CRISTINA MARCHIS-CRISAN AND ROBERT A. CHRISTMAN
Several arthritides have a predilection for the foot (Box 19-1). Without question, osteoarthritis is the most common, primarily because of the mechanical wear and tear that weight-bearing activities place on cartilage. However, it is not unusual for the inflammatory rheumatic diseases (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and reactive arthritis) to first appear or be diagnosed in the feet. Furthermore, gouty arthritis and diabetic neuropathic osteoarthropathy target the foot as well. Radiography remains the initial study of choice for most rheumatic disorders.1
BOX 19-1 Joint Disorders with Predilection for the Foot
Osteoarthritis
Rheumatoid arthritis
Psoriatic arthritis
Reactive arthritis (formerly called Reiter syndrome)
Ankylosing spondylitis
Gouty arthritis
Charcot neuropathic osteoarthropathy
Septic (infectious) arthritis
The archetypal radiographic presentations of joint disorders that have been described in the literature are not necessarily what the clinician encounters in everyday practice. The patient presenting with a classic radiographic picture was probably diagnosed with the joint disease many years or even decades before. In contrast, the patient with acute symptomatology may initially come for help at the onset of disease or soon thereafter. In such a case, the radiographic findings are frequently subtle and nonspecific, the clinical findings are vague, and the diagnosis is often elusive. Furthermore, atypical cases are common. The challenge, therefore, is to identify the subtle, early radiographic findings, because the classic features of any particular joint disorder may not manifest until many years later. To maximize the detection of early arthritis, you “must know how to look, where to look, and what to look for.”2 Then, after considering clinical and laboratory findings, along with advanced imaging studies, if warranted, you must list and consider the probable differential diagnoses.
A detailed, systematic approach for radiographically evaluating joint disease in the foot entails three considerations3 (Box 19-2). For obvious reasons, the symptomatic joint or joints are assessed first. The asymptomatic joints of both extremities should also be evaluated, for two reasons: Most joint disorders target both extremities, and joints may be affected that are clinically asymptomatic. (Joint disease is one of the few pathologic conditions that justifies requesting a bilateral radiographic study.) The examination does not stop here, however. Sites distant from involved joints, osseous and soft tissue, are also considered. Abnormal findings at the calcaneal entheses and heel pain, for example, can be associated with joint disease. Finally, the distribution of radiographic findings must be assessed for specific patterns.4 Many articular disorders demonstrate characteristic patterns of joint involvement that help distinguish one disease from another.
BOX 19-2 A Systematic Approach to Evaluating Joint Disease
ROENTGEN FEATURES AT OR ADJACENT TO INVOLVED JOINTS
PRIMARY FINDINGS
Osteophyte
Osseous erosion
Subchondral resorption
Arthritis mutilans
SECONDARY FINDINGS
Bone production
Joint space alteration
Soft tissue edema, mass, calcification
Detritus
Geode
Para-articular osteopenia
Alignment abnormalities
EXTRA-ARTICULAR INVOLVEMENT OF JOINT DISEASES
Erosion
Enthesopathy
Soft tissue mass
PATTERNS OF JOINT DISEASE ACCORDING TO DISTRIBUTION OF ROENTGEN FINDINGS
Joints involved
Targeted joints
Bilateral versus unilateral
Symmetry versus asymmetry
Extra-articular sites involved
CATEGORIZATION OF THE JOINT DISORDERS
Articular disorders affecting the foot may involve one or multiple joints. Monoarticular joint disease is divided into two groups: inflammatory disease and mechanical/infiltrative disorders.1 Foot examples are generally attributed to trauma, infection, or acute gouty arthritis (Box 19-3). Less common causes in the foot include rheumatoid monoarthritis and pigmented villonodular synovitis. Polyarticular joint disorders are divided into two similar categories, inflammatory and noninflammatory. Examples affecting the foot are listed in Box 19-4.
BOX 19-3 Causes of Monoarticular Joint Disease in the Foot
INFLAMMATORY
Infectious (septic arthritis)
Crystal-induced
Gout (acute)
Pyrophosphate arthropathy
Hydroxyapatite
Systemic disease but monoarticular involvement
Rheumatoid monoarthritis
Psoriatic arthritis
Reactive arthritis
MECHANICAL/INFILTRATIVE (NONINFLAMMATORY)
Trauma
Osteonecrosis
Benign tumor
Pigmented villonodular synovitis
Osteochondroma
Differentiation of joint disorders can be simplified by applying a general classification system to the presenting features. One categorization of arthritis has been based on underlying pathologic processes: degenerative, inflammatory, and metabolic5 (Box 19-5). This classification, unfortunately, does not include Charcot neuropathic osteoarthropathy.
BOX 19-4 Polyarticular Joint Disease Affecting the Foot
INFLAMMATORY
Rheumatoid arthritis
Seronegative spondyloarthritis
Psoriatic arthritis
Ankylosing spondylitis
Reactive arthritis
Chronic tophaceous gout
NONINFLAMMATORY
Primary osteoarthritis
Charcot neuropathic osteoarthropathy
Pigmented villonodular synovitis (midfoot)
In the first edition of this textbook, Christman6 categorizes joint disorders affecting the foot as either hypertrophic or atrophic arthritis, based on predominant radiographic features (Box 19-6). As far back as 1904 these terms were used to distinguish between osteoarthritis and rheumatoid arthritis.7 Hypertrophic joint disease features bone overgrowth and enlargement. The characteristic findings are subchondral sclerosis and osteophyte formation at the joint margin. Detritus arthritis, a subcategory of hypertrophic arthritis, includes those disorders that exhibit fragmentation in addition to exaggerated hypertrophic features.
BOX 19-5 Categories of Joint Disease (Based on Underlying Pathology)
DEGENERATIVE
Osteoarthritis
INFLAMMATORY
Rheumatoid arthritis
Seronegative spondyloarthritis
Psoriatic arthritis
Reactive arthritis
Ankylosing spondylitis
Septic arthritis
METABOLIC
Gouty arthritis
Pyrophosphate arthropathy
The loss of bone substance, primarily through erosion, and joint space narrowing, with or without periarticular osteoporosis, characterize the atrophic joint disorders. A subdivision of this group is commonly associated clinically with an adjacent soft tissue mass and the preservation of joint space; the term “lumpy-bumpy” joint disease has been used to characterize this group.8
BOX 19-6 Categories of Joint Disease (Based on Radiographic Features)
HYPERTROPHIC JOINT DISEASE
Osteoarthritis (primary)
Detritus arthritis
Tarsus and midfoot Charcot neuropathic osteoarthropathy
Posttraumatic arthritis
ATROPHIC JOINT DISEASE
Rheumatoid arthritis
Seronegative spondyloarthritis
Psoriatic arthritis
Ankylosing spondylitis
Reactive arthritis
Septic arthritis
Forefoot Charcot neuropathic osteoarthropathy
“Lumpy-bumpy” joint disease
Gouty arthritis
Multiple reticulohistiocytosis
Pigmented villonodular synovitis
Charcot neuropathic osteoarthropathy is divided into two subtypes: forefoot and the combined midfoot and tarsus. The radiographic features vary depending on location: Forefoot sites exhibit findings characteristic of atrophic joint disease; the midfoot and tarsal sites display features of detritus (hypertrophic) arthritis.
Since the first edition, Christman has developed a new categorization for joint disorders in the foot based upon four primary radiographic findings: osteophyte, erosion, subchondral resorption, and arthritis mutilans (Box 19-7). The joint disorders are then further distinguished by secondary (associated) findings, including joint space alteration, soft tissue abnormality, bone production, bone loss, and detritus (Box 19-8). This system is valuable for the process of differentiation between the disorders.
BOX 19-7 Categories of Joint Disease (Based on the Primary Radiographic Finding)
OSTEOPHYTE
Osteoarthritis
EROSION
Rheumatoid arthritis
Seronegative spondyloarthritis
Psoriatic arthritis
Ankylosing spondylitis
Reactive arthritis
Gouty arthritis
SUBCHONDRAL RESORPTION
Charcot neuropathic osteoarthropathy
Septic arthritis
ARTHRITIS MUTILANS
Psoriatic arthritis
Charcot neuropathic osteoarthropathy (forefoot only)
Rheumatoid arthritis (fifth MPJ only)
Each of the roentgen features associated with joint disease is discussed individually in the following section. Remember the radiographic categories of joint disorders; you can recognize associations between certain roentgen findings and arthritis categories, improving your diagnostic acumen.
RADIOGRAPHIC FINDINGS IN JOINT DISEASE OF THE FOOT
Primary Radiographic Findings
Osteophyte
An osteophyte is a spur at the margin of a joint (Figure 19-1). Numerous figurative terms have been applied to this lesion, including dorsal flag (along the first metatarsal head), lipping (if at both sides of the joint, especially intertarsal), and beaking (along the talar head). However, the talar beak may not truly represent an osteophyte; its location is between the articular margins of the talonavicular and talocrural joints, where a ridge is normally found.9 The presence of an osteophyte is pathognomonic of osteoarthritis.
BOX 19-8 Joint Disease Secondary Findings
BONE PRODUCTION
Periostitis
Whiskering; ivory phalanx (hallux distal phalanx)
Subchondral sclerosis (eburnation)
Diffuse sclerosis
Overhanging margin (Martel sign)
JOINT SPACE ALTERATION
Narrow: uneven vs. even
Normal
Wide
SOFT TISSUE ABNORMALITY
Increased volume/density: joint effusion versus “sausage toe”
Mass: “lumpy-bumpy” vs. fusiform
Calcification
DETRITUS
Loose body (“joint mouse”)
Fragmentation
GEODE (WITH OR WITHOUT SCLEROTIC MARGIN)
PARA-ARTICULAR OSTEOPENIA
ALIGNMENT
Less than 100% apposition
Misalignment
Osseous Erosion
Erosion is a localized wearing away of bone that begins along its outer surface. It has varying appearances, which are helpful when determining whether or not the associated pathology is acute as well as distinguishing between diseases (Box 19-9). It is the primary feature of all joint disorders affecting the foot except osteoarthritis, Charcot neuropathic osteoarthropathy, and septic arthritis. Generally speaking, the early appearance of erosion is small, ill-defined, and irregular (Figure 19-2). This characterization contrasts with the larger, well-defined C-shaped erosion classically seen in the disorders associated with an adjacent soft tissue mass (Figure 19-3). The presence of erosion excludes osteoarthritis as a primary diagnosis; however, geodes (or subchondral bone cysts, which are a secondary finding of osteoarthritis) and trauma-induced subchondral bone defects can mimic the appearance of erosion (Figure 19-4).
BOX 19-9 Presentations of Erosion
PREEROSION (SUBCHONDRAL BONE PLATE)
“Dot-dash” appearance
“Skip pattern”
MARGIN
Ill-defined
Well-defined
With or without sclerotic margin
LOCATION
Periarticular (extra-articular)
Intra-articular
Medial vs. lateral vs. both
WITH OR WITHOUT JOINT SPACE NARROWING
WITH OR WITHOUT ASSOCIATED NEW BONE PRODUCTION

FIGURE 19-1. Osteophyte (osteoarthritis). A: “Flagging” along dorsum of first metaratsal head. B: “Lipping” at intermediate naviculocuneiform joint (arrows) and “beaking” at the talar ridge (arrowhead), probably not a true osteophyte.
Erosion is an early finding in the course of most inflammatory joint diseases. It is usually intra-articular and typically begins along the medial and/or lateral margins of the joint. Between where the cartilage ends and the joint capsule inserts is a bony surface covered only by periosteum or perichondrium; this surface is in contact with the synovium and its fluid and is known as the “bare” area.4 The inflamed synovium, known as pannus, invades the bare area; on a radiograph, the outer margin of subchondral bone quickly disappears. Initially this disappearance may be as subtle as a “dot-dash” appearance or “skipping” along the thin white line that comprises the subchondral bone plate (Figure 19-5). Eventually the localized loss of marginal bone (decreased density) progresses so far that the form of the affected bone appears abnormal. These findings may be recognized days or weeks after the onset of symptoms and contribute to the erosion’s ill-defined and irregular appearance.
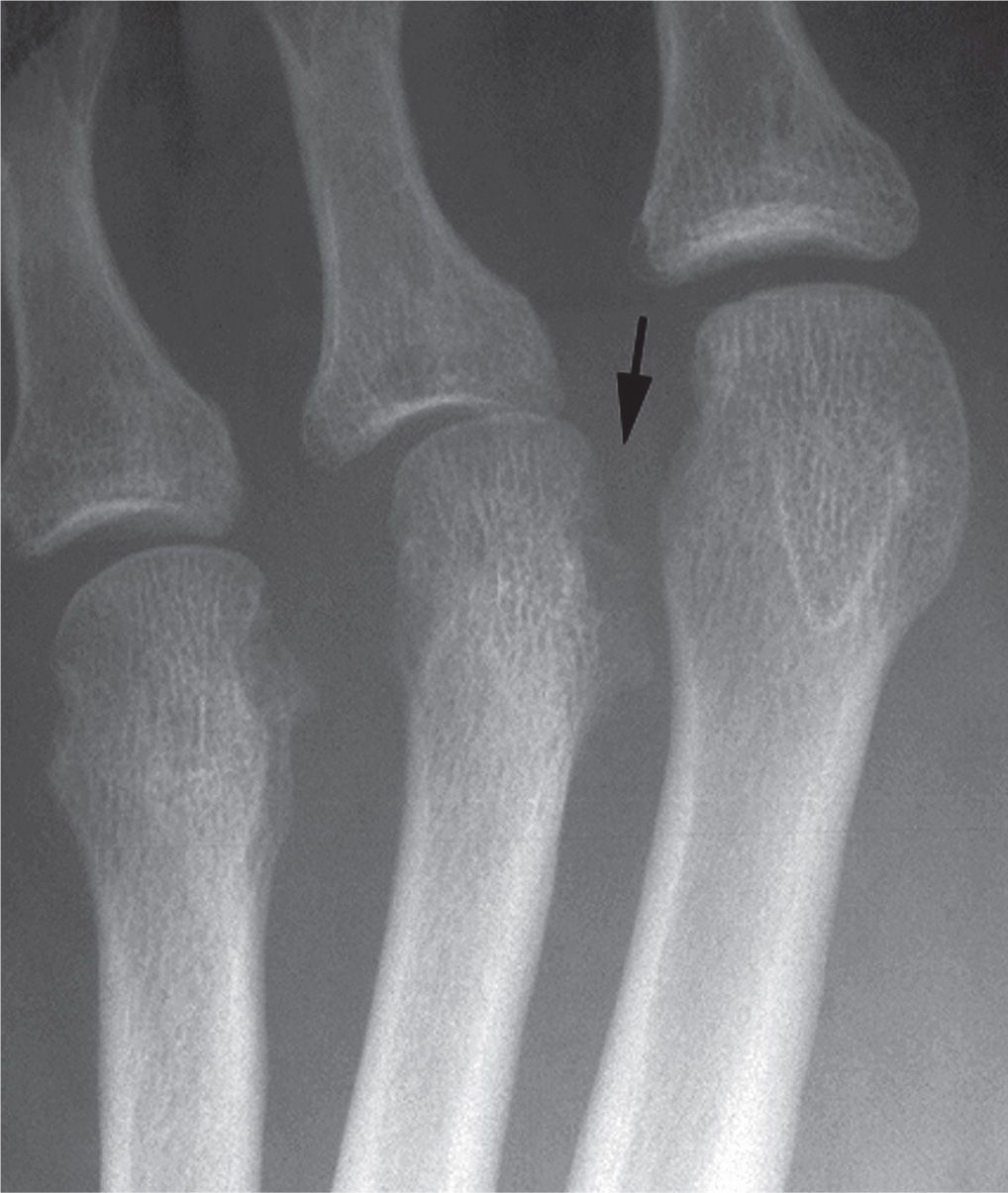
FIGURE 19-2. Irregular, ill-defined erosion (arrow) (ankylosing spondylitis).

FIGURE 19-3. Well-defined, C-shaped erosion (gouty arthritis).
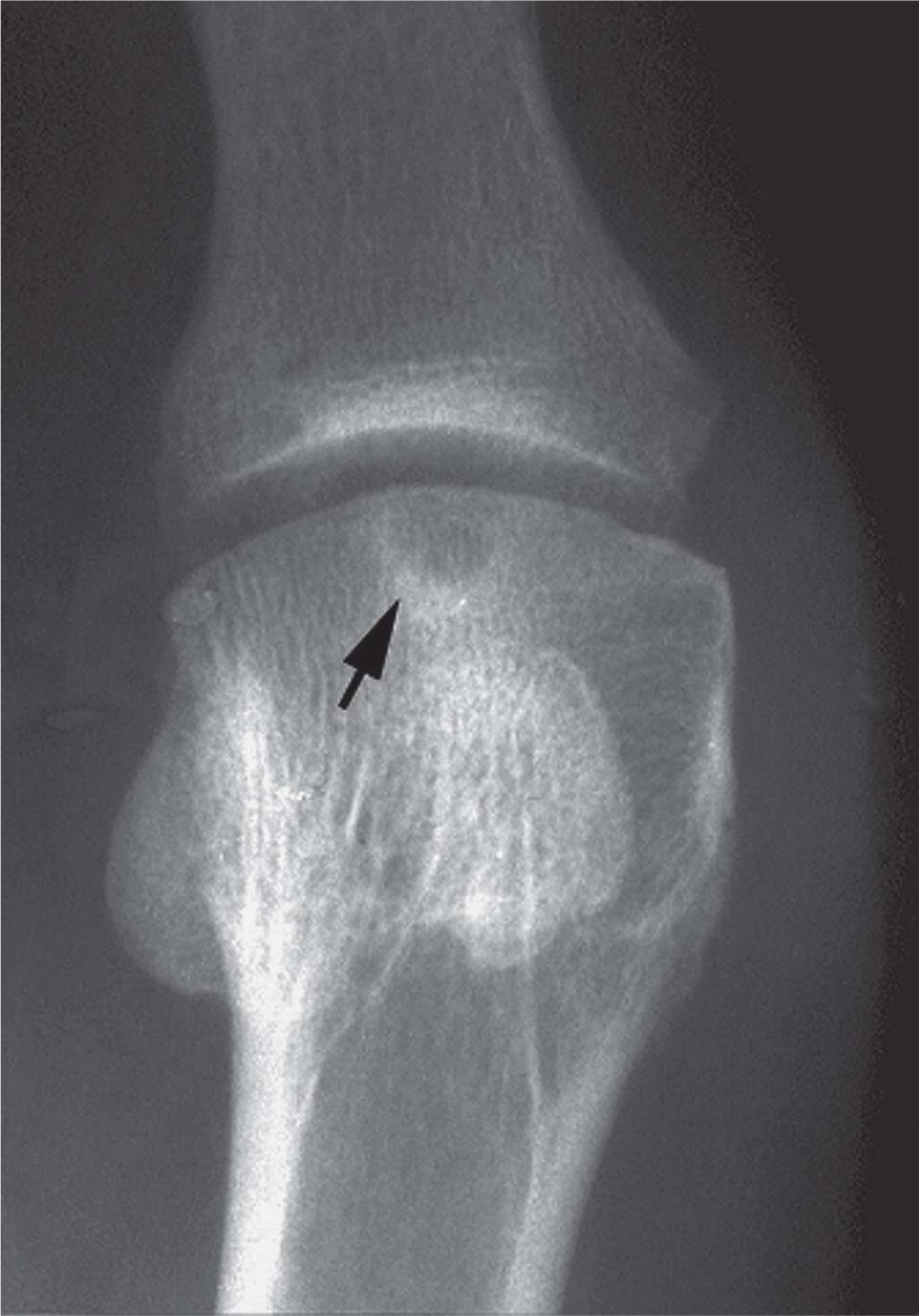
FIGURE 19-4. Subchondral geode (arrow) mimicking an erosion (osteoarthritis).
The well-defined erosion, in contrast, appears radiographically several months or years after the initial onset of symptoms. It frequently results from chronic pressure atrophy secondary to direct apposition of a soft tissue mass with concomitant infiltration and replacement of bone (Figure 19-3). Or, it may result months or years after acute, ill-defined erosion remodels.
Subchondral Resorption
The subchondral bone plate is the thin white line at an articular margin; it is where the cartilage ends and bone begins. Normally it is well-defined and continuous (Figure 19-5). Subchondral resorption typically involves the central portion of the joint, in contrast to erosions that are marginal. There are three presentations (Box 19-10): disappearance of the subchondral bone plate centrally; the subchondral bone plate is visible but there is rarefaction of bone immediately adjacent to it, which may appear as early osteolysis; and a combined presentation that demonstrates loss of the bone plate and rarefaction (osteolysis) (Figure 19-6). Subchondral resorption is the primary radiographic feature of septic arthritis and Charcot neuropathic osteoarthropathy.
BOX 19-10 Presentations of Subchondral Resorption
Disappearance of subchondral bone plate centrally
Visibility of subchondral bone plate but rarefaction of bone is immediately adjacent to it
Loss of subchondral bone plate and rarefaction/osteolysis

FIGURE 19-5. Early erosion: dot-dash or skip pattern, second metatarsal head (arrowheads). Compare it to the obvious erosion of the third metatarsal head and the normal subchondral bone plate of the fourth metatarsal head (rheumatoid arthritis). Also note the geode in the center of the third metatarsal head and narrowing of the third metatarsophalangeal joint.
Arthritis Mutilans
Erosions that involve both margins (medial and lateral) of any metatarsophalangeal or interphalangeal joint (IPJ) proximally accompanied by central resorption of the adjacent phalangeal base can result in a condition known as arthritis mutilans. Also called resorptive arthropathy, arthritis mutilans is characterized by concentric bone resorption and primary joint destruction (osteolysis), and has a very characteristic radiographic picture (Figure 19-7).5 Bone resorption may even expand to include the nearby metadiaphyseal cortex. This has figuratively been described by several terms, most commonly the “pencil-in-cup” deformity. Other terms used to describe arthritis mutilans are listed in Box 19-11. Arthritis mutilans has characteristically been associated with psoriatic arthritis (Figure 19-7). However, forefoot Charcot neuropathic osteoarthropathy (Figure 19-8) and, to a lesser degree, rheumatoid arthritis at the fifth metatarsophalangeal joint (Figure 19-9) present similar pictures.
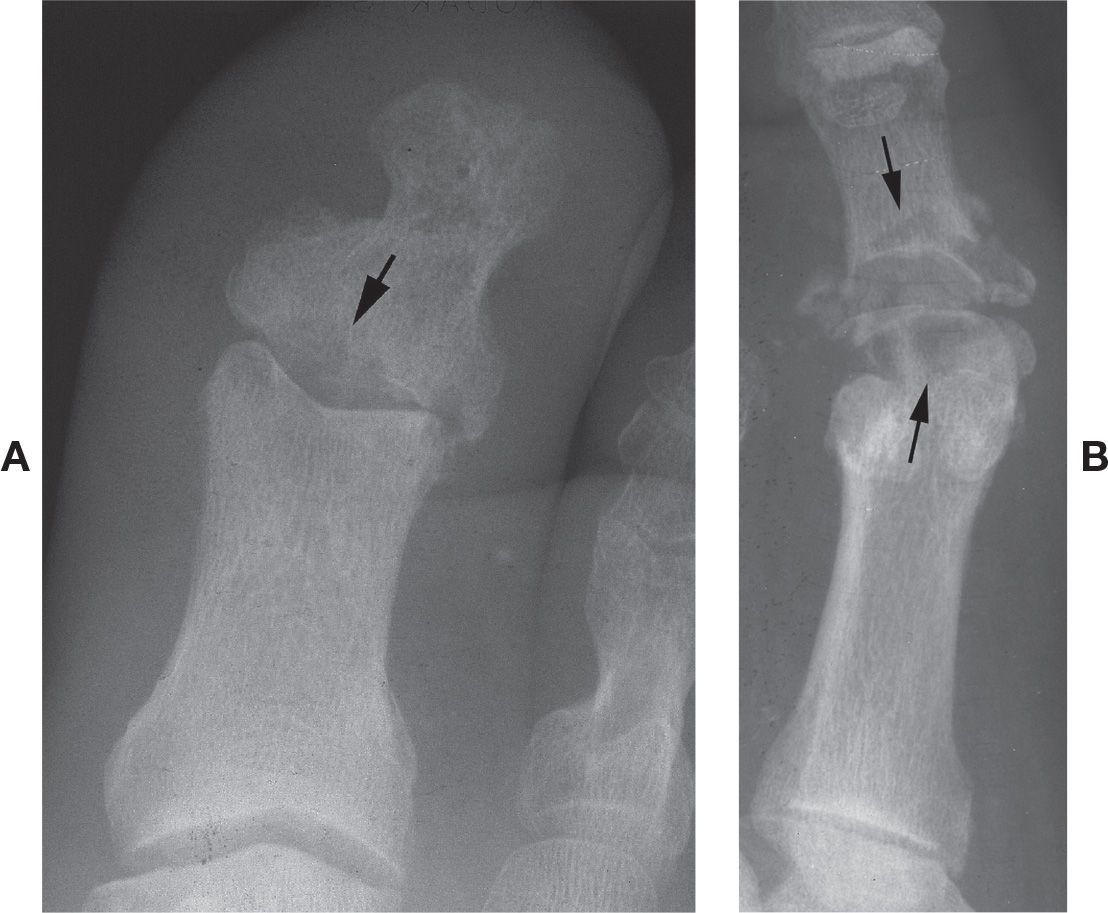
FIGURE 19-6. Subchondral resorption. A: Central (arrow) (septic arthritis). B: Rarefaction adjacent to subchondral bone plate (arrows) and osteolysis (Charcot neuropathic osteoarthropathy) (B: Courtesy of Philip Bresnahan, DPM.)
BOX 19-11 Arthritis Mutilans Figurative Terms
Pencil-in-cup deformity
Mortar and pestle
Sucked candy stick
Whittling
Pencil sharpening
Secondary Radiographic Findings
Bone Production
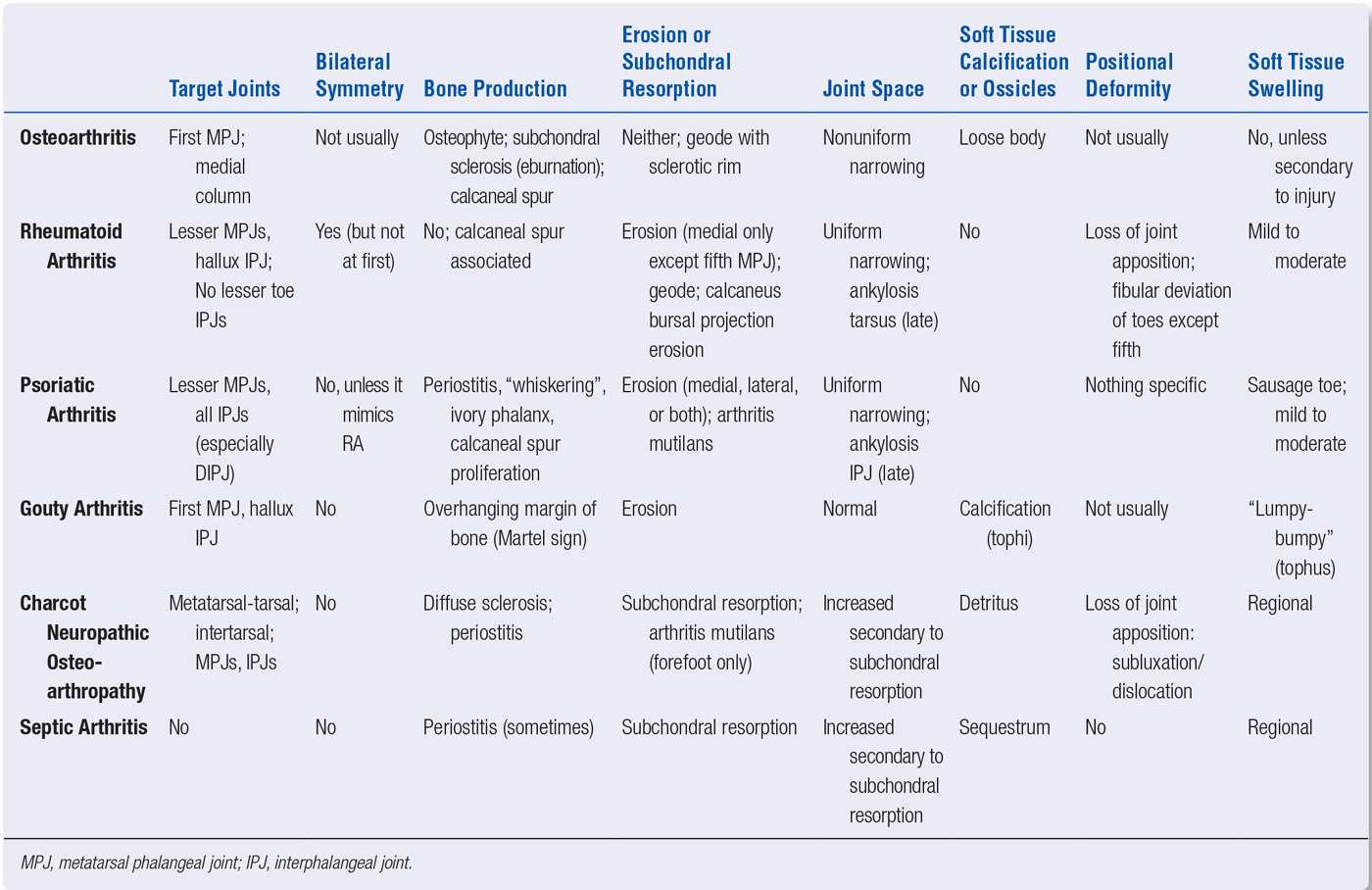
Aside from the osteophyte, other forms of bone production may be associated with the primary radiographic findings listed earlier. The presence or absence of secondary findings can further narrow down the differential diagnoses. For example, new bone production is rarely seen at joints affected by rheumatoid arthritis. However, periostitis is frequently seen with seronegative spondyloarthritis, and an overhanging margin of new bone is associated with the C-shaped erosions encountered with gouty arthritis (Table 19-1).

FIGURE 19-7. Arthritis mutilans: psoriatic arthritis.

FIGURE 19-8. Arthritis mutilans: neuropathic osteoarthropathy.

FIGURE 19-9. Arthritis mutilans: rheumatoid arthritis (fifth metatarsophalangeal joint).
| Forms of Bone Production and Associated Joint Disorders |
Form of Bone Production | Differential Diagnosis |
Osteophyte (dorsal flag, lipping, beaking) | Osteoarthritis |
Subchondral sclerosis (eburnation) | Osteoarthritis |
Diffuse sclerosis | Charcot neuropathic osteoarthropathy (midfoot and tarsus) |
Periostitis | Seronegative spondyloarthritis (IPJ or MPJ) Psoriatic (also whiskering type) Septic arthritis Charcot neuropathic osteoarthropathy (forefoot) |
Overhanging margin of bone (Martel sign) | Gouty arthritis |
Ivory phalanx | Psoriatic arthritis (distal phalanx hallux) |
IPJ, interphalangeal joint; MPJ, metatarsophalangeal joint.
Subchondral sclerosis, also referred to as eburnation (Figure 19-10), is an ill-defined increased density found in periarticular bone. It is commonly associated with posttraumatic osteoarthritis.

FIGURE 19-10. Osteoarthritis, first metatarsophalangeal joint. Osteophytes (white arrows) and subchondral sclerosis (black arrows).
Diffuse sclerosis involving an entire bone is associated with the repair and remodeling phases of Charcot neuropathic osteoarthropathy in the tarsus (Figure 19-8).
The presence of periostitis near the metaphysis of a symptomatic metatarsophalangeal or interphalangeal joint is highly suggestive of seronegative arthritis (Figure 19-11). Unfortunately the periostitis is short-lived: Within a few weeks it quickly remodels and becomes continuous with the bony margin. Periostitis may also be seen with septic arthritis and forefoot Charcot neuropathic osteoarthropathy; the latter is difficult to differentiate from infection.
A variation of periostitis seen particularly with psoriatic arthritis is referred to as “whiskering”10; its spiculated appearance radiates away from the bone margin. It characteristically involves the hallux and, less frequently, the lesser digit distal phalanges (Figure 19-12). Ill-defined bony sclerosis frequently accompanies this finding. Whiskering appears to represent concomitant new bone formation and erosion at the capsular and ligamentous entheses.
Occasionally the distal phalanx of an affected digit becomes quite radiodense or sclerotic relative to normal bone density. This is seen especially in the hallux (Figure 19-13). Known as the “ivory” phalanx, it is another presentation associated, in the proper clinical setting, with psoriatic arthritis.11
The well-defined erosions of chronic gouty arthritis occasionally have an overhanging margin of bone (Figure 19-14). This finding, described by Martel,12 represents new bone production at the margin of erosion. The body seems to be responding to the presence of the tophus and attempting to encapsulate it or wall it off. Its presence strongly suggests gouty arthritis.13 Another finding sometimes associated with the developing erosion of gouty arthritis is ill-defined surrounding sclerosis, which may become well-defined over time.
Joint Space Alteration
The joint space seen radiographically corresponds to the cartilage lining each bony surface. Kaye14 has correlated three types of joint space alteration with the articular disorders: narrowing, normal, and widening (Table 19-2).
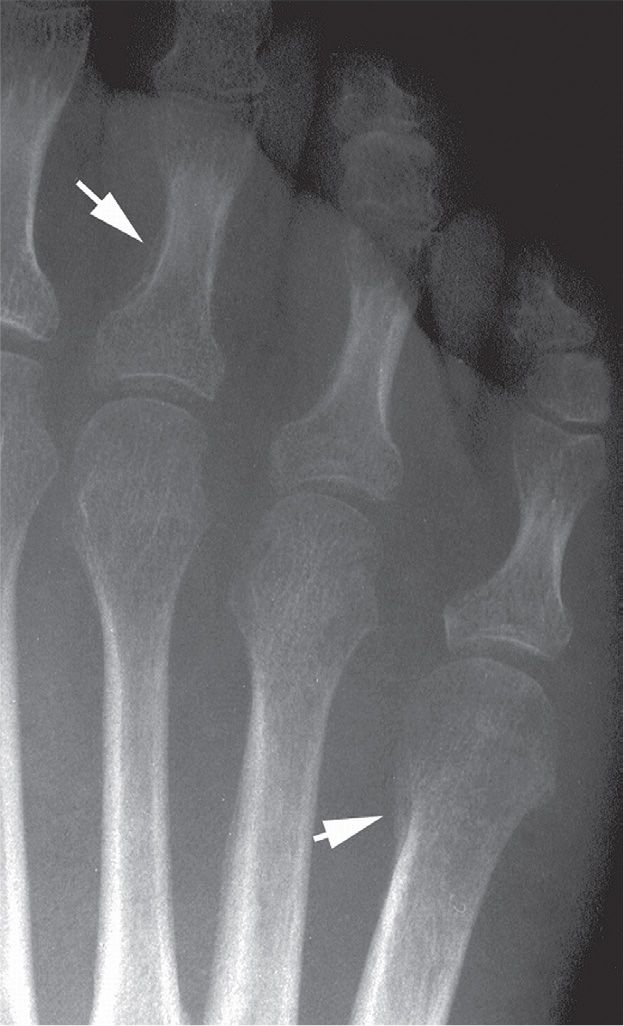
FIGURE 19-11. Psoriatic arthritis: periostitis (arrows).
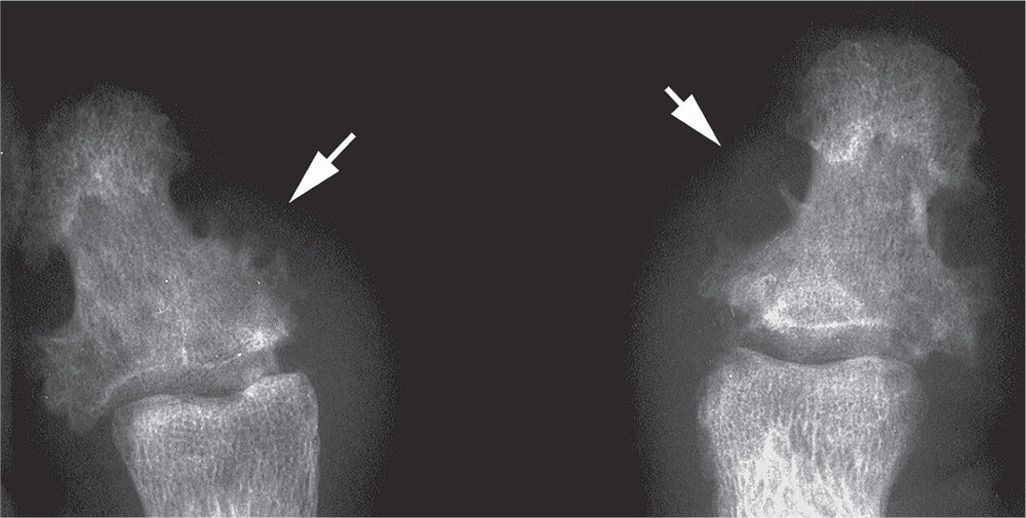
FIGURE 19-12. Psoriatic arthritis: whiskering (arrows) of hallux distal phalanx, bilateral.
Erosion or lysis of articular cartilage eventually appears as joint space narrowing radiographically, as the two opposing surfaces converge. This is an early radiographic finding of rheumatoid arthritis but is seen eventually in most joint disorders.
Joint space narrowing may be either even or uneven. The narrowing seen with inflammatory arthritis usually is even or uniform across the joint (Figure 19-15). This is because inflammatory pannus is distributed throughout the joint and affects all cartilage. In contrast, osteoarthritis secondary to wear and tear or trauma usually only involves one section of the cartilage or subchondral bone, not the entire surface; as a result, joint space narrowing has an uneven or nonuniform presentation radiographically (Figure 19-16). The unaffected joint section has normal spacing.
The presence of a normal joint space associated with periarticular erosion is characteristic of joint disorders associated with soft tissue masses (Figure 19-17). Chronic tophaceous gout, for example, is not primarily an inflammatory disorder. Although intense inflammation is clinically seen with acute attacks of gout, these symptoms last only a short period of time. Several years may lapse before radiographic evidence of erosion is evident. Furthermore, since erosion associated with gouty arthritis is commonly periarticular, that is, outside the joint capsule, cartilage may not be directly involved until much later in the course of disease. As a result, the presence of normal joint space in light of obvious erosion is a characteristic finding. This is in strict contrast to inflammatory joint disease. The aggressive nature of this latter group of disorders and associated intense synovitis quite rapidly cause bone and cartilage destruction.

FIGURE 19-13. Psoriatic arthritis: ivory phalanx.
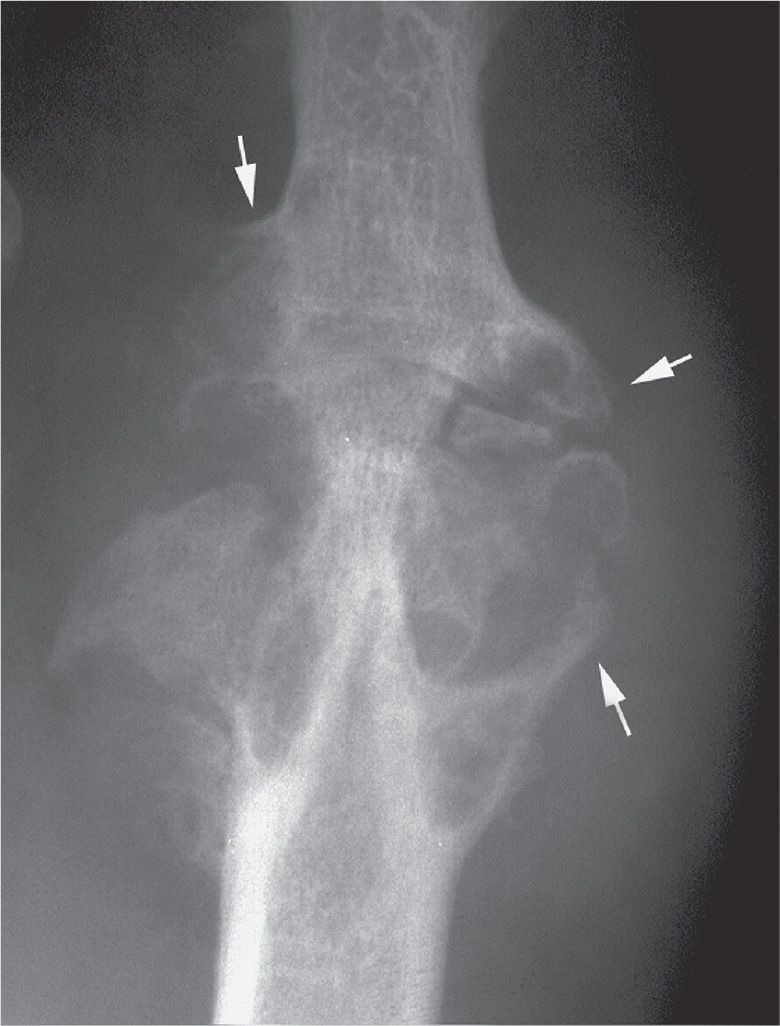
FIGURE 19-14. Gouty arthritis: overhanging margin of bone (arrows) (Martel sign).
Bony or fibrous ankylosis may occur between two bones as an end stage of some joint diseases. This is especially true of the inflammatory joint disorders. Bony ankylosis is more commonly associated with seronegative arthritis. The interphalangeal joints are targeted in psoriatic arthritis (Figure 19-18A). Midfoot ankylosis may be seen in the rheumatoid foot (Figure 19-18B). Ankylosis is seldom seen with gouty arthritis and is not associated with pedal osteoarthritis. However, the superimposition of osteophytes and joint space narrowing may simulate bony ankylosis.
| Grouping of Joint Disease Based on Joint Space Alteration (Modified Kaye Classification9) |
Joint Space |
| Arthritis |
Narrowing | Uniform | Inflammatory arthritis (rheumatoid) |
| Nonuniform | Degenerative arthritis (osteoarthritis) Posttraumatic arthritis Septic arthritis |
| Ankylosis (end stage) | Seronegative spondyloarthritis (IPJ) Midfoot rheumatoid arthritis |
Normal or near normal joint space |
| Gouty arthritis |
Widening | Uniform | Early inflammatory arthritis (with acute synovitis) |
| Nonuniform | Early psoriatic arthritis (extensive erosion with fibrous tissue deposition) |
IPJ, interphalangeal joint.
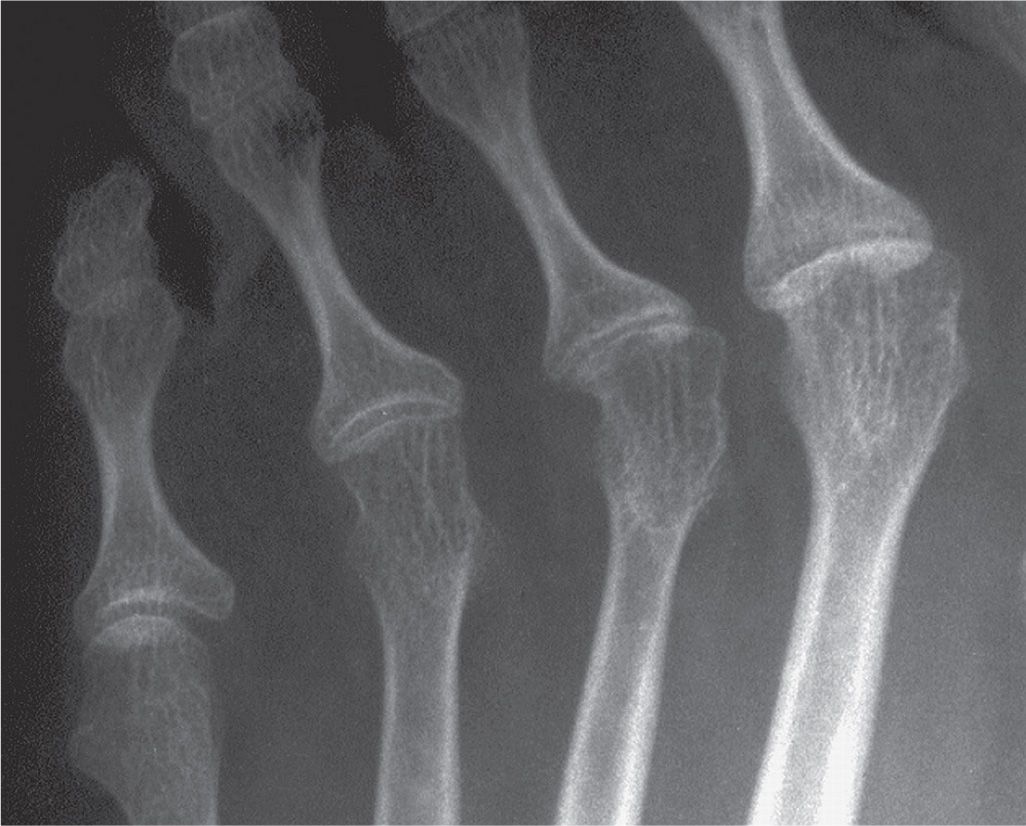
FIGURE 19-15. Rheumatoid arthritis: even joint space narrowing.
Excess fluid accumulates in a joint that is acutely inflamed. To accommodate this fluid, the capsule becomes stretched and the opposing bones are distracted. Radiographically, this may appear as widening of the joint space (Figure 19-19A). Unfortunately, joint space widening secondary to acute synovitis can be a very subtle finding. Furthermore, the finding is short-lived; its radiographic presence is a hit-or-miss incident.

FIGURE 19-16. Osteoarthritis: uneven joint space narrowing. Other findings include osteophytes and geodes.

FIGURE 19-17. Gout: sparing of joint space despite erosive disease. Faint tophus calcification (arrow) is noted medial to the erosion.
Extensive resorption of subchondral bone also gives the appearance of joint space widening (Figure 19-19B). Resorption and subsequent fibrous tissue deposition between bones contribute to the widening seen in psoriatic arthritis.3
Soft Tissue Edema, Mass, and Calcification
Soft tissue edema may be generalized throughout the foot, regional (forefoot, midfoot, rearfoot, or a toe), or localized to a joint or extra-articular site (Table 19-3). It is viewed radiographically as an increased soft tissue density and/or volume relative to normal expectation.
Generalized soft tissue edema can be related to abnormal systemic conditions (cardiac disease, acromegaly), diffuse inflammatory states (cellulitis), or peripheral vascular disease (venous insufficiency, lymphedema).5 It is not, however, a specific finding in joint disease. Many patients with pedal joint disease have concomitant generalized soft tissue edema that is secondary to the conditions just noted.
Regional soft tissue edema is confined to a smaller segment of the body. An entire digit, for example, may be edematous from acute inflammatory conditions including infection, seronegative arthritis (the so-called sausage toe), and gout. The edema associated with an acute gouty attack at the first metatarsophalangeal joint may extend to the midfoot. This clinical presentation may certainly mimic an infectious process. Posttraumatic states also can show regional soft tissue edema. Neuropathic osteoarthropathy of the midfoot and tarsus shows either regional or diffuse edema.
Localized soft tissue edema may be related to synovial inflammation or to a mass. The edema associated with synovitis surrounds the joint and is quite well-defined radiographically. Increased soft tissue density and volume secondary to synovitis is known as joint effusion. This condition, although nonspecific, is highly associated with inflammatory joint disease. However, synovitis secondary to trauma, either acute or chronic and repetitive, can appear radiographically identical to that caused by inflammatory rheumatic disease (rheumatoid and seronegative arthritis).
Periarticular soft tissue masses are associated with a few joint disorders (Table 19-4). The most common example is the gouty tophus. Tophi are well-defined masses that are found adjacent to joints or at extra-articular sites (Figure 19-20). They occasionally exhibit calcification. Lesions are distributed asymmetrically in the foot.
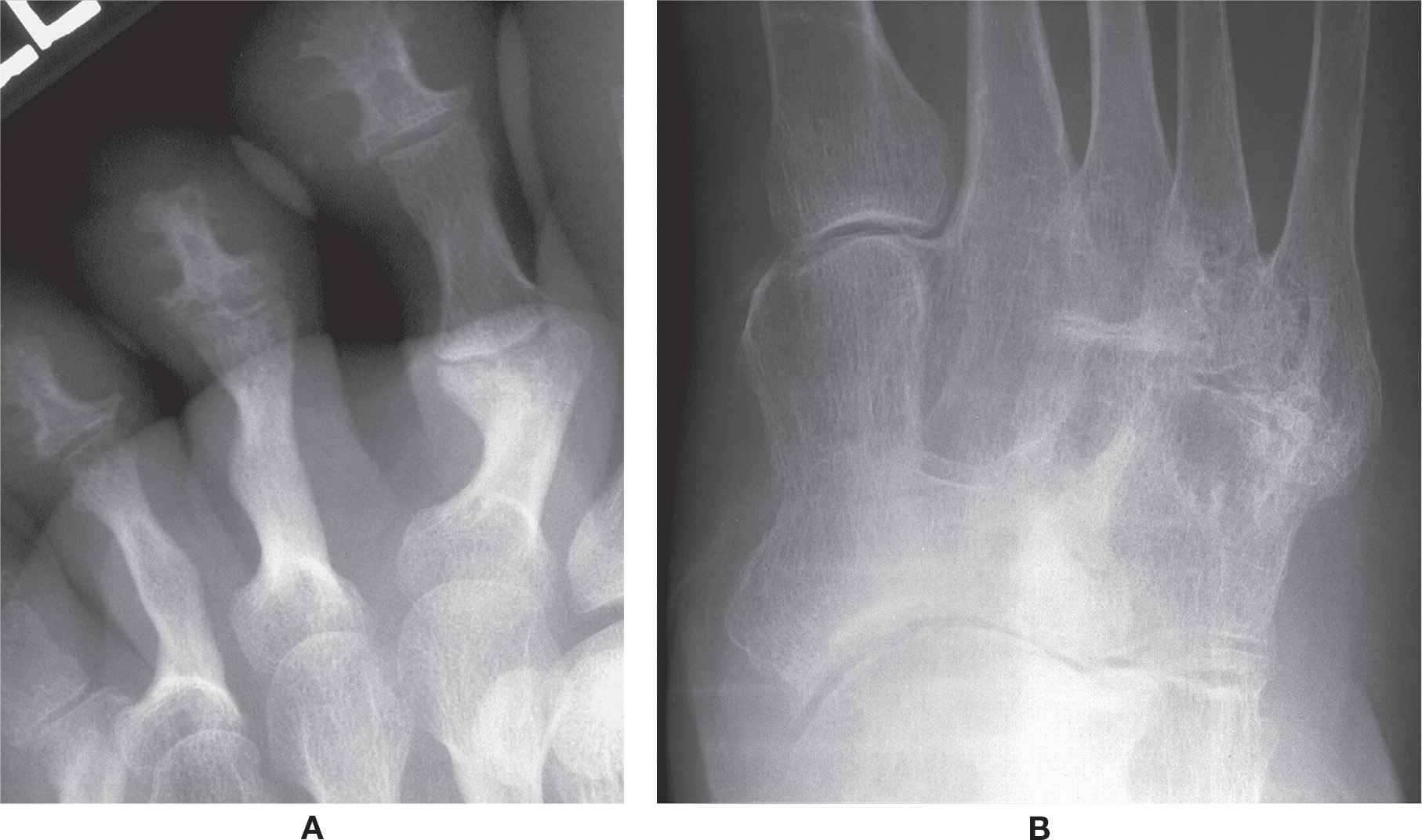
FIGURE 19-18. Bony ankylosis: A: Psoriatic arthritis. B: Rheumatoid arthritis.

FIGURE 19-19. Joint space widening: A: Secondary to inflammatory exudate (septic arthritis). B: Secondary to central erosion (psoriatic arthritis).
Tophi may be seen several years after the initial onset of symptoms. They are a characteristic feature of chronic tophaceous gout; erosions develop adjacent to tophi. It has been reported that the clinical presence of tophi are strongly associated with the characteristic radiographic features of gouty arthritis.15
Another soft tissue erosive joint disorder is multiple reticulohistiocytosis. These masses radiographically appear similar to those seen in gout. However, masses associated with multiple reticulohistiocytosis are widespread, symmetric, and do not calcify.
Soft tissue masses are occasionally seen with rheumatoid arthritis. Rheumatoid nodules are seldom found in the foot but, when present, may radiographically appear indistinguishable from a gouty tophus except that the former rarely calcifies.16
Soft tissue tumors and tumor-like lesions may manifest in periarticular locations and cause articular erosions. Although not common, an example of one such lesion occurring in the foot is pigmented villonodular synovitis. As a rule, it is monoarticular. However, a rare, polyarticular (diffuse) manifestation can appear in the midfoot (Figure 19-21). This is probably related to the unique synovial compartmentalization in this anatomic region. Well-defined erosions develop adjacent to soft tissue masses.
| Grouping of Joint Disease Based on Soft Tissue Edema Classification |
Soft Tissue Edema | Arthritis |
Generalized/diffuse | None |
Regional | Seronegative spondyloarthritis (“sausage toe”) Gouty arthritis (acute) Septic arthritis (acute) Charcot neuropathic osteoarthropathy (midfoot/tarsus) |
Localized | Posttraumatic arthritis Inflammatory (rheumatoid or seronegative spondyloarthritis) |
Numerous disorders are associated with soft tissue calcification in the foot. Widespread soft tissue calcification in otherwise normal tissues is associated with disorders that demonstrate elevated calcium or phosphate levels in the serum. Hyperparathyroidism, for example, may cause diffuse periarticular, capsular, and vessel calcification. The majority of soft tissue calcifications seen in the foot, however, are probably dystrophic or idiopathic. Dystrophic calcifications occur in soft tissues that are damaged or altered but have no underlying disturbance in calcium or phosphorus metabolism.17,18
Soft tissue calcifications, when associated with joint disease, may be diagnostic for a group of disorders known as the crystal deposition diseases (Table 19-5). The crystals are monosodium urate (MSU) (gouty arthritis), calcium pyrophosphate dihydrate (CPPD), and hydroxyapatite (HA). Calcifications can be found in the periarticular tissues, joint capsule, or cartilage.
| Characteristics of Erosive Joint Disorders with Associated Soft Tissue Mass |
Joint Disorder | Soft Tissue Mass Characteristics |
Chronic tophaceous gout | Well-defined (lumpy-bumpy); articular and/or periarticular; asymmetric; occasionally calcifies |
Multiple reticulohistiocytosis | Widespread; periarticular; symmetric; no calcification |
Rheumatoid arthritis | Well-defined (fusiform); extra-articular; asymmetric; rarely calcifies |
Pigmented villonodular synovitis | Well-defined; articular or periarticular; asymmetric; two presentations: monoarticular (nodular) and diffuse; no calcification |

FIGURE 19-20. Gout: tophus at hallux interphalangeal joint (arrows).
The crystals associated with gouty arthritis may be deposited in the joint capsule, synovium, cartilage, subchondral bone, or periarticular tissues.19 In the foot, radiographic visualization of calcified crystals is best appreciated in the periarticular soft tissues. A collection of MSU crystals in the soft tissue is known as a tophus. Tophus calcification is occasionally seen with chronic tophaceous gout. Although not a pathognomonic finding, calcification of a periarticular soft tissue mass, especially if situated adjacent to erosion, is highly suggestive of gouty arthritis in the proper clinical setting. Small, punctate calcifications can be identified in the soft tissue mass (Figure 19-22).

FIGURE 19-21. Pigmented villonodular synovitis, tarsus. There are multiple, well-defined C-shaped erosions adjacent to the soft tissue mass.
| Characteristics of Joint Diseases Associated with Soft Tissue Calcifications |
Arthritis | Crystal Deposited | Location/Characteristics |
Gouty arthritis | Monosodium urate | Periarticular soft tissues (tophus); joint capsule; synovium; cartilage; subchondral bone Small, punctate calcifications |
Pyrophosphate arthropathy | Calcium pyrophosphate dihydrate (CPPD) | Cartilage (chondrocalcinosis); periarticular soft tissue of MPJ, tarsal, and ankle joint. Curvilinear calcifications parallel subchondral bone plate |
HADD | Hydroxyapatite | Periarticular, including tendons, and bursae. Calcifying tendonitis Small punctate calcifications vs. large, amorphous calcification adjacent to a joint |
Calcium pyrophosphate dihydrate (CPPD) deposition disease is associated with several patterns of joint involvement.20 In general, radiographic features include joint space narrowing, subchondral sclerosis, and loose osseous bodies; these collective findings are known as pyrophosphate arthropathy when associated with CPPD deposition.21 Calcifications can occur in articular and periarticular soft tissues. However, cartilage calcification, or chondrocalcinosis, has received the most attention. The primary crystal associated with chondrocalcinosis appears to be CPPD.
Little has been reported in the literature regarding pedal CPPD involvement. Perhaps this is because microscopic examination for crystals is not performed routinely for the workup of acutely symptomatic joints. However, the literature refers to metatarsophalangeal, tarsal (talonavicular, in particular), and ankle joint involvement.22 Chondrocalcinosis is not readily recognized at the tarsal joints, because other bones are superimposed.
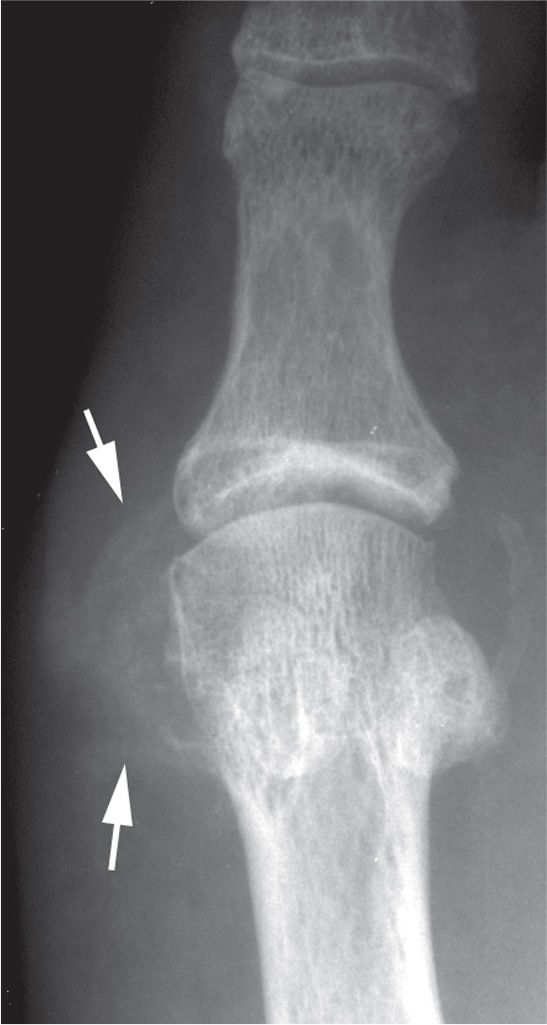
FIGURE 19-22. Gout: calcified tophus. Faint calcifications are seen in the soft tissues medial to first metatarsal head (arrows).
Calcification of periarticular structures, including tendons and bursae, is also seen with hydroxyapatite crystal deposition disease (HADD).23 The clinical course may mimic the single-joint symptomatology seen with gout and pseudogout.24 The radiographic presentation of HADD, also referred to as calcifying tendonitis, consists of round or oval calcifications within the course of a tendon.25 Linear or punctate calcific densities may be seen along the margins of affected joints. Another presentation can be a rather large, amorphous calcification adjacent to a joint.
Detritus
Ossicles may be seen in the joint and are referred to as loose osseous bodies. Also referred to as “joint mice,” loose bodies vary considerably in size and architecture. They are occasionally seen in osteoarthritic joints (Figure 19-23). Trauma can cause osteophytes or subchondral bone with overlying cartilage to break off. These fragments of bone and/or cartilage can float or become wedged within the joint or synovium. Because many of these loose bodies contain cartilage, faint calcifications may be identified. They tend to enlarge over time. Large osseous bodies or fragments in the midfoot and tarsal joints are suggestive of either posttraumatic arthritis or Charcot neuropathic osteoarthropathy (Figure 19-24).
Geode
Geode, also referred to as subchondral bone cyst or pseudocyst, is a subarticular area of rarefaction, usually presenting as a geographic lytic lesion. It may be seen in osteoarthritis, rheumatoid arthritis, osteonecrosis, and CPPD disease.26 The geode may mimic erosion viewed en face; this is especially true along the medial aspect of the first metatarsal head. (Because the term cyst implies an epithelial-lined cavitary lesion, the term geode is deemed to be more appropriate.26–28)
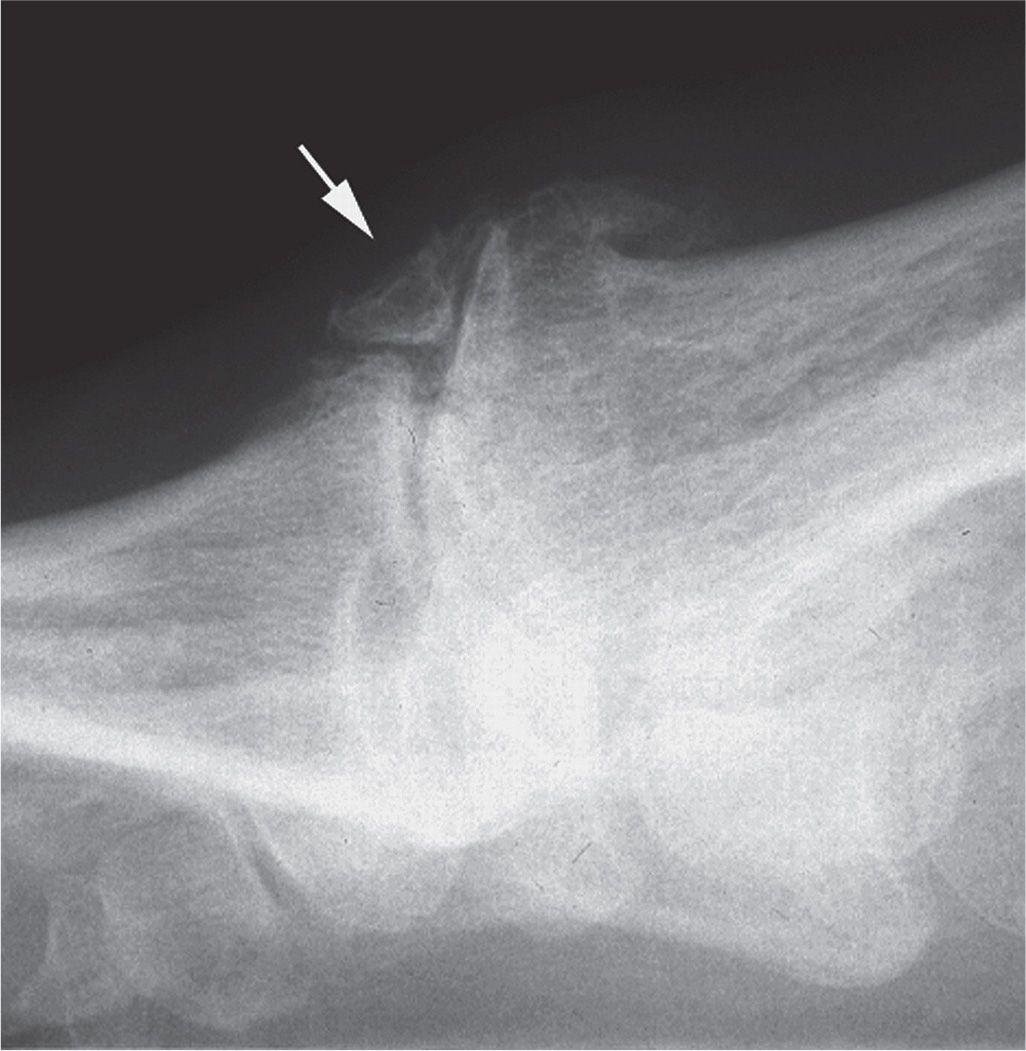
FIGURE 19-23. Loose bodies (arrow), osteoarthritis. An osteophyte is also seen along the superior aspect of the first metatarsal head.
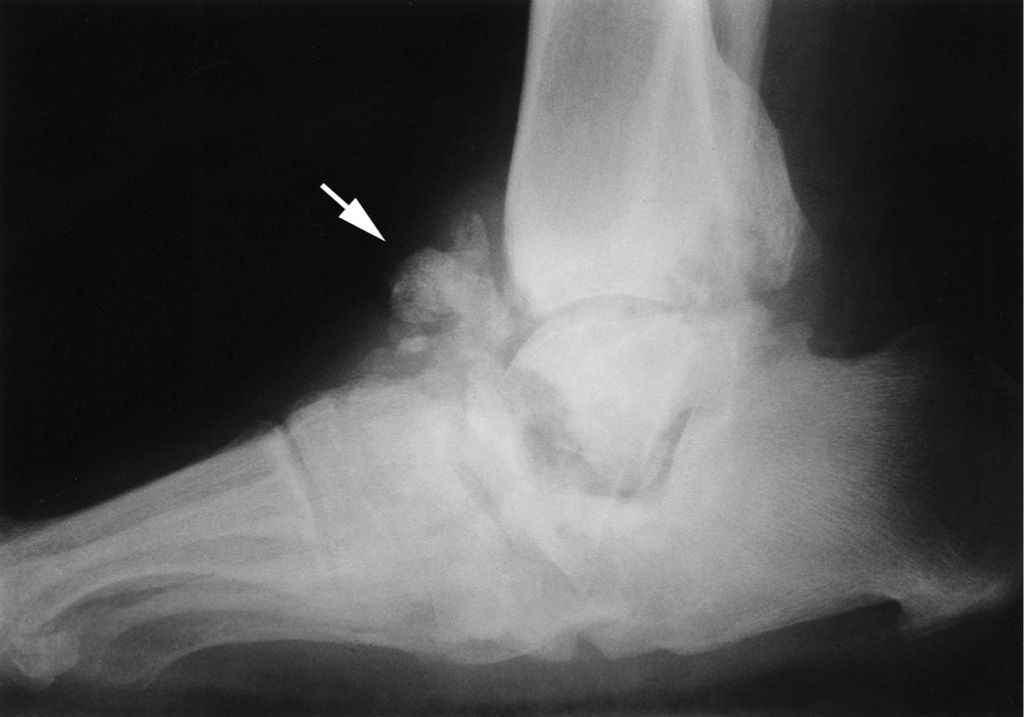
FIGURE 19-24. Detritus arthritis (arrow): tarsal Charcot neuropathic osteoarthropathy. Additional findings include diffuse sclerosis and subchondral resorption (talonavicular region and posterior ankle).
The typical subchondral geode with sclerotic margin is commonly associated with osteoarthritis (Figures 19-4 and 19-16).27 Its pathogenesis is controversial; the two probable mechanisms are bone contusion29 and synovial intrusion.26 Geode has also been associated with rheumatoid arthritis (Figure 19-25). Its radiographic appearance is identical to the degenerative geode but lacks a sclerotic margin.30 The mechanism of formation is thought to be pannus invading the subchondral bone.31 The mechanism and radiographic appearance of the CPPD geode is similar to that associated with osteoarthritis, except the geode may be larger. The osteonecrosis geode forms as a result of osteoclastic resorption of necrotic bone; radiographically there may be surrounding sclerosis.26
MSU crystals, typically deposited in the soft tissues in patients with gout, may also be deposited in bone.32 This deposition has been associated with chronic tophaceous gout. Multiple focal, geographic areas of bone loss (rarefaction) are seen at these sites (see Figure 19-26). Christman (unpublished data) observed, in a retrospective study of 40 patients with gouty arthritis, that localized rarefaction at the first metatarsophalangeal joint with the absence of erosion is frequently an early radiographic finding. The rarefaction is localized in the medial and superior aspects of the first metatarsal head. Although this finding is nonspecific, in the proper clinical setting it suggests gouty arthritis.
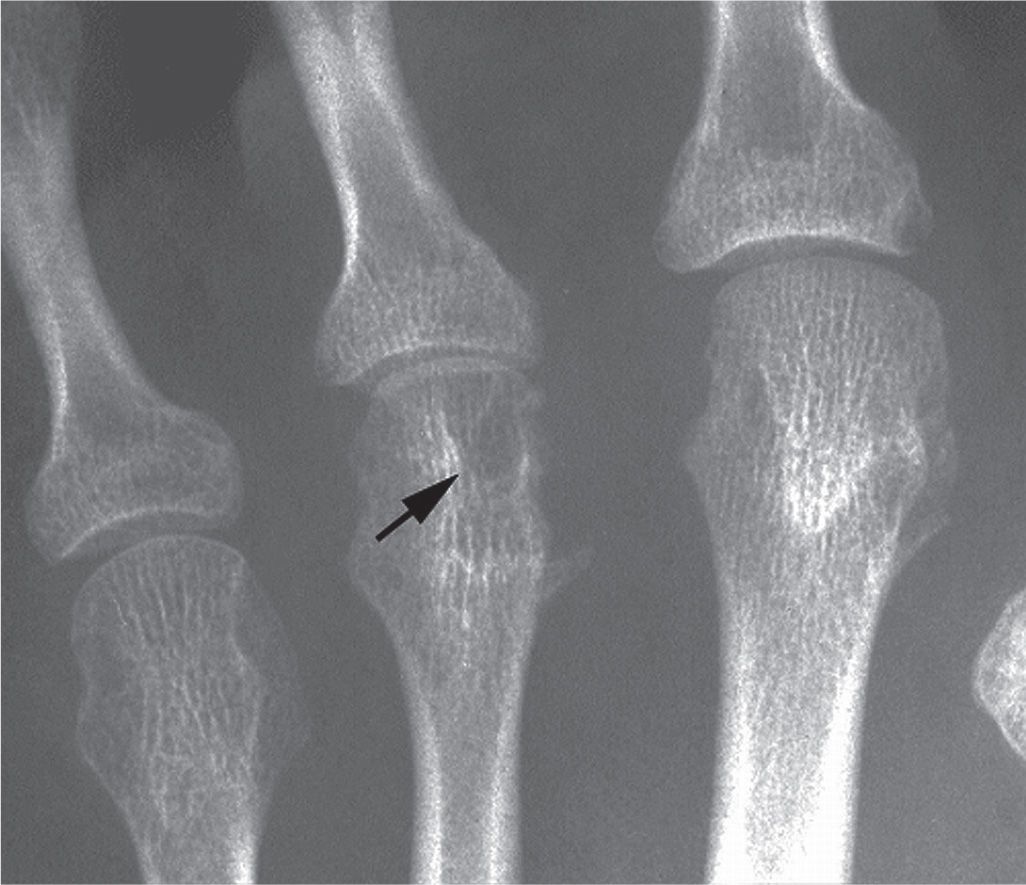
FIGURE 19-25. Rheumatoid arthritis: geode (arrow). Other findings include medial third metatarsal head erosion and joint space narrowing.

FIGURE 19-26. Early gout: rarefaction first metatarsal head and proximal phalanx base, medially. The latter was actually an erosion viewed en face.
Osteopenia
Para-articular osteopenia has been described as an early, though not specific, finding in rheumatoid arthritis. It is considered to be an indirect sign of synovitis, a collateral effect of osteoclast activation.33
Alignment Abnormalities
Positional deformities may be encountered with joint disorders. Abnormalities range from nonspecific misalignment of bones to subluxation and dislocation.
Fibular deviation of the digits, especially the hallux, is associated with rheumatoid arthritis, especially late in the course of the disease (Figure 19-27). This finding generally does not involve the fifth digit, however; the constraints of shoe gear probably prevent lateral deviation of this toe. Erosion may or may not accompany misalignment. It is important to note that hallux abductovalgus and lesser toe deformities are nonspecific; these abnormalities are frequently seen in the absence of rheumatoid arthritis.
Subluxation and dislocation are frequently encountered in the rheumatoid forefoot. These changes especially affect the lesser metatarsophalangeal joints. The digits dislocate superiorly; superimposition of the proximal phalanx base on the metatarsal head may appear as ankylosis in the dorsoplantar view (Figure 19-28). Metatarsophalangeal joint dislocation is best appreciated with the lateral view, although it is difficult to visualize the joint structures because the adjacent bones are superimposed.

FIGURE 19-27. Rheumatoid arthritis: fibular deviation.
Midfoot joint subluxation and dislocation are characteristic features of tarsal Charcot neuropathic osteoarthropathy. This is especially noteworthy at the tarsometatarsal joints, although it can also occur at the intertarsal joints (Figure 19-29). The forefoot dislocates superolaterally relative to the rearfoot. Posterosuperior calcaneal displacement is noted when the talocalcaneal joint is involved.
Misalignment between two articular surfaces can result in cartilage damage and subsequent osteoarthritis. Examples include hallux abductovalgus and other medial column misalignments associated with pes planus and pes cavus.
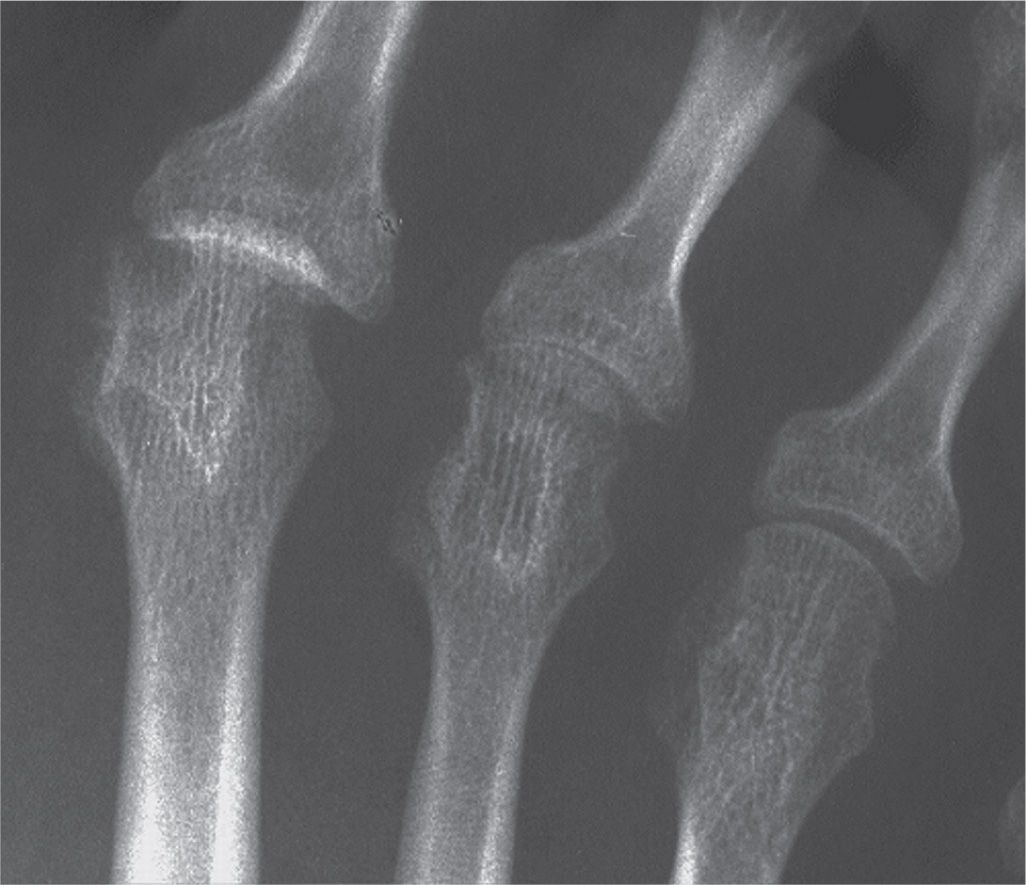
FIGURE 19-28. Rheumatoid arthritis: second metatarsophalangeal joint dislocation simulating ankylosis.

FIGURE 19-29. Neuropathic osteoarthropathy: midfoot subluxation and dislocation.
Pes planovalgus is a frequent deformity in the rheumatoid arthritis midfoot. It is also seen with Charcot neuropathic osteoarthropathy. Alignment abnormalities are not commonly observed with seronegative and gouty arthritis.
Extra-articular Involvement of Joint Disease
Erosion
With rheumatoid and seronegative arthritis, erosions may also be found at sites distant from involved joints. The calcaneus is a common location. The site most frequently affected is the bursal projection (posterosuperior aspect). The retrocalcaneal bursa lies over this portion of bone. The bursa is lined by synovium, and the bursal projection is covered with cartilage.34 The bursitis accompanying rheumatoid arthritis and the seronegative arthritides frequently causes rarefaction and erosion of the adjacent calcaneus (Figure 19-30). The erosion may be bounded by sclerosis in some instances. Retrocalcaneal bursitis caused by local trauma or irritation should not in turn cause underlying bone pathology in the absence of infection or systemic inflammatory rheumatic disease. Erosion along the inferior surface of the medial tuberosity can also be encountered. Rarely, calcaneal erosion is associated with gout.
Psoriatic arthritis can erode the hallux ungual tuberosity (Figure 19-31). This may be an isolated finding. The outline of the tuberosity may appear irregular and sometimes spiculated (Figure 19-13). This finding alone is not pathognomonic for psoriatic arthritis; normal variation appears similar.
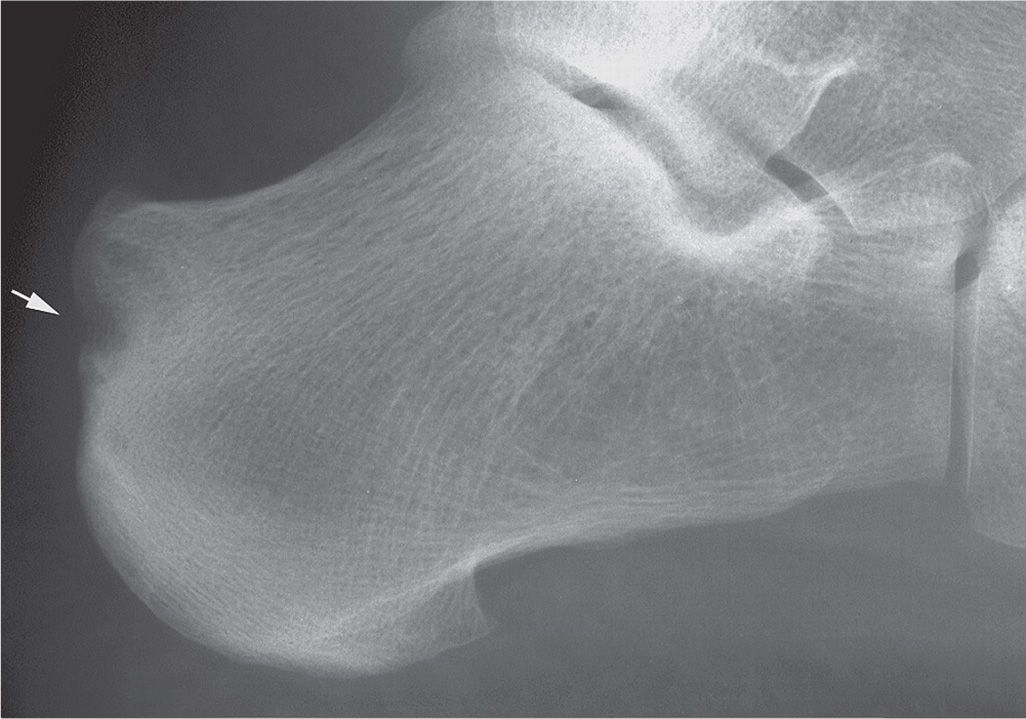
FIGURE 19-30. Rheumatoid arthritis: erosion along calcaneal bursal projection (arrow).
Enthesopathy
Enthesopathy represents an alteration at any ligamentous or tendinous attachment to bone (i.e., enthesis). It may present as spur formation, erosion, or a combination thereof (Figure 19-32A). Enthesopathy has been associated with many joint disorders (Box 19-12).35,36 Common sites of enthesopathy in the foot are the inferior calcaneal tuberosities and the posterior calcaneus. The fifth metatarsal tuberosity is infrequently affected.
BOX 19-12 Differential Diagnosis of Enthesopathy in the Foot
Trauma
Degenerative disease (well-defined, pointed or hook shaped, inferior calcaneal spur)
Osteoarthritis
Diffuse idiopathic skeletal hyperostosis
Inflammatory joint disease
Rheumatoid arthritis (well-defined, inferior calcaneal spur)
Seronegative spondyloarthritis (irregular, large calcaneal spur)
Crystal deposition disease
CPPD (probable)
HADD (probable)
Gout (possible) (ill-defined, small, inferior calcaneal spurs)
Endocrine disorders
Diabetes mellitus
Inferior calcaneal spur formation associated with degenerative joint disease and rheumatoid arthritis is generally well-defined. Degenerative spurs commonly are pointed and sometimes hook shaped. However, early spur development, regardless of etiology, may be ill-defined. Calcaneal spur formation related to seronegative arthritis tends to be large and irregular. Ill-defined erosion and adjacent sclerosis frequently accompany these spurs (Figure 19-32B). Inferior calcaneal spurs may be seen with gout. They are smaller and ill-defined.

FIGURE 19-31. Psoriatic arthritis: ungual tuberosity erosion (acro-osteolysis).
Soft Tissue Mass
Gouty tophi may be found anywhere in the foot, not just intra- or periarticular. Rheumatoid nodules are rarely encountered in radiographs of the foot but could appear similarly at extra-articular sites.
Patterns of Joint Disease and Distribution of Roentgen Findings
Joints Involved
Each of the joint disorders (with the exception of septic arthritis) consistently targets specific sites in the foot. Furthermore, joints may be involved that are clinically asymptomatic. Radiographs of both feet (dorsoplantar and lateral views, at a minimum) are needed to assess the pattern of joint disease and distribution of roentgen findings. Box 19-13 lists the primary joints targeted by the more common pedal disorders. The patterns of joint involvement and distribution of roentgen findings are discussed in more detail with the following characteristic descriptions of each joint disorder.
BOX 19-13 Primary Target Joints
Osteoarthritis | First MPJ |
Rheumatoid arthritis | MPJs |
Seronegative spondyloarthritis | Lesser MPJs, DIPJs |
Gout | First MPJ |
Neuropathic osteoarthropathy | Tarsometatarsal and intertarsal joints |
DIPJ, distal interphalangeal joint; MPJ, metatarsophalangeal joint.
Extra-articular Sites Involved
Calcaneal abnormality is frequently associated with joint disease. Both spur and erosion may be encountered at inferior and retrocalcaneal locations. For this reason, lateral views should always be included with dorsoplantar views of the feet when evaluating for joint disease. It is unusual to see erosions of the calcaneus unless they are associated with inflammatory rheumatic disease or infection. Occasionally erosion may be encountered with gouty arthritis at an enthesis, adjacent to a tophus.
CHARACTERISTIC PRESENTATIONS OF JOINT DISEASE IN THE FOOT (TABLE 19-6)
Osteoarthritis
Osteoarthritis is the most frequently encountered pedal joint disorder. It is not just a disease of the elderly population; in the foot and ankle, regardless of age and weight, it occurs secondary to abnormal wear and tear to a particular joint (pronatory biomechanical abnormality is most frequent37) or is posttraumatic (related to either repetitive low-impact injury, or to a single event, such as a high-impact sports injury38).
The term osteoarthritis is misleading, because the disease is not primarily inflammatory in nature. It has also been referred to as degenerative joint disease (DJD), degenerative arthritis, and osteoarthrosis. The term degenerative joint disease is more general and pertains to synovial and nonsynovial locations.39 Osteoarthritis specifies joint disease at a synovial articulation. The disorder is one of chronic cartilage and subchondral bone deterioration; if inflammation is present, it is mild in severity and not a primary pathologic feature. Because the term osteoarthritis is widely accepted, it will be used in this discussion.
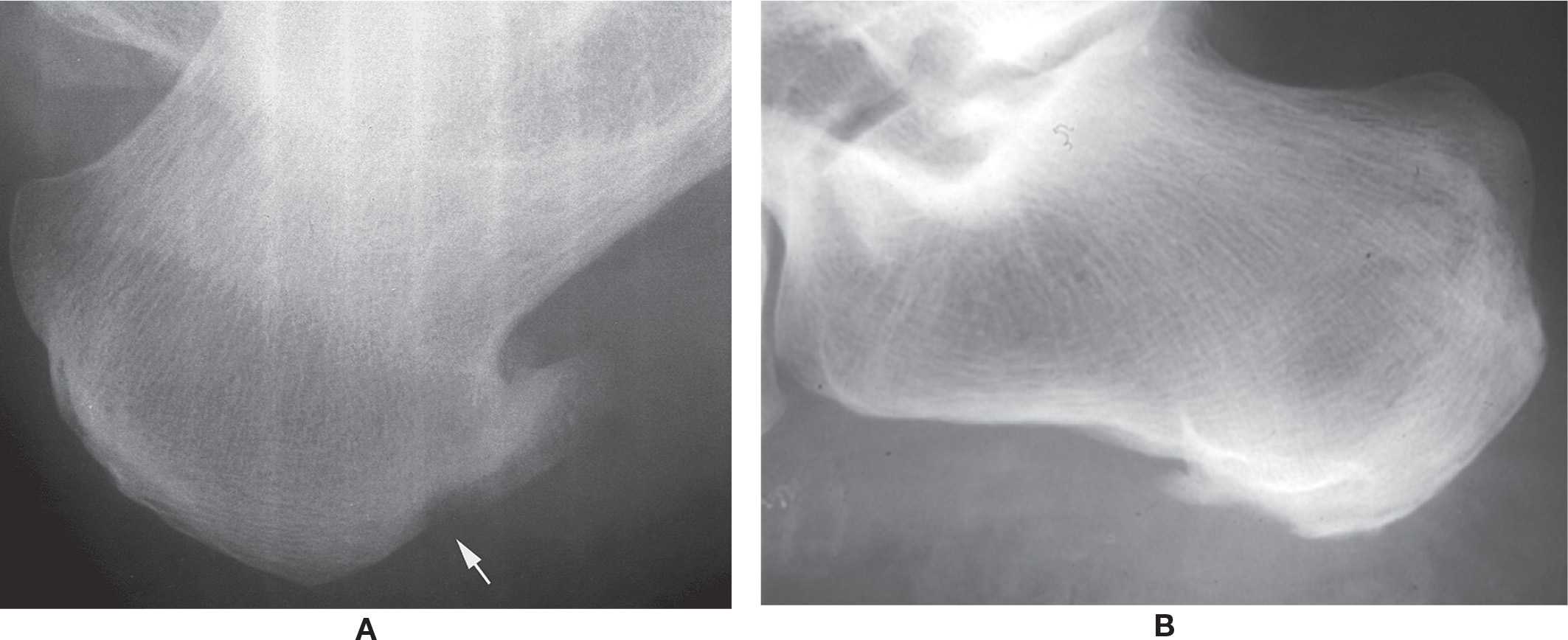
FIGURE 19-32. Enthesopathy. A: Rheumatoid arthritis: spur and erosion (arrow). B: Psoriatic arthritis: ill-defined inferior calcaneus erosion and spur surrounded by diffuse sclerosis.
| Presentation of Joint Disorders in the Foot |
Another misnomer is use of the term “destructive” to denote a late-stage osteoarthritic joint. Degenerative implies a slow or chronic “wear and tear” process, whereas destructive reflects an aggressive, acute, and lytic process. Because the latter term may have different connotations, its use should be avoided in this context.
Osteoarthritis targets joints along the medial column of the foot (Box 19-14). Its distribution is typically asymmetric, but it is not uncommon to see the same joint or joints affected bilaterally; also, if bilateral, the findings may not be symmetric in severity. It is unusual to see osteoarthritis at the remaining pedal joints unless related to previous trauma.
Osteoarthritis develops from one or both of the following settings40,41: (1) abnormal concentration of force/mechanical stress on a normal articulation, which includes its supporting connective tissues (for example, direct trauma, accumulation of repetitive microtrauma, misalignment); and (2) normal concentration of force on an abnormal articulation (an underlying cartilage or subchondral bone abnormality, such as osteonecrosis).
BOX 19-14 Target Joints: Osteoarthritis
Hallux interphalangeal
First metatarsophalangeal
Second metatarsocuneiform
Intermediate naviculocuneiform
Talonavicular
Radiographic evidence of osteoarthritis typically takes years to develop. The characteristic features (summarized in Box 19-15 and illustrated in Figure 19-33) include (collectively or individually):
BOX 19-15 Osteoarthritis: Radiographic Features
Primary finding: osteophyte
Uneven joint space narrowing
Subchondral sclerosis (eburnation)
Geode with sclerotic margin (subchondral cyst)
Detritus (loose body, “joint mouse”) usually posttraumatic
Gross joint deformity seen in severe osteoarthritis
Targets: medial column, especially first metatarsophalangeal joint; other joints if posttraumatic
Foot distribution: U/L, B/L, any joint possible; monoarticular or polyarticular. If bilateral, typically asymmetric in location and severity. Seldom involves the lesser toe IPJs, unlike the hand. Ankle joint involvement primarily with history of fracture
Elsewhere: hands, knees, spine

FIGURE 19-33. Osteoarthritis. A: First metatarsophalangeal joint. B: Secondary to Freiberg disease or previous trauma, third metatarsophalangeal joint. C: Second metatarsal-intermediate cuneiform joint.
1. Osteophytosis. An osteophyte is a bony outgrowth (spur) at the margin of the affected joint (Figures 19-1, 19-10, 19-16, and 19-23). It frequently is an isolated finding but can present in combination with any or all of the following four findings, especially in more severe cases. Evidence suggests that osteophyte formation does not predict disease progression.42 Normal bone density is maintained and trabecular reorganization occurs in the osteophyte. Osteophytes have also been found in the absence of cartilage loss. As such, osteophyte formation may be a reparative process, or possibly a redistribution response to changes in weightbearing, stress distribution, or microfractures. Though experimentally induced osteoarthritis in the rabbit knee has demonstrated the identification of osteophytes in as little as 2 weeks,43,44 it is a chronic, gradual process under normal circumstances.
2. Joint space narrowing. The joint space narrowing typically is uneven (or nonuniform). Narrowing occurs at the focus of the applied abnormal force or at the site of cartilage or subchondral bone abnormality (Figure 19-16); however, uniform narrowing may be seen if the entire cartilaginous surface is affected (Figure 19-10).
3. Subchondral sclerosis (also called eburnation). This finding is represented by periarticular increased bone density. Subchondral sclerosis is frequently found adjacent to the site of joint space narrowing. In more severe cases, its appearance is diffuse (Figure 19-10). Sharma et al.45 demonstrated that osteophytosis and sclerosis are inversely related phenomena. There also does not appear to be any correlation between subchondral sclerosis and cartilage degeneration, at least not in the first metatarsal head,46 which may suggest that sclerosis is the process of supporting the cartilage so it does not collapse.42 However, subchondral sclerosis does increase as the disease progresses.1
4. Geode (subchondral cyst) formation. The geode or subchondral (aka “degenerative”) cyst is a geographic, radiolucent, eccentric lesion frequently associated with the osteoarthritic joint. It characteristically has a thin, sclerotic margin (Figures 19-4 and 19-16). The location of this lesion at the margin of a bone may be mistaken for erosion; however, erosion is not a characteristic feature of osteoarthritis and its presence suggests an underlying inflammatory condition.
5. Loose osseous body (or “joint mouse”). The loose body appears as a bone fragment or ossicle within the joint or along its margins (Figure 19-23). It more than likely is related to a traumatic event, which the patient may not ever recall; it could be an osteochondral bone fragment that initiates osteoarthritis (a subchondral defect may be identified) or can represent a fractured osteophyte in an already existing osteoarthritic joint.
MRI (Magnetic Resonance Imaging) of Cartilage
There is poor to moderate correlation between the radiographic characteristics suggesting degenerative cartilage and the actual degree of cartilage damage. Also, no correlation has been found between subchondral plate thickness, porosity of bone, or osteophytosis and the degree of cartilage degeneration.38,46–49 Recently developed MRI techniques and sequences allow for a sensitive analysis of cartilage from focal lesions to generalized disease.38 The SPGR (spoiled gradient-recalled echo) sequence produces a high cartilage signal, while the signal for the adjacent joint fluid is low, thus making the SPGR sequence the current standard for quantitative morphologic imaging of cartilage.50 Having a long-term precision error of only 1.4 to 3.9%, SPGR sequence may be used for diagnosis, patient follow-up, and longitudinal studies.38,51 Newer MRI techniques, such as dGEMRIC, T1ρ MRI, and NaMRI (sodium MRI), provide a validated quantitative measurement of specific articular matrix constituents, making them useful in the future for early articular cartilage damage evaluation and follow-up.38
Interphalangeal Joints
Osteoarthritis seldom affects the interphalangeal joints of the lesser toes, unlike the hands. Joint space narrowing and osteophyte formation are the usual findings; however, joint space narrowing is difficult to ascertain in most cases, because of digital contracture. Furthermore, the tubercles along the margins of the phalangeal bases may appear as osteophytes if the toe is rotated into adductovarus.
Hallucal interphalangeal osteoarthritis is frequently posttraumatic in nature and affects the medial aspect of this joint; radiographic findings generally are limited to irregular joint space narrowing. Loose osseous bodies and small geodes are occasionally associated with osteoarthritis at this site.
First Metatarsophalangeal Joint
The first metatarsophalangeal joint is by far the most commonly affected pedal joint and may demonstrate few or all of the classic radiographic features of osteoarthritis (Figure 19-33A; also, Figures 19-1A, 19-10, 19-16, and 19-23).
Mild osteoarthritis typically features an osteophyte, small or large, but with only minimal uneven joint space narrowing. Osteophytes are more likely to be seen at the proximal side of the joint, but may also present along the adjacent proximal phalangeal base. A larger superior osteophyte may be associated with medial enlargement of the metatarsal head. Joint space narrowing is best appreciated in the dorsoplantar view. Loose osseous bodies are more commonly associated with severe osteoarthritis but also can be seen in mild disease. They typically present superiorly and are therefore best visualized in the lateral view. Osteochondral defect is infrequently seen centrally in the first metatarsal head.
Mild to moderate osteoarthritis demonstrates progressive joint space narrowing and osteophytosis in varying degrees. Loose osseous bodies are also more frequent. Mild subchondral sclerosis may become evident. (A well-defined, increased density is normally present along the concave hallux proximal phalanx base centrally and may be mistaken for eburnation. The eburnation associated with osteoarthritis is typically ill-defined and diffuse in appearance.) Osteochondral defects and/or geodes are infrequent but may appear exaggerated relative to the other radiographic findings.
Significant joint space narrowing, osteophytosis, and eburnation are seen with moderate to severe osteoarthritis. Geode formation, at either side of the joint or within the hypertrophied medial eminence, is also frequent.
Gross joint deformity is seen in severe osteoarthritis. The first metatarsal head and proximal phalanx base are hypertrophied both medially and laterally. Subchondral sclerosis is exaggerated, and subchondral geodes and loose osseous bodies are predominant.
Metatarsosesamoid osteoarthritis is not uncommon and is best visualized in the sesamoid axial view. Irregular joint space narrowing and small osteophytes may be seen. Similar findings may be seen in the lateral view but are unlikely, because numerous osseous structures are superimposed.
Lesser Metatarsophalangeal Joint
Lesser metatarsophalangeal joint osteoarthritis is generally not seen unless the patient has had epiphyseal osteonecrosis (Freiberg disease) or a history of injury to the joint. Gross deformity of the metatarsal head and proximal phalangeal base are predominant findings (Figure 19-33B).
Metatarsocuneiform Joints
Osteophytosis, subchondral sclerosis, and joint space narrowing can be visualized in both the dorsoplantar and lateral views. Osteoarthritis of the first metatarsocuneiform joint is frequently associated with osteoarthritis of the second metatarsocuneiform joint; however, the converse is not.
Osteoarthritis of the second metatarsocuneiform joint is best identified in the lateral view (Figure 19-33C). The primary finding is dorsal osteophytosis; lack of visualization of a joint space and subchondral sclerosis may also be apparent. Joint disease is not easily visualized in the dorsoplantar or medial oblique views unless the arthritis is severe.
Osteoarthritis of the third metatarsocuneiform joint is not frequently encountered. When present, joint space irregularity and eburnation are best noted in the medial oblique and lateral views.
Naviculocuneiform Joints
Osteoarthritis of the medial naviculocuneiform joint primarily consists of joint space irregularity and subchondral sclerosis, with or without mild osteophytosis. These findings are best seen in the dorsoplantar view, although joint space narrowing can also be seen along the inferior aspect of this joint in the lateral view.
Intermediate naviculocuneiform osteoarthritis is best visualized in the lateral view and is characterized by dorsal osteophytosis, joint margin irregularity, and eburnation (Figure 19-1B). Similar findings may be seen in the medial oblique view; the dorsoplantar view seldom is useful for assessment at this location. Intermediate naviculocuneiform osteoarthritis is frequently associated with osteoarthritis of the second metatarsocuneiform and medial naviculocuneiform joint.
Talonavicular Joint
Talonavicular joint osteoarthritis is best appreciated in the lateral view. Radiographic findings vary from large osteophyte formation superiorly with normal joint space to significant joint narrowing with subchondral sclerosis. Occasionally an osteochondral defect will be seen along the navicular posterior articular surface associated with osteoarthritis at the talonavicular joint.
Calcaneocuboid Joint
Osteoarthritis is seldom seen at the calcaneocuboid joint. The typical finding, when present, includes an enlarged, hook like exostosis laterally, originating from the calcaneus and seen primarily in the dorsoplantar view; the joint space is relatively spared, and the lateral view appears normal. When more pronounced, eburnation and joint space narrowing can also be seen in both the dorsoplantar, medial oblique, and lateral views.
Talocalcaneal Joint
The middle and posterior talocalcaneal joints are not easily visualized with radiography, and osteoarthritis is not common. However, posterior talocalcaneal osteoarthritis may be recognized in the medial oblique and lateral ankle views as joint space narrowing and osteophyte production, and less frequently with calcaneal axial views at varying degrees of tube head angulation. Incomplete or fibrocartilaginous coalition is often associated with evidence of middle talocalcaneal joint osteoarthritis in the lateral view, which presents as joint space narrowing and eburnation. Computed tomography (CT) is valuable for further assessment of this joint.
Ankle Joint
Unlike the knee and hip, primary osteoarthritis of the ankle is rare.52 It has a very high association with a previous history of fracture or significant ankle trauma (78%53 and 70%52). Of the world’s adult population, approximately 15% is affected by osteoarthritis54; approximately 1% of that 15% have ankle involvement.55 Fracture of the malleoli is the most severe risk factor for development of ankle osteoarthritis, accounting for about 39% of the ankle osteoarthritis cases.53 In contrast, the painful ankle in a geriatric patient with no prior history of trauma seldom demonstrates radiographic evidence of osteoarthritis, or mild at best. Posttraumatic ankle arthritis demonstrates varied radiographic features, depending on the type of injury and its extent. Findings may include osteophytosis (best seen in the lateral view), uneven joint space narrowing, subchondral sclerosis, and subchondral lucency (related either to the fracture site itself, an osteochondral defect, or geode formation).
Rheumatoid Arthritis
Rheumatoid arthritis targets synovial tissue, especially of the foot and hand. The acute synovitis and associated pannus formation result in lysis of intra-articular structures, including cartilage and subchondral bone. Capsular and ligamentous laxity also occurs. Clinically, the onset is insidious and its course demonstrates periods of remission and exacerbation. The majority of these patients are seropositive for rheumatoid factor. Its etiology, however, is unknown but is regarded as an autoimmune disorder33.
A new classification system has redefined the 1987 American College of Rheumatology system to one that features earlier stages of the disease.56 It has been widely tested in many patient populations and appears to be a sensitive instrument.57 In general, there are four classification criteria: joint involvement, serology, acute-phase reactants, and duration of symptoms.
The radiographic appearance of early rheumatoid arthritis of the foot differs from its well-established form. The latter classically involves all metatarsophalangeal joints bilaterally and occasionally the hallux interphalangeal joints. In contrast, early rheumatoid arthritis is often monoarticular or polyarticular but asymmetric. The fifth metatarsophalangeal joint is frequently the first joint affected. Findings at the first metatarsophalangeal joint are generally subtle or unremarkable. Although rheumatoid arthritis may involve the tarsal (especially the talocalcaneal) joints, early recognition is difficult with radiography. CT may be necessary for further evaluation of these joints. Unlike the hand, it is rare to see involvement of lesser toe interphalangeal joints.
The radiographic grading system proposed by Larsen et al.58 is still widely used for grading rheumatoid arthritis (Table 19-7). Scott et al.59 later modified the Larsen system to provide more sensitivity for grading early and mild radiographic changes. These two sets of descriptors were then combined by Edmonds (Table 19-8).60 Although radiography still plays a great role for imaging rheumatoid arthritis, it is not sensitive enough to detect the earliest signs (hyperemia, synovitis, effusion, and para-articular osteopenia) prior to erosion, which are valuable for early diagnosis and treatment to delay joint destruction.
| Larsen System for Radiographic Grading of Rheumatoid Arthritisa,58 |
Grade | Definition | Radiographic Findings |
0 | No radiographic changes | Abnormalities not related to rheumatoid arthritis may be present |
1 | Slight abnormality | Periarticular swelling, para-articular osteopenia, slight joint space narrowing |
2 | Definite early abnormality | Erosion (except in weight-bearing joints), joint space narrowing |
3 | Medium destructive abnormality | Erosion (in all types of joints), joint space narrowing |
4 | Severe destructive abnormality | Erosion, joint space narrowing, bone deformation in weight-bearing joints |
5 | Mutilating abnormality | Disappearance of the original articular surfaces, gross bone deformities in weight-bearing joints |
aImages (“standards”) were included in the original publication for more specific correlation to the different grades.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








