Varus Distal Femoral Osteotomy
Patient Presentation and Symptoms
Valgus mechanical alignment of the lower limb transmits excess load to the lateral compartment and is thus thought to influence progression of lateral compartment knee arthritis. This is supported by prospective data where valgus alignment (<5 degrees coronal plane) has been associated with a nearly fivefold increase in the odds of progression of lateral compartment osteoarthritis (OA) (having adjusted for age, sex, and body mass index).1 The rationale underpinning realignment osteotomies about the knee is therefore the prevention or delay of OA in knees with significant malalignment.
As opposed to the varus knee, where this goal has been addressed with proximal tibial osteotomy (PTO), in the valgus knee varus distal femoral osteotomy (VDFO) has had better reported results.2,3 This reflects the fact that the deformity in these cases usually occurs in the distal femur itself and that, in the coronal plane, the joint line often slopes from superolateral to inferomedial.4,5 Correcting the valgus deformity in the proximal tibia does not correct this joint line obliquity and allows the proximal tibia to gradually sublux laterally, leading to increased shear forces across the articular cartilage.6 Several authors have thus recommended that the corrective osteotomy is best performed in the distal femur rather than the proximal tibia. This is particularly true if the tibiofemoral angle exceeds 10 to 12 degrees.7,8
VDFO also alters the biomechanics of the patellofemoral joint, which is an important additional benefit given the high association of valgus malalignment with patellofemoral disorders.6 Valgus deformities may also be better tolerated than varus deformities, due to the forces across the knee in gait, and it is for this reason that they commonly present with arthritis later than varus knees.9
Regarding the specific presentation, the patient should have relatively explicit complaints of lateral joint line pain, as significant involvement of the other compartments indicates that total knee arthroplasty (TKA) may be more appropriate. A history of possible instability or any previous interventions should also be sought. Hip or spine disease may also be very relevant and should be inquired about. The typical deformity of the lower limb is usually readily apparent, and it is important to obtain a history of this deformity from the patient. A history of trauma is of significance, but it should be remembered also that, in contrast to the more common varus deformity of OA, valgus deformities are more commonly associated with other conditions such as rickets, rheumatoid arthritis (RA), renal osteodystrophy, and poliomyelitis.
Indications
Varus distal femoral osteotomy is essentially indicated in the young, active patient with genu valgum with a tibiofemoral angle greater than 15 degrees and symptomatic lateral compartment arthritis that has failed conservative therapy. Deformity should primarily be in the femur, and it is important to recognize a superolateral slope to the joint line as mentioned above. The knee should also be ligamentously stable, as the osteotomy will not address this component of any deformity. There should be a satisfactory range of motion to at least 90 degrees of flexion. Patients with malunited femur fractures can also be considered for a femoral osteotomy. In these cases, the closer the deformity is to the knee, the greater its effect on altering joint biomechanics.
Contraindications
Marked knee instability and flexion contracture of more than 15 degrees are strict contraindications, as is tricom-partmental degenerative disease (though mild medial compartment disease may be acceptable).
Advanced age itself is not a strict cutoff, but an upper age limit of 65 years has been proposed. This is in part due to the longer healing time and resultant restrictions this osteotomy imposes on patients’ mobilization postoperatively. Osteoporosis should also be considered a relative contraindication. Given these considerations and the success of TKA (survivorship approaching 95% at 15 years10) or more recently unicompartmental arthroplasty in the older population, VDFO is not commonly performed in patients over 55 to 60 years of age. With the less certain results of arthroplasty in younger populations, however, VDFO has been reasonably successfully applied to this group.
A relative contraindication is inflammatory arthritis (i.e., rheumatoid and crystalline arthritis). Outcome after osteotomy in these conditions is not as predictable as after osteoarthritis. This is attributed to the synovitis as well as to the involvement of more than one compartment. Unfortunately, it is also these patients who are more likely to present with the valgus arthritic knee.
Physical Examination
Some of the important points in clinical examination have been mentioned already in discussing indications. Essential points include the determination of any significant instability in the joint and whether there is a sufficient range of movement. General examination should include the presence of previous scars and status of the skin and local vasculature. The ipsilateral hip should always be assessed in these patients. An arthritic ipsilateral hip joint can exacerbate lateral knee arthritis by increasing compressive forces across the lateral aspect of the joint and can also be a cause of referred pain.9
Diagnostic Tests
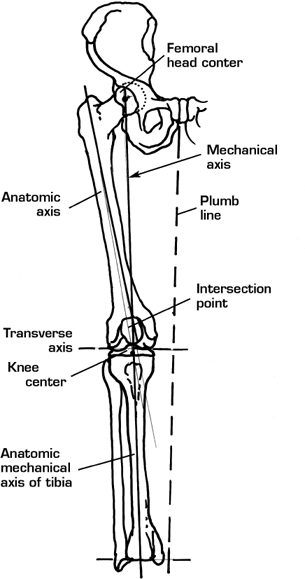
Standing full-length (hip-knee-ankle) roentgenograms of the affected limb with anteroposterior (AP) and lateral views of the knee are obtained. Assessment of the deformity will be based on these radiographs by measuring the axes of the lower extremity. The mechanical axis of the lower extremity is defined as the angle subtended by the lines connecting the center of rotation of the hip with the center of the knee joint and the knee center to the center of the ankle. Under circumstances of normal alignment this should be a straight line. In a normally aligned knee, a line drawn from the hip center to the knee center should be co-linear with a line drawn from the knee center to the tibial plafond center. In a valgus or varus malaligned knee, these two lines will not be co-linear; the angle between these lines constitutes the angle of deformity (Figs. 55–1 and 55–2). The anatomic or femorotibial axis represents the angle formed between the lines of the femoral and tibial shafts. If there is doubt as to the ligamentous stability or the status of the contralateral compartment of the knee, stress films have been used to aid assessment. If there remains any question that the pain is due to the deformity, other investigations such as magnetic resonance imaging (MRI) and isotope bone scan may be employed.
Special Considerations
As mentioned earlier, valgus deformity is more common with certain inflammatory and metabolic conditions. If there is an undiagnosed but suspected presence of one of these conditions, further specific investigations are definitely warranted as such patients may not be best served by femoral osteotomy.
Preoperative Planning and Timing of Surgery
The medial closing wedge osteotomy is the most commonly described method of performing VDFO. Other techniques include the lateral opening wedge osteotomy, the dome osteotomy, and the gradual hemicallotasis technique. Methods of fixation include staples, external fixation, and the 90-degree angled blade plate, which is probably the most commonly used method today. Although external fixation has the potential advantages of the ability to fine-tune correction of the deformity and to gradually rather than abruptly stretch the peroneal nerve, we focus here on the techniques of medial closing wedge, lateral opening wedge, and osteotomy performed for extraarticular deformity.
In correcting the valgus malaligned knee, it is generally agreed that the goal should be to obtain an anatomic axis of 0 degrees, equating to a mechanical axis of 4 to 6 degrees of varus.7,8 This is to preferentially load the less involved medial compartment, and to allow for the common slight postoperative loss of correction.7 Careful templating is essential, and the correct wedge size to obtain the desired correction can be determined from the radi-ographic measures outlined above. The proposed internal fixation should also be templated on the preoperative radiographs.
Regarding extraarticular femoral deformity proximal to the knee joint, for example, following trauma, preopera-tive planning follows the same general principles. Additionally, though, on the AP x-ray of the femur, a line is drawn from the center of the greater trochanter distally down the center of the femoral canal. A second line is drawn from the center of the knee joint retrograde up the center of the femoral canal. The point and angle of intersection of the femoral axis proximal and distal to the point of extraarticular deformity approximates the center of angulation and the angle of deformity. The osteotomy is best performed at this site, provided that the bone and soft tissues in that region are not compromised. Great care is required in planning the exact size and orientation of the osteotomy here, however, and appreciation of the potential multiplanar nature of such deformity is essential. If there is compromise of either the soft tissues or bone in the area of deformity, then we recommend performing the osteotomy more distally at the metaphyseal-diaphyseal junction, where vascularity and healing potential are much better.
The metaphyseal-diaphyseal junction should also be the site of the osteotomy if one is considering performing a TKA either simultaneously or in a staged fashion. The main reason for this consideration is that the osteotomy fixation can be combined with the femoral component of the arthroplasty. For example, the femoral component could incorpoate an intramedullary rod, either press-fit or proximally and distally interlocked. Methods of fixation for the osteotomy alone may include an interlocked retrograde nail or external fixation, such as an Ilizarov or spatial frame.
As regards timing of the osteotomy, it is important to intervene early in the course of disease progression. Early intervention has been shown to maximize functional outcomes and potentially lessen the risk of disease progression.11,12
Patient and Equipment Position
The techniques described here are performed with the patient in the supine position with the leg routinely prepared and then draped free. A radiolucent table is required to enable intraoperative use of a fluoroscopic C-arm, which is necessary.
Anesthesia
There are no specific requirements for anesthesia; general or spinal anesthesia is suggested.
Surgical Procedure
Medial Closing Wedge Osteotomy
This is the most commonly described method of performing VDFO.6 A longitudinal midline incision is made from the tibial tubercle to 15 cm proximal to the patella. Dissection should then be carried down to the superficial fascia; then, a standard subvastus approach is performed to expose the periosteum. The periosteum is incised, and the distal femur is exposed subperiosteally. The subperiosteal dissection is performed distally to the proximal margin of the femoral condyles, proximal to the origin of the gastrocnemius. Most of the dissection is performed in the figure-of-four position (hip flexed and externally rotated, knee flexed). Proximal dissection should be performed carefully to avoid injury to the superficial femoral artery as it exits the adductor canal. We use an AO 90-degree angled blade plate with variable offset for fixation. The blade should be inserted 2 cm proximal to the articular surface of the distal femur. It should also lie in the anterior half of the medial femoral condyle to ensure that the side plate lies on the distal femoral shaft and does not slide off posteriorly. The step off between the blade and neck of the AO plate is ~2 cm, so that the osteotomy is performed somewhere between 2.5 to 3 cm proximal to the blade. This osteotomy site is marked by electrocautery (Figs. 55–3 and 55–4).
Three 3.2-mm Steinmann pins are then used to guide the osteotomy. Pin 1 is placed perpendicular to the shaft of the femur and inserted somewhat proximally. Pin 2 is placed more distally at the site of the osteotomy, such that the angle between these two pins equals the desired correction. During this step, it is advisable to use a sterile goniometer to measure the angle of the osteotomy. Pin 3 is placed distally within the femoral condyles and is parallel to pin 2; pin 3 guides the osteotomy and the insertion of the blade plate. The trough for the blade plate is prepared with the chisel and guide. The osteotomy is performed using an oscillating saw, thus creating a medially based wedge that is then removed. As the osteotomy site is closed, the first and third pin should become parallel. The blade is then inserted into the trough, followed by fixation of the side plate to the femoral shaft with cortical screws, using the techniques of dynamic compression. The bone wedge removed is morselized and used to bone graft the osteotomy site medially. Wound closure is routine, and we typically use a single Hemovac drain.
Lateral Opening Wedge Osteotomy
This technique was initially described by Postel and Langlais13 and performed through a standard lateral approach. The most common fixation device is the AO 95-degree angled plate. After exposing the femur subperiosteally, pin 1 is inserted perpendicular to the femur, proximal to the planned osteotomy site. Pin 2 is then inserted 2 cm proximal to the joint line at an angle equal to the preoperatively calculated deformity plus 5 degrees because the angle of the plate is 95 degrees. Again, as with the medial closing wedge technique, the osteotomy itself is generally performed 2.5 cm proximal to the blade plate and at an angle from the lateral femoral cortex equal to the deformity plus 5 degrees. The blade plate is first applied as described previously, followed by creation of the osteotomy. The medial cortex is left intact as a hinge. The lateral cortex is distracted open until it has reached the preoperatively templated distance; as this is performed, the medial side is automatically impacted. The side plate is then secured to the femoral shaft with cortical screws. Because the medial side of the osteotomy is impacted, some authors state that bone grafting is unnecessary.
Dressings and Braces
We routinely use a bulky Robert Jones dressing or knee immobilizer over the normal wound dressings (Fig. 55–5).
Tips and Pearls
Use of the C-arm is very important, as it facilitates the accurate placement and orientation of the osteotomy, ensuring, for instance, that the osteotomy is above the patellofemoral joint.
The opposite cortex should be kept intact at the time of the VDFO to maintain stability while fixing the plate. This cortex can then be cracked with correction of the deformity and fixation of the side plate. It is important to keep the site irrigated while performing the osteotomy to prevent thermal necrosis of the bone ends.
It is also probably advisable to take a slightly smaller wedge than planned with VDFOs, as there is a recognized tendency to overestimate the necessary wedge.9 The extracted bone wedge should also be morselized and used as graft at the osteotomy site.
Pitfalls and Complications
Nonunion of the osteotomy site has been significantly reduced by the introduction of more stable fixation techniques. Rates of reported nonunion have ranged from 0 to 8% with use of a medial 90-degree blade plate.7,14 Failure of fixation has also been largely overcome with the use of rigid internal fixation over staples as the method of fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








