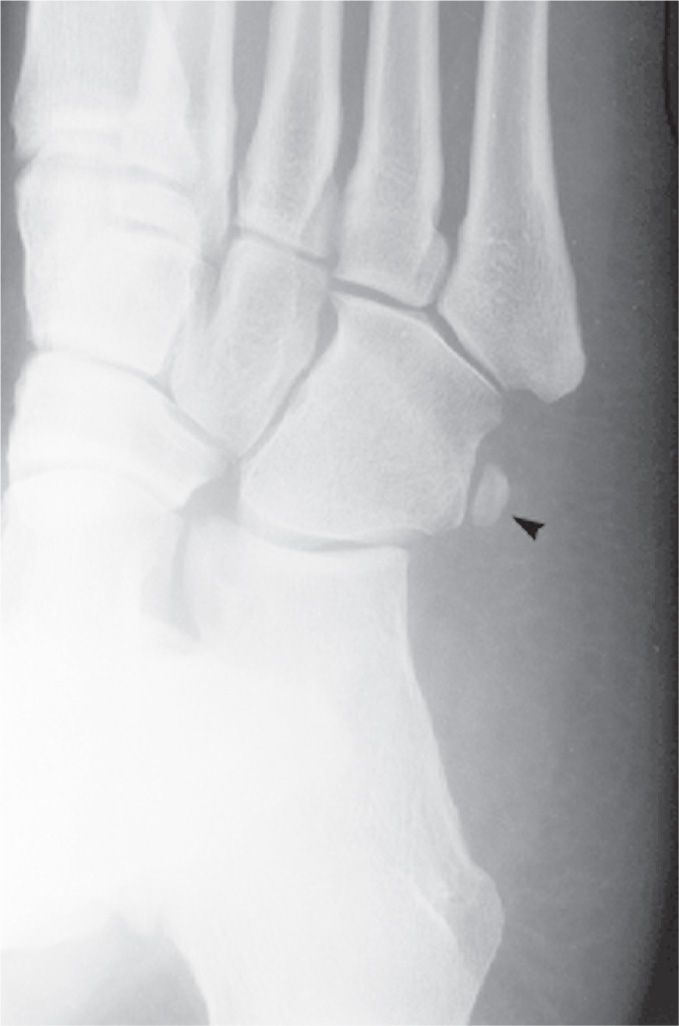
FIGURE 6-54. Os peroneum (arrowhead): Typical size and location adjacent to cuboid.
Os Infranaviculare
An ossicle uncommonly found along the superior aspect of the intermediate cuneiform–navicular joint is the os infranaviculare (Figure 6-55A).62 It has also been referred to as the os naviculocuneiforme I dorsale and os paracuneiforme I.78 It is best identified in the lateral view.
Another ossicle is seen infrequently along the superomedial aspect of the medial cuneiform–navicular joint in the medial oblique view (Figure 6-55B). This is near the location of the os intercuneiforme (see Figure 6-50).
Kim and Roh79 recently reported a large ossicle located superior to the medial cuneiform that articulates with the navicular, medial, and intermediate cuneiforms. Though its location was similar to that of the os intercuneiforme, they named it as os infranaviculare because of its direct attachment to the navicular.
Os Supranaviculare (Os Talonaviculare Dorsale)
The os supranaviculare is seen along the superior aspect of the talonavicular joint in the lateral view (Figure 6-56). This ossicle has a multitude of configurations. It may appear as an entirely separate ossicle, as a continuation of the articular subchondral bone, or even as an attachment to the navicular. As with many of the accessory ossicles, it may be impossible to differentiate the os supranaviculare from an old, nonunion fracture. An ossicle may infrequently be identified in the medial oblique view along the superomedial aspect of the talonavicular, possibly representing a variant position of the os supranaviculare.
Ingalls and Wissman80 have, by CT, demonstrated in two cases that the os supranaviculare sits in a small depression or “cortical notch.” They discuss the association of an incomplete fracture line (stress fracture) that originated from this notch and suggest further study.
Os Supratalare
The accessory ossicle located along the superior surface of the talar head is known as the os supratalare (Figure 6-57). It typically is located over the ridge along the talar head/neck but may be seen distally over the head. It easily can simulate an old, nonunion avulsion fracture and is only identified in the lateral view. Calcification of the talonavicular ligament may occasionally appear in the same location and mimic the appearance of an os supratalare.
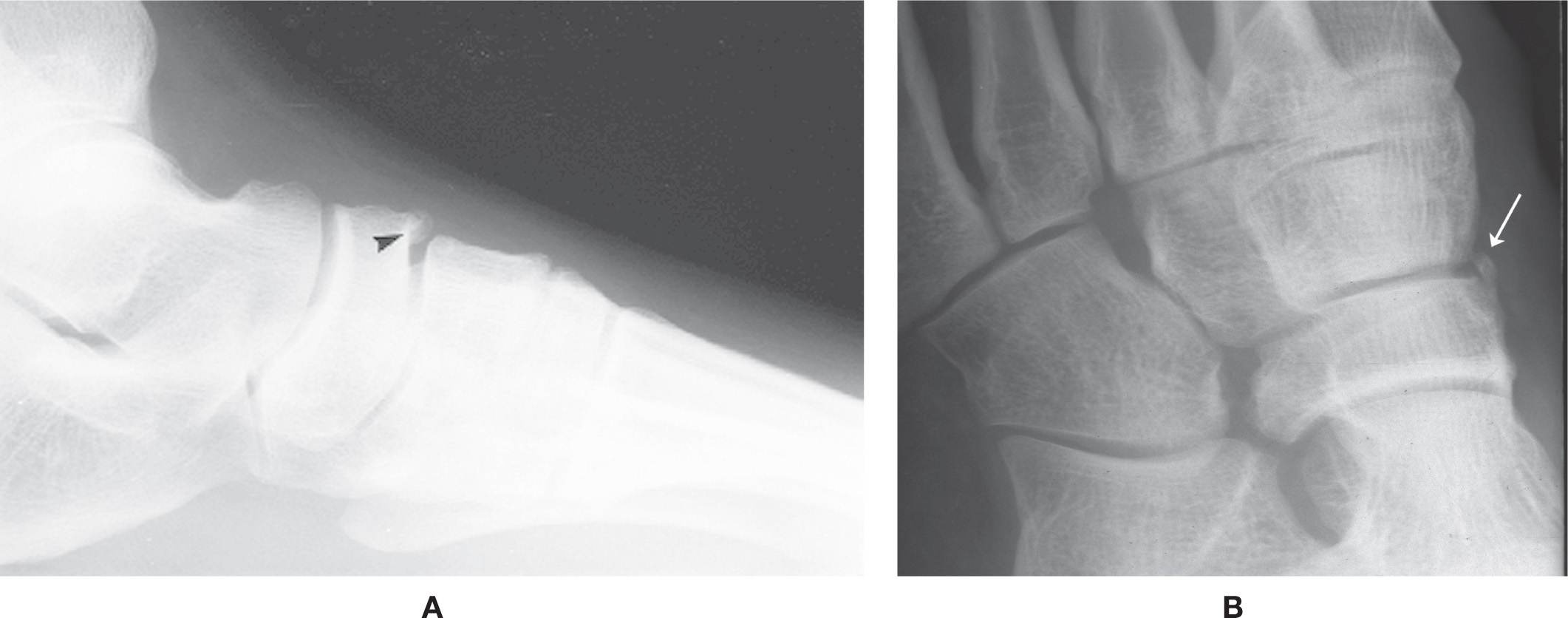
FIGURE 6-55. Os infranaviculare. A: DP view (arrowhead). B: Medial oblique view (arrow) (different patient).
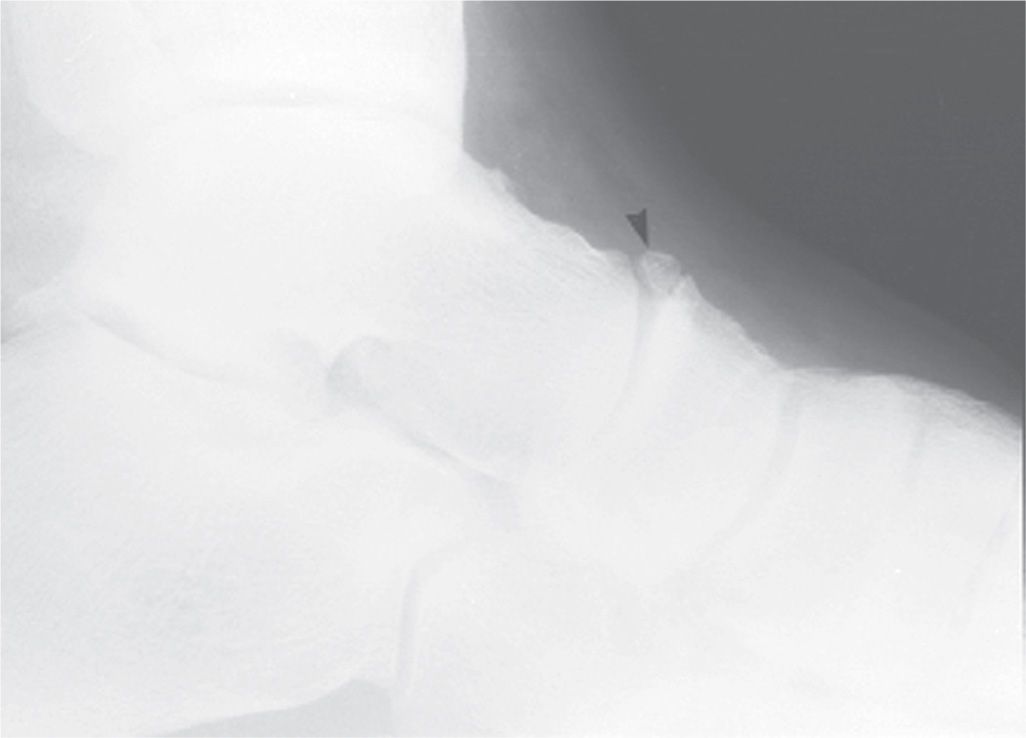
FIGURE 6-56. Os supranaviculare (arrowhead).
Accessory Navicular (Os Tibiale Externum, Os Naviculare)
An ossicle of varying size, shape, and position may be found adjacent to the navicular tuberosity. It is best identified in the lateral oblique view. Melamed81 recently suggested a modification of the Harris–Beath method to visualize the accessory navicular by rotating the toes inward.
The ossicle that is found adjacent to the navicular tuberosity may either represent a sesamoid in the posterior tibial tendon or an accessory ossification center for the navicular tuberosity. The sesamoid characteristically is round, small, and located at a distance at least 3 mm from the navicular tuberosity.82 This is the true os tibiale externum.83 The accessory ossification center, in contrast, is larger, characteristically triangular or heart-shaped, and in close apposition to the tuberosity. Cartilage or fibrocartilage may attach it to,84 or it may articulate with, the tuberosity, containing true synovial tissue.85 Occasionally, the accessory ossification center is fused to the tuberosity. This latter instance has been referred to as a “wraparound” navicular, cornuate or cornuted navicular, gorilloid navicular, and the Kidner foot type. With so many varied presentations, one can see why there has been discrepancy in the literature as to the definition and identification of this entity.

FIGURE 6-57. Os supratalare (arrowhead).
Based on these three distinct types of ossicles identified adjacent to the navicular tuberosity, Lawson84 has classified them as follows:
Accessory navicular type I: sesamoid in the tendon (Figure 6-58A)
Accessory navicular type II: articulating accessory ossification center (Figure 6-58B)
Accessory navicular type III: fused accessory ossification center (Figure 6-58C)

FIGURE 6-58. Accessory navicular. A: Type I: Bipartite sesamoid (arrowheads) in tendon. B: Type II (arrow). C: Type III (arrowhead).
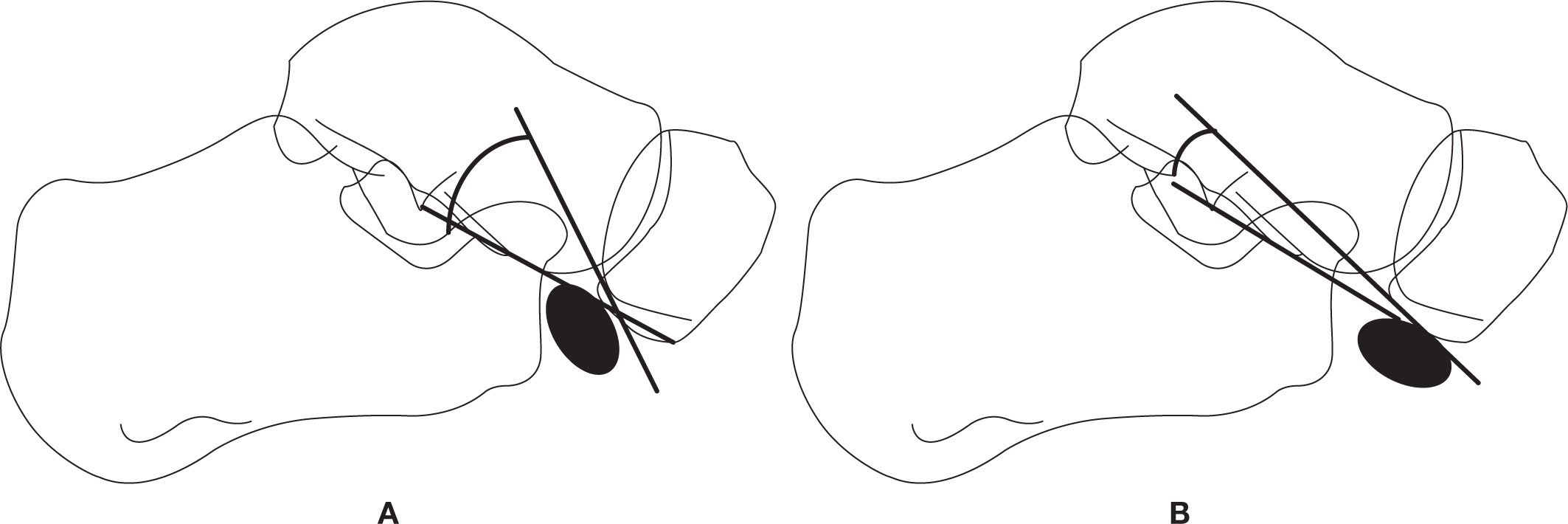
FIGURE 6-59. Type II accessory navicular subtypes. A: Type IIA. B: Type IIB.
This classification system best distinguishes between the varying forms of this enigma. It has also been correlated to their cross-sectional imaging appearances on CT and MRI.86 The term os tibiale externum should be used cautiously and applied only to the sesamoid entity (type I).87 The accessory navicular type I may be partite. The partition could be either transverse or longitudinal.
Sella and Lawson88 modified this classification by dividing the type II accessory navicular into two separate entities based on two criteria in the lateral view: (1) the accessory navicular position; and (2) the SOT (synchondrosis–ossicle–talar) angle. The two axes forming the SOT angle are (1) a line running through the synchondrosis and (2) a line that connects the inferior surface of the navicular to the inferior tip of the lateral talar process. In Type IIa, the TOC angle averages 56° (range 50°–70°) (Figure 6-59A). In Type IIb, the accessory navicular sits in a more inferior position and the SOT angle averages 21.5° (range 10°–35°) (Figure 6-59B). Huang et al.89 further subdivided each type into three subtypes; however, they only show noncropped images (making it difficult to see the accessory bone), and there are no accompanying descriptions.
The articulation between the accessory navicular type II and navicular may be quite irregular and sclerotic. These findings most likely represent degenerative joint disease and can simulate the appearance of a hypertrophic nonunion fracture. Of all types, the Type II accessory navicular has been most associated with the most symptomatology, 70% according to Chiu et al.90 Bone scintigraphy has been advocated for distinguishing between symptomatic and asymptomatic accessory navicular.91 MRI is also valuable for assessing the symptomatic type II.92,93
Os Calcaneus Secundarius
The os calcaneus secundarius is best seen in the medial oblique view, adjacent to and in close apposition to the calcaneal anterior process along its superomedial surface (Figure 6-60). Anatomically, the adjacent calcaneus has a crescent-shaped notch in the anterior calcaneal facet for the ossicle,94 which may or may not be appreciated radiographically. The ossicle is located centrally between the anterior calcaneus, talar head, cuboid, and navicular and appears to articulate with them, especially when larger in size. It is not clearly seen in the lateral view because it is superimposed on the calcaneus and talus. The os calcaneus secundarius can be mistaken for a fracture of the anterior calcaneal process.95 MRI may be valuable for differentiating fracture from the variant ossicle.96 In other cases, it may be that the ossicle itself is symptomatic; bone scintigraphy has also been used to support this.97

FIGURE 6-60. Os calcaneus secundarius (arrow).
Os Sustentaculi
This rare ossicle, also known as the os sustentaculum tali, has been identified anatomically along the posterior aspect of the sustentaculum tali (Figure 6-61). It is best visualized with the anteroposterior ankle and calcaneal axial (Harris–Beath) views.98 Another rare condition that simulates this ossicle is known as the “articulatio talocalcanea”99 or assimilated os sustentaculum tali,62 which represents an accessory joint between enlargements of the sustentaculum tali (posteriorly) and adjacent talus (medial tubercle).28 Talocalcaneal coalition has been attributed to fusion of the os sustentaculi with the talus and calcaneus.41,42 MRI has been used to evaluate the symptomatic os sustentaculi.100

FIGURE 6-61. Os sustentaculum tali (arrowhead).
Os Trochleare Calcanei
Rarely, an ossicle is found along the lateral aspect of the peroneal tubercle (or trochlea), adjacent to the peroneal tendons (Figure 6-62). It also has been referred to as the accessory calcaneus,101,102 os calcaneus accessorius, and os talocalaneare laterale.5,56,69 It may be seen in the dorsoplantar foot, anteroposterior ankle, or calcaneal axial views along the lateral surface of the anterior calcaneus, adjacent to the peroneal tubercle. Larger presentations also position the ossicle adjacent to the talocalcaneal joint. It may appear similar to a talus secundarius or an os subfibulare, which are located above the level of the talocalcaneal joint in the ankle AP view.102

FIGURE 6-62. Os trochleare calcanei (arrow).

FIGURE 6-63. Os subcalcis (arrow).
Os Talus Secundarius
Rarely reported in the literature, the os talus secundarius is found along the lateral surface of the talus in the anteroposterior ankle view.103,104 It may be attached to the talus by a synchondrosis or synostosis. If large enough, it may also articulate with the calcaneus and fibula.
Os Subcalcis
Another rare ossicle, the os subcalcis, may be seen along the inferior aspect of the calcaneal tuberosity. This probably represents an unfused ossification center for the calcaneal apophysis. When it is located beneath the medial tuberosity, it is seen in the lateral view. However, when closely associated with the lateral tuberosity, it is clearly identified with the medial oblique view (Figure 6-63).
Os Aponeurosis Plantaris
An ossicle or ossicles located in the plantar fascia have been referred to as the os aponeurosis plantaris (Figure 6-64).32 This entity may or may not be related to trauma (myositis ossificans).
Os Trigonum
An accessory ossification center can be found along the posterior aspect of the talar posterolateral process (Figure 6-65). When fused to the talus, the elongated posterior process is known as the trigonal (Stieda’s) process. If it remains unfused and separate, it is known as the os trigonum. In either case, its inferior surface typically articulates with the calcaneus105 or the posterior subtalar joint.106 The os trigonum may have a fibrous, fibrocartilaginous, or cartilaginous attachment to the talus.16,107 An articulation may be identified between it and the posterior talus. Occasionally, it may exhibit findings suggesting osteoarthritis. The size of this ossicle ranges from small to large. It is best seen in the lateral view but is infrequently viewed in the medial oblique view (the leg must be perpendicular to the foot to prevent superimposition by the fibula). Paulos et al.108 recommend a subtalar oblique technique performed at 30° to help differentiate between os trigonum and acute fracture.

FIGURE 6-64. Os aponeurosis plantaris (arrowheads).

FIGURE 6-65. Os trigonum (arrowhead).
Bone scintigraphy may be a valuable diagnostic study for differentiation between symptomatic and asymptomatic os trigonum.84,109 Focal intense uptake suggests degenerative disease and/or unhealed fracture. CT110 and MRI,111 the technique of choice, have been used to assess the symptomatic os trigonum or to differentiate the trigonal process from fracture. Dynamic fluoroscopy and ultrasound have also been used.106
Talus Partitus (Bipartite Talus)
Schreiber et al.112 report a case that divides the talar body into anterior and posterior segments; they believe that it may be a secondary ossification center for the talus.112 It resembles a large os trigonum and talar body fracture.5 It has been reported with talar fracture.113 Differential diagnosis for the os trigonum includes the talus partitus.114

FIGURE 6-66. Os accessorium supracalcaneum (arrow) posterior to an os trigonum.
Os Accessorium Supracalcaneum
The os accessorium supracalcaneum is an extremely rare ossicle. It is found along the superior surface of the posterior calcaneus. It can be mistaken for the os trigonum; however, the os supracalcaneum is not in direct apposition to the posterior talar process. The os supracalcaneum, when present, may be large and easily recognized in the lateral view. It has been reported to be attached to the Achilles tendon and have a bony bridge with the calcaneus.115 Occasionally, it is also found with an os trigonum just anterior to it (Figure 6-66).
Os Talotibiale
An accessory ossicle infrequently seen along the anterior aspect of the ankle joint116,117 in the lateral view (Figure 6-67) is the os talotibiale. It is found in close apposition to the most anteroinferior aspect of the tibia. It can easily be mistaken as a loose osseous body. However, the latter entity is usually associated with other degenerative joint findings. Rarely, an ossicle may present along the posterior aspect of the ankle joint. This unnamed ossicle, like the os talotibiale, is closely apposed to the tibia.
Os Subtibiale
The os subtibiale is an ossicle found just inferior to the tibial malleolus (Figure 6-68). It varies considerably in size and shape. Coral118 states that the true os subtibiale is distinct and separate from the anterior and posterior colliculi of the medial malleolus, and can be mistaken for the following conditions: unfused malleolar accessory ossification center, loose osseous body, acute or nonunion avulsion fracture, and deltoid ligament ossification. Reports of the os subtibiale misinterpreted as fracture has been reported,119,120 and it also has been related to posterior tibial tendon dysfunction.121 The cases reported by Coral118,120 are directly apposed to the posterior colliculus of the tibial malleolus. In contrast, malleolar avulsion fractures involve the anterior colliculus. This relationship is best appreciated in the lateral view. The os subtibiale and avulsion fracture may be impossible to differentiate in the AP and mortise ankle views alone.

FIGURE 6-67. Os talotibiale (arrowhead).

FIGURE 6-68. Os subtibiale (arrow); probably an unfused malleolar accessory ossification center.
Bellapianta et al.122 recently reported large, bilateral os subtibiale associated with middle talocalcaneal coalition. However, since both ossicles appear to encompass both colliculi and are more anteriorly positioned, these are more than likely examples of the unfused malleolar accessory ossification center. Coral118 believes that small ossicles inferior to the tip of the anterior colliculus are also unfused secondary ossification centers, if not related to prior injury.
Os Subfibulare
Several ossicles may be found adjacent and inferior to the fibular malleolus; they are sometimes all generically referred to as the os subfibulare. However, Coughlin5 states that the true os subfibulare is positioned posterior to the fibular malleolus and should be differentiated as such from the unfused apophyseal ossification center that is located anteriorly, and the unfused avulsion fracture123 versus unfused accessory ossification124 that may be seen inferiorly (Figure 6-69). Champagne et al.125 found the posteriorly positioned os subfibulare encased within both peroneal tendons; they agree with Coughlin that the term os subfibulare be reserved for the posteriorly positioned ossicle, but also that it be considered a sesamoid.
The os subfibulare is seen in both the AP and mortise ankle views. It is not readily visible in the lateral view but can appear as a fairly well-defined increased density superimposed on the talus. One can determine the anterior versus posterior position with the lateral view, and may see the smaller ossicle inferior to the tip in some instances.
A large accessory ossification center for the fibular malleolus may be encountered in the same location as the os subfibulare. It is directly related to ankle joint instability because of insertion of the calcaneofibular and/or anterior talocalcaneal ligaments and abnormal movement between the accessory ossification center and distal fibula.126
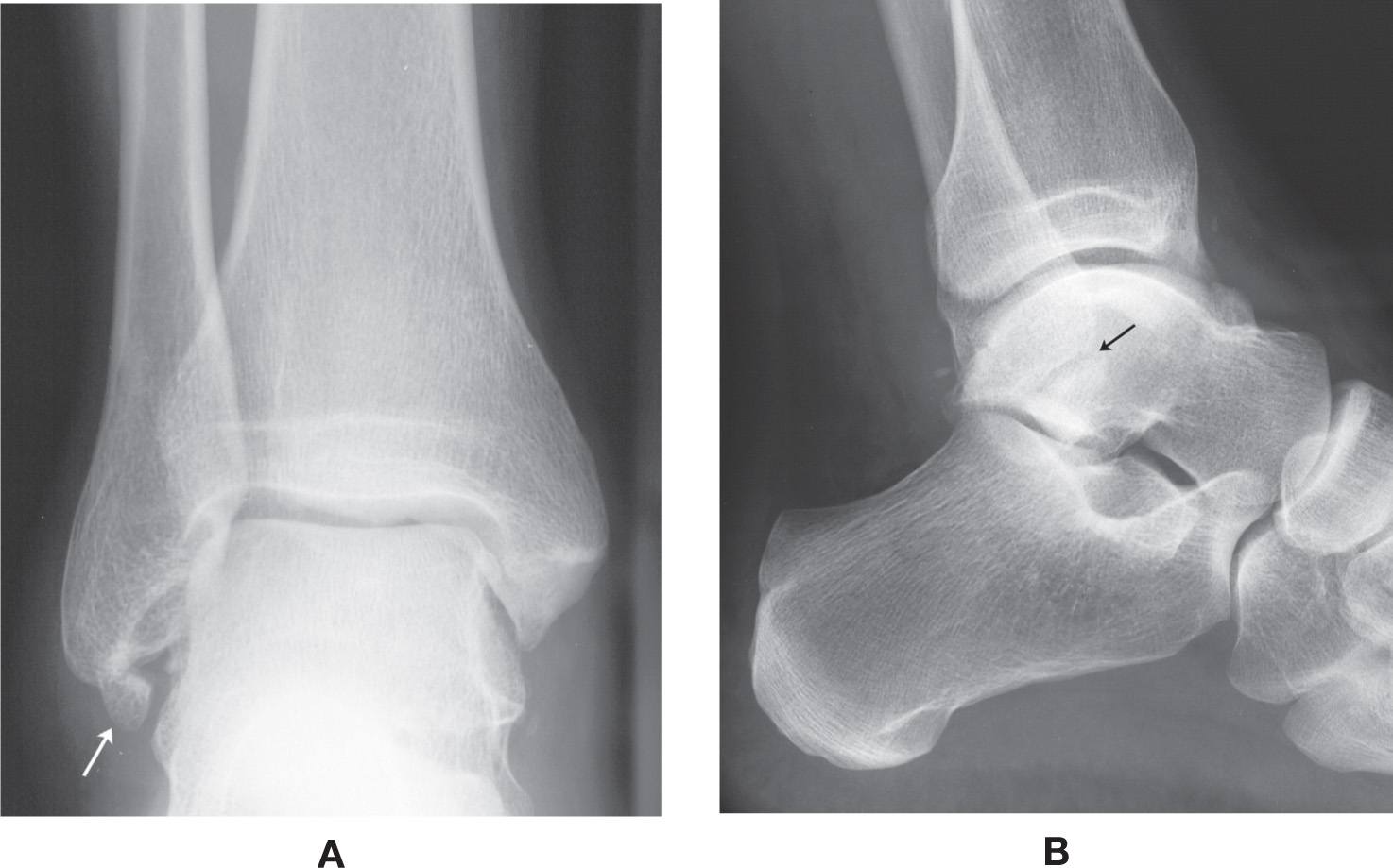
FIGURE 6-69. Os subfibulare (arrow); probably an unfused apophyseal ossification center. A: Anteroposterior view. B: Lateral view, identified along the anteroinferior margin of the fibular malleolus.

FIGURE 6-70. Os retinacula (arrow).
Os Retinaculi
An ossicle may be seen along the lateral aspect of the fibular malleolus near the peroneal retinaculum (Figure 6-70); this ossicle is known as the os retinacula.127
Accessory Talus (Talus Accessorium)
Feeney et al.128 reported a large ossicle along the dorsomedial aspect of the talus in a 7-year-old female who also had an accessory toe removed from the first metatarsal base. The extra tarsal ossicle was believed to be a duplicate talus.
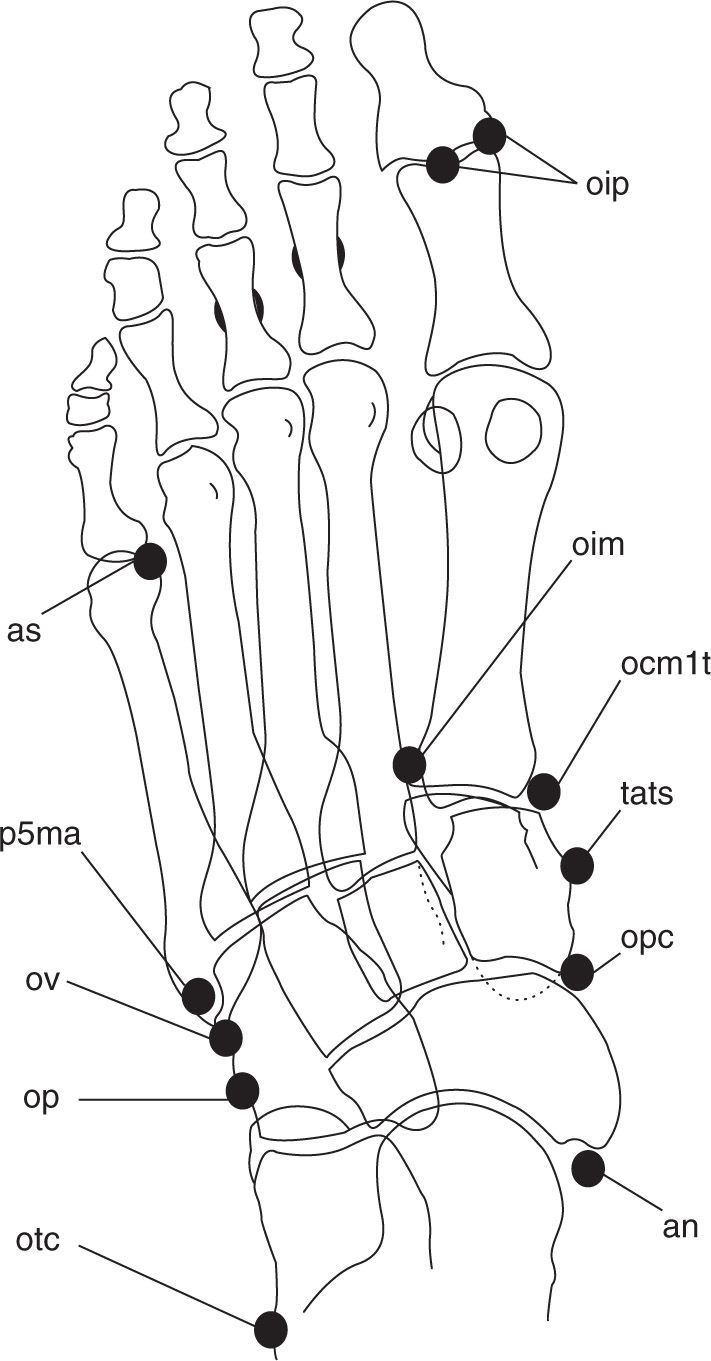
FIGURE 6-71. Dorsoplantar view of accessory ossicles. (See Box 6-2 for labels.)
SUMMARY
Figures 6-71 through 6-74 illustrate the accessory ossicles in the views that they would most likely be seen.
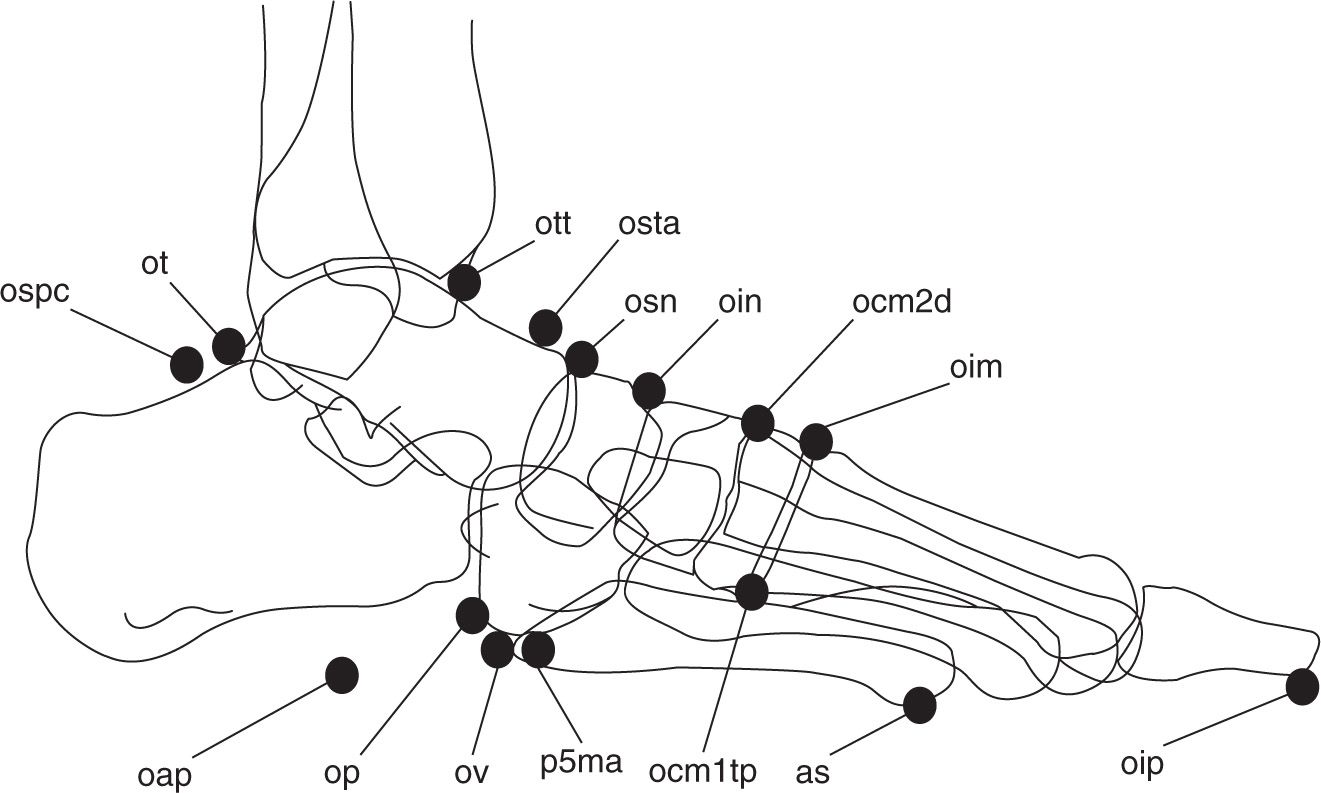
FIGURE 6-72. Lateral view of accessory ossicles. (See Box 6-2 for labels.)
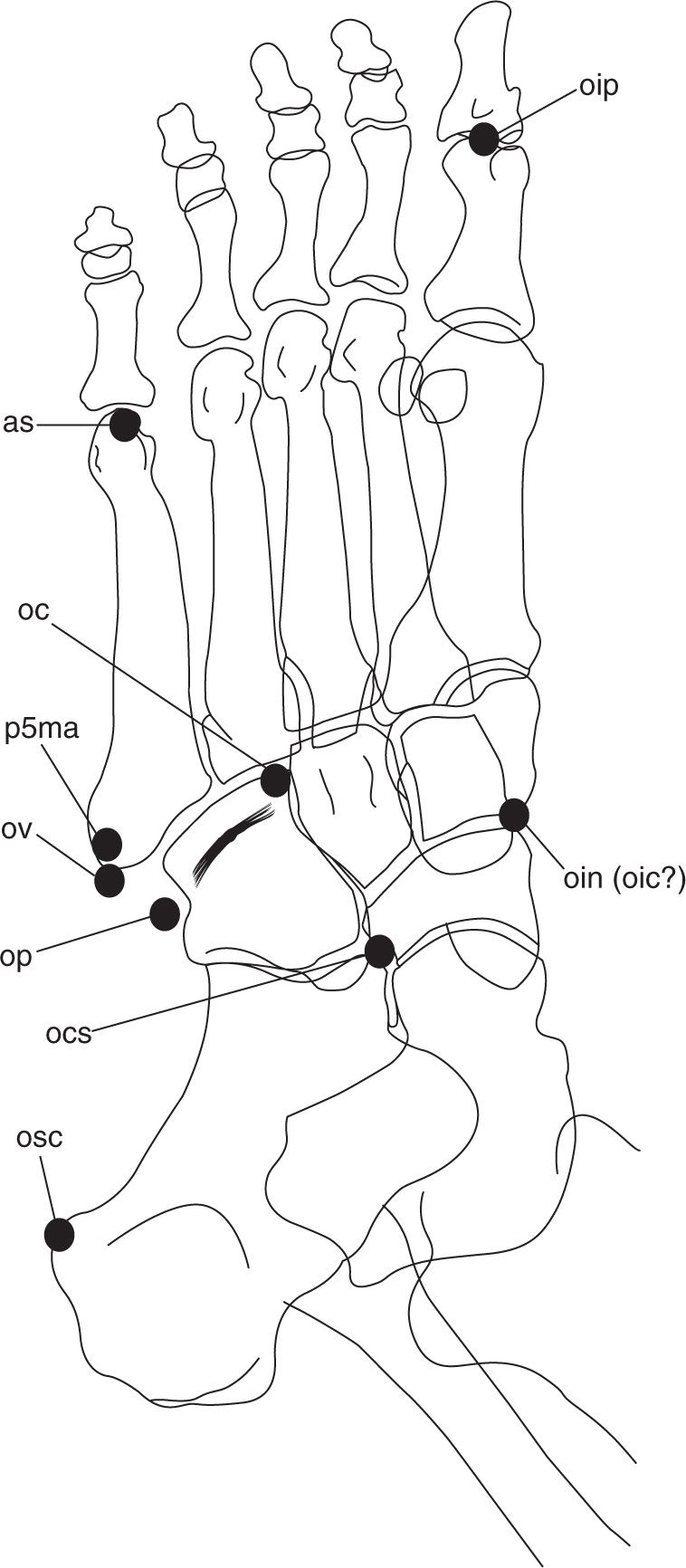
FIGURE 6-73. Medial oblique view of accessory ossicles. (See Box 6-2 for labels.)
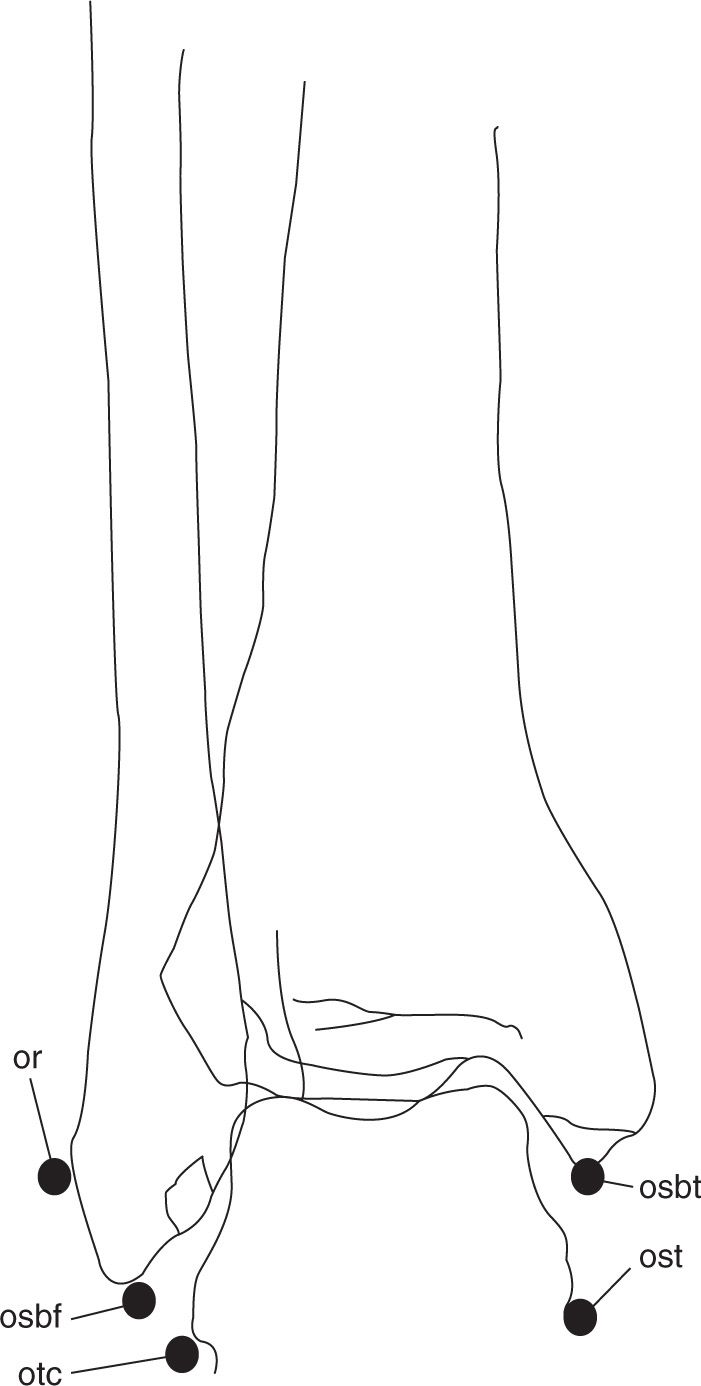
FIGURE 6-74. Anteroposterior view of accessory ossicles. (See Box 6-2 for labels.)
BOX 6-2 Labels Used in Figures 6-71 through 6-74.
an | Accessory navicular |
as | Accessory sesamoid |
oap | Os aponeurosis plantaris |
oc | Os cuboid |
ocm1tp | Os cuneometatarsale I tibiale Plantare |
ocm1t | Os cuneometatarsale I tibiale |
ocm2d | Os cuneometatarsale II dorsale |
ocs | Os calcaneus secundarius |
oic | Os intercuneiforme |
oim | Os intermetatarseum |
oin | Os infranaviculare |
oip | Os interphalangeus |
op | Os peroneum |
opc | Os paracuneiforme |
or | Os retinacula |
osbt | Os subtibiale |
osbf | Os subfibulare |
osc | Os subcalcis |
osn | Os supranaviculare |
ospc | Os supracalcaneum |
ost | Os sustentaculum tali |
osta | Os supratalare |
ot | Os trigonum |
otc | Os trochleare calcanei |
ott | Os talotibiale |
ov | Os vesalianum |
p5ma | Persistent 5th metatarsal apophysis |
tats | Tibialis anterior tendon sesamoid |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








