View Selection for the Radiographic Study
Careful thought and consideration are necessary to select the positioning techniques that optimally demonstrate the area in question. One must be able to predict, before the study is ordered, how each bone will appear in every view. This is not easy. In addition to the differing appearances of the foot in each view, the appearance of the bones in a pronated foot, for example, is quite different from those in a supinated foot. Competency, therefore, requires continual and repetitive review of radiographs, paying special attention to the form, position, density, and architecture of each bone.
Selecting positioning techniques for a foot or ankle study should not be performed as a routine. However, it has become common practice to perform a standard set of positioning techniques for these studies; emphasis is not placed on the specific clinical area of symptomatology but on the views that show the most bones with the least amount of superimposition. They include the dorsoplantar, lateral, and medial oblique foot views and the anteroposterior, mortise, and lateral ankle views. Alternative views that may be more appropriate are not initially considered in this scenario. Because of this approach, some pathologic conditions may not be recognized.
It is not uncommon for certain practices or procedures to continue for decades without being questioned. This, unfortunately, does not make such procedures correct. One example is the routine bilateral radiographic foot or ankle study. Another is the number of positioning techniques performed. A third example concerns the technical aspects of a weight-bearing foot study. These are discussed in turn. Overutilization of radiographic studies is also briefly examined.
The last half of this chapter concentrates on which views best demonstrate each bone and specific osseous landmarks. A method is presented that simplifies the process by which views are selected.
BILATERAL VERSUS UNILATERAL STUDY
No written rule states that an extremity study should routinely be performed bilaterally. Some practitioners, however, habitually obtain views of both extremities for every radiographic study performed. The reasoning behind this practice has been to provide a comparison view of the opposite extremity, a baseline for future reference, or a means for biomechanical (orthomensurative) examination.
Use of comparison views should decrease as the practitioner’s level of experience increases. The more familiar one becomes with normal radiographic anatomy, the less necessary are comparison views. Use of a reference standard, such as that provided in the radiographic anatomy section of this text, may, in many instances, be sufficient to replace the need for a comparison view of the opposite extremity. Furthermore, short tubular bones, such as the metatarsal and phalanx, rarely require comparison views of the opposite extremity; the remaining tubular bones of the same extremity serve as useful standards for comparison. To become familiar with the multiple superimposed shadows in the midfoot, rearfoot, and ankle regions, one must study these areas carefully and correlate them to the gross anatomic specimen routinely, not just when searching for a specific pathology.
Bilateral studies have also been advocated for the pediatric radiographic study, especially for epiphyseal injuries.1 However, irregular ossification, multiple ossification centers, and accessory ossification centers are frequently encountered as variations of normal development; their differentiation from abnormality may be impossible, even with comparison views of the opposite extremity. Comparison views of the pediatric foot or ankle may actually be misleading more often than they are beneficial. For example, developmental variants are frequently unilateral. The absence of a variant in the opposite extremity encourages the misdiagnosis of fracture or other pathology.2 Studies have shown that pediatric radiologists do not consider bilateral studies routinely necessary.3,4
The need for bilateral studies is obvious for patients who exhibit symptomatology in both extremities. They are also valuable for assessing joint disease. However, it is illogical to order and perform bilateral radiographic studies routinely for every patient. Direct trauma, for example, does not require radiographic examination of the opposite extremity if the fracture is obvious.
Comparison views of the opposite, asymptomatic extremity may be useful when a questionable lesion or finding is present in the affected extremity. In most instances, the questionable finding only appears in one view. A comparison study of the opposite extremity can, therefore, be limited to the view in question. Other supplementary comparison views offer no additional diagnostic information and expose the patient to additional potentially harmful radiation. If you were the patient, would you appreciate the physician ordering radiographic studies that were not going to contribute to the diagnosis or treatment of your condition?
BOX 10-1 Potential Indications for Radiographic Study of the Foot or Ankle (MINTCAP)
Metabolic, endocrine, nutritional disorders
Infection
Neoplasm
Trauma
Congenital/developmental
Arthritis
Positional deformity
A radiographic study should not be ordered or performed until after an adequate history and physical examination has been completed on the patient and then only if clinically indicated. Baseline radiographic studies without clinical indication should, therefore, not be performed and are discouraged. Nor should radiography for biomechanical examination be performed routinely. The foot should first be analyzed clinically; radiographs should only be obtained if the examination suggests that an osseous structural or positional abnormality exists and could be contributing to the presenting concern and if the outcome of the study could affect the treatment rendered. Potential indications for radiographic study of the foot or ankle are listed in Box 10-1.
NUMBER OF VIEWS
How many views are necessary for evaluating the foot or ankle? This depends entirely on the provisional diagnosis (or diagnoses) and the area of concern. For example, when evaluating the first metatarsophalangeal joint for degenerative joint disease, only dorsoplantar and lateral views are necessary to make the diagnosis. An oblique view ordinarily does not offer any additional information in the diagnosis of osteoarthritis unless the physician is looking for a more specific condition or lesion, such as a loose osseous body.
Controversy exists regarding the number of views necessary to assess ankle trauma. The practice of obtaining three views is advocated widely in the literature.5–7 These views include the anteroposterior, lateral, and oblique (typically the mortise). However, others suggest that the number of ankle views be limited to two (anteroposterior and lateral) or even eliminated in the absence of soft tissue swelling.8–11
A rational, analytic approach for selecting a radiographic study is to first obtain two or three views that best demonstrate the area in question. Typically this would include dorsoplantar and lateral views; an oblique or axial view may be indicated if the area of concern is best seen in one. If your diagnosis is confirmed, no other views are necessary. If a unilateral study is inconclusive or a questionable lesion is seen, additional views should then be obtained of the same extremity. If comparison views of the opposite extremity are warranted, select only those views that were questionable from the initial study. Of course, conditions that can demonstrate generalized radiographic findings, such as inflammatory joint disease, require examination of other regions and/or extremities. Because the distribution of radiographic findings and patterns of joint involvement are important aspects for the evaluation of joint disease, bilateral dorsoplantar and lateral views are advocated.
OVERUTILIZATION/APPROPRIATENESS
Overutilization of radiography has been defined as “excessive irradiation per unit of diagnostic information, therapeutic impact, or health income”; it can include excessive radiation per image, excessive images per examination, or excessive examinations per patient.12 Regarding foot radiography, excessive radiation per image can be minimized by limiting the size of the x-ray beam to the area in question (also known as collimation), using appropriate image receptors, and shielding the patient with a lead apron; excessive images per examination can be limited by initially obtaining only the basic views to assess the area in question and by preventing repeat examinations due to poor positioning and exposure technique; and excessive examinations per patient can be reduced by depending more on clinical findings than relying on radiographs for follow-up examination, by educating the demanding patient that a radiographic study may not be indicated, and by imagining that the cost of the study is being funded by the patient, not reimbursed by insurance. Examples have already been briefly addressed citing areas of potential overuse of radiographic studies, including bilateral comparison studies, the number of views selected for any particular study, and whether the study should be performed at all.
Several factors affect one’s decision to obtain radiographic studies (Box 10-2).13,14 A primary factor is the training and experience of the practitioner. Someone trained to order bilateral comparison views for every patient would certainly perpetuate this activity in practice. Experience, addressed earlier, should also have an effect: The number of studies and/or views ordered should decrease as practical experience increases. Another factor addresses the patient evaluation: Radiographs should never replace a thorough history and physical examination. Studies have suggested that ankle fractures can be discriminated from nonfractures by considering specific clinical variables.15,16 These criteria (Box 10-3), referred to as the Ottawa Ankle Rules (OAR), were designed to minimize false-negative results. The OAR boasts nearly 100% sensitivity and has since been reproduced and validated in different types of medical settings; it has reduced the cost of treating ankle injuries by reducing the necessity of radiographic studies.17–20 In essence, the need for radiographs of the ankle in adults with acute ankle injury is reduced at least 30%. A modification to the OAR (the “Buffalo rules”) (Box 10-3) has shown reduction of greater than 50% while maintaining the high sensitivity.21 Boutis et al.22,23 have validated what is referred to as the “Low Risk Ankle Rule” to safely reduce radiography in children with acute ankle injuries (Box 10-3). The Low Risk Ankle Rule boasts 100% sensitivity for fractures of the distal fibula and has the potential to reduce radiographic studies by nearly 60%.24,25
BOX 10-2 Factors Affecting Radiographic Decision Making
Physician training and experience
Patient examination
Medicolegal justification
Reassurance
Patient insistence
BOX 10-3 Ankle Trauma Rules
Ottawa Ankle Rules (adults) | Radiography indicated if: • Tenderness over the inferior or posterior aspect of either malleolus, including the distal 6 cm • Inability to bear weight (four steps taken independently, even if limping) at the time of injury and at the time of evaluation |
Modified Ottawa Ankle Rules (adults) (aka “Buffalo Rules”) | Radiography indicated if: • Tenderness over the midportion or crest of the bone from the tip of each malleolus to 6 cm proximal • Inability to bear weight (four steps taken independently, even if limping) at the time of injury and at the time of evaluation |
Low Risk Ankle Rule (children) | Radiography may not be indicated to further exclude high-risk ankle injury if tenderness and swelling isolated to: • Distal fibula and/or • Adjacent lateral ligaments distal to the tibial anterior joint line |
Diagnostic imaging criteria have been developed by the American College of Radiology (ACR), which are evidence-based guidelines for making appropriate imaging decisions and enhancing quality of care.26 More specifically, they have developed musculoskeletal imaging guidelines for acute foot trauma, chronic foot pain, suspected ankle fracture, chronic ankle pain, and suspected foot osteomyelitis in patients with diabetes mellitus.27 Also relevant to the foot practitioner are guidelines for imaging soft tissue masses and primary bone tumors.
Nonclinical factors may significantly affect the practitioner’s decision to perform a radiographic study. Radiographs are routinely ordered by many for patients presenting with a history of trauma, with the intent of providing medicolegal documentation. Long13 poses this dilemma: “If the justification for ordering a radiograph is to protect the physician, one wonders what number of those radiographs are clinically necessary.” Radiographic studies are also ordered for reassurance, especially after orthopedic surgical procedures and fractures. Generally speaking, most follow-up radiographic examinations only require reassessment at 3- to 4-week intervals, unless clinical history or physical evaluation warrants otherwise. Examples of the latter include postreduction, reinjury, and infection. Another nonclinical factor includes the patient’s insistence. The practitioner should be prepared to educate the patient regarding the determination for radiographs or against their inclusion in the diagnostic workup.
The goal to controlling overutilization is learning diagnostic restraint.28 Occasionally we need to rely on our clinical wisdom; a condition does not always have to be “ruled in or out” by performing one more test, in this case, the radiographic study. Will the outcome of the study affect the treatment instituted? We also must remember that there are possible dangers associated with low levels of ionizing radiation, including diagnostic x-ray studies.29,30 Ask yourself if the radiographic study really is necessary.31,32 Finally, determine whether or not another diagnostic technique may be more appropriate to assess the underlying problem.33
TECHNICAL CONSIDERATIONS
Bilateral studies should be performed as individual studies of each extremity. This limits and directs the x-ray beam to the part under study. X-ray beam limitation (collimation) reduces scatter radiation that otherwise may be absorbed by the patient. For example, bilateral dorsoplantar views of the feet should be performed so that individual exposures of each foot are obtained. The useful x-ray beam can then be collimated to the individual foot (a 5- × 12-in area for a 10- × 12-in image receptor). Exposure of both feet together requires collimation to an area that is much larger (10 × 12 in for a 10- × 12-in image receptor). Scatter radiation increases when collimating to a larger area; this low-energy radiation is easily absorbed by the patient, increasing their dose of ionizing radiation, and can impair the quality of the image. Image quality can also be affected by the direction of the central x-ray beam. A central x-ray beam that is directed to the individual foot or area in question reduces geometric blurring and distortion, resulting in an image that is truer in size, shape, and position.
A basic principle in radiography is to have the x-ray central beam directed perpendicular to both the subject and the image receptor. Oblique views of the feet should, therefore, not be performed weight bearing. Significant distortion of the image results when the central x-ray beam is directed at a 45° angulation to the image receptor (Figure 10-1). Oblique foot views should be performed non–weight bearing and with the foot turned 45° in the coronal plane so that the x-ray beam is directed perpendicular to both the foot and the image receptor. This positioning technique minimizes image distortion.
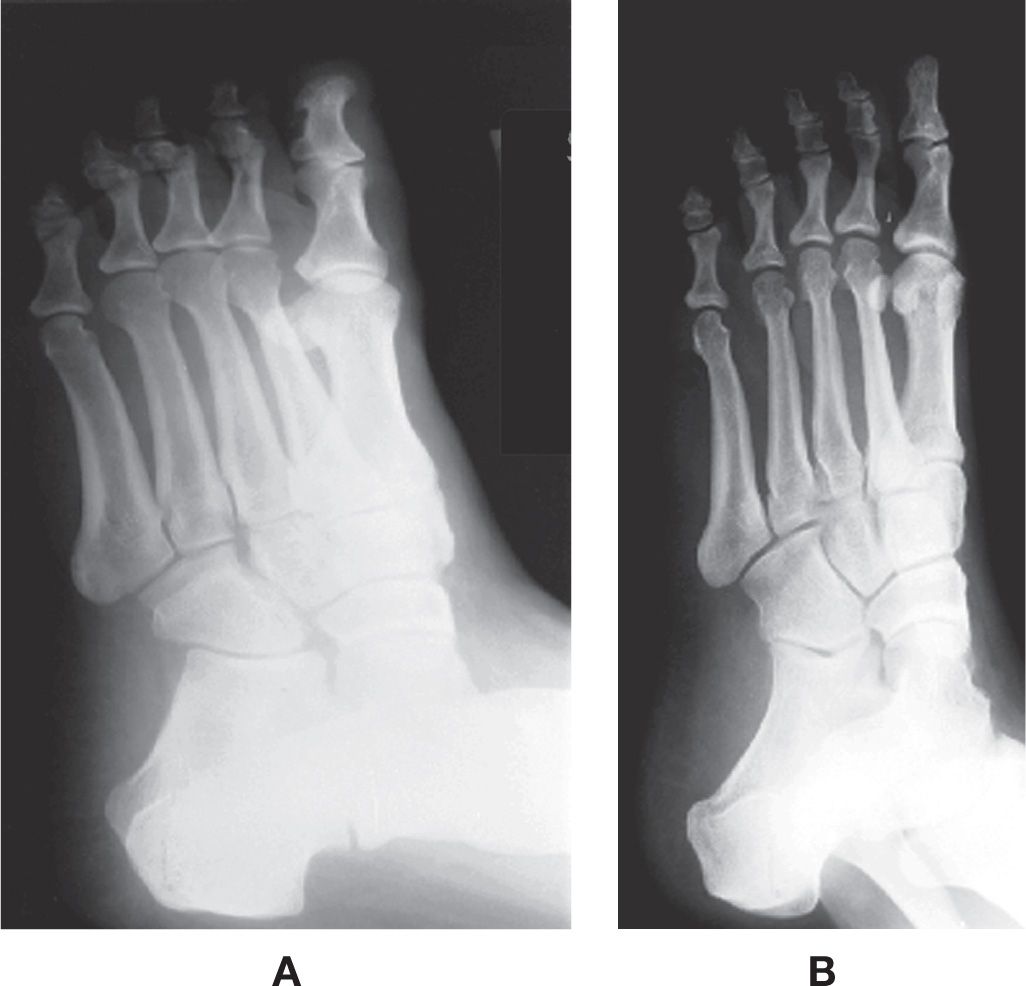
FIGURE 10-1. Weight-bearing versus non–weight-bearing oblique view. A: Distorted weight-bearing oblique view with tube head directed at 45°. B: Non–weight-bearing oblique view with tube head directed perpendicular to image receptor and foot turned 45°.
A compromise in positioning technique is made with the weight-bearing dorsoplantar view. The central x-ray beam, unfortunately, cannot be directed perpendicular to both the foot and the image receptor. Because the tube head physically cannot be positioned perpendicular to the image receptor with the patient standing and because the metatarsals are declined approximately 15° (when averaged together), the tube head is directed at a 15° angle from perpendicular so that it is perpendicular to the osseous structures. Minimal image distortion occurs in this view.
Occasionally a question arises regarding which side of the foot should be positioned closer to the image receptor. Generally speaking, that aspect of the body farthest from the image receptor appears magnified and less sharp. This is especially true in the chest, which has considerable depth. The size of the heart appears larger in an anteroposterior view than that in a posteroanterior view. However, the foot is not very thick (relative to the chest), and size of the foot bones is not a critical aspect in their assessment. The width of the average foot is approximately 3 in. Magnification of that side farthest from the image receptor is only between 1.08 and 1.14, depending on the source-to-image distance (40 and 24 in, respectively). (The magnification factor is determined by dividing the source-to-image receptor distance by the source-to-object distance.34)
SELECTION OF POSITIONING TECHNIQUES
Before studying the following paradigm, it is important to understand the concept of marginal (or tangential) surfaces. A tangent is defined as a line that intersects a curved surface at a single point of intersection35 (Figure 10-2). The outermost aspect or margin of a tubular bone, for example, seen in a two-dimensional radiograph represents the three-dimensional anatomic surface that is tangent to the primary x-ray beam. Unfortunately, bones are irregularly shaped and occasionally have flat surfaces. Furthermore, more than one point or surface may be tangent to the x-ray beam in the same plane. For these reasons, I use the word margin, not tangent, to describe the outermost aspect or outline of a bone seen in the two-dimensional radiograph.
FIGURE 10-2. Illustration of a line tangent to a circle.
BOX 10-4 Marginal Bone Surfaces Seen in Each Foot View
Foot View | Marginal Surfaces |
Dorsoplantar | Medial, lateral, anterior, and posterior |
Lateral | Superior, inferior, anterior, and posterior |
Medial oblique | Superomedial, inferolateral, anterior, and posterior |
Lateral oblique | Superolateral, inferomedial, anterior, and posterior |
Sesamoid axial | Superior, inferior, medial, and lateral |
Calcaneal axial | Medial, lateral, superior, and inferior |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








