11 Arthroscopic Abrasion Arthroplasty
The operation known as arthroscopic abrasion arthroplasty (AAA) was developed more than 25 years ago.1,2 It was a multiple tissue debridement procedure for patients with severe knee joint osteoarthritis. Like so many other arthroscopic procedures it was an adaptation of a known open operation, the Magnuson “house cleaning.”3
The term arthroscopic abrasion arthroplasty was chosen because it described each aspect of the procedure.1,2Arthroscopic refers to the surgical method used to perform the operation. Abrasion emphasizes the aspect of the procedure that is directed toward the sclerotic lesion. The novel method was a superficial debridement to remove the dead osteones and expose the vascularity, similar to dermabrasion. In one sense, the word arthroplasty indicated that many tissue types were debrided: synovectomy, chon-droplasty, meniscectomy, and osteophyte removal, as well as the localized abrasion of the sclerotic area. Arthroplasty also implied that there was a tissue repair documented by second-look arthroscopy and biopsy. Arthroplasty is defined as a remolding or reshaping of the joint surface, which occurred in many patients.4 The name was descriptive, but perhaps this procedure would have been better accepted if it simply were called an arthroscopic debride-ment. However, the simpler name would not have been an adequate description of this novel approach.
Abrasion was used as an alternative to drilling of the areas of exposed bone. Prior to that time, conventional wisdom presumed that the surface of exposed sclerotic bone associated with degenerative arthritis was devoid of blood supply.5–7 This belief led to the popular open surgical treatment using multiple deep drill holes in the lesion to reach the subchondral blood supply and stimulate a healing response. One such procedure, the so-called Insall-Pridie procedure, advocated even focal resection of the entire subchondral bone plate for the same purpose.8 Because the abrasion aspect accompanies many other tissue-type debridements in abrasion arthroplasty, it is not possible to know what specific clinical benefit the abrasion contributes.
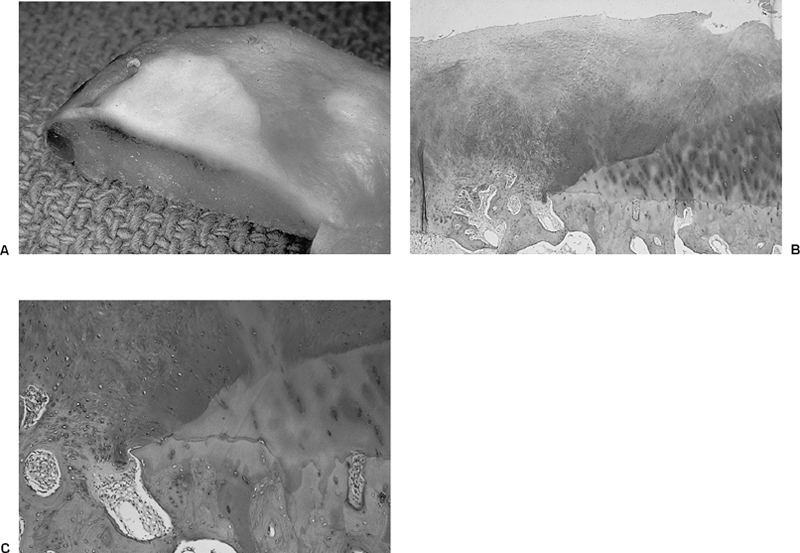
The arthroscopic surgical environment provided the opportunity to observe that the blood supply of the sclerotic lesion was at the surface and drilling deeper was not necessary to create bleeding.1,2 This was best visualized during fluid decompression of the joint by shutting off the inflow (Fig. 11–1). In addition, opportunistic arthroscopic observations showed some sclerotic lesions to have hemorrhaged as part of the natural history of this condition (Fig. 11–2). The spontaneous bleeding may well may be the first event in the natural history attempt to repair the sclerotic lesion. Patches of fibrocartilage are often seen on the surface of such lesions (Fig. 11–3). Pathologic inspection of tissue obtained during total knee surgery confirms the vascularity at the surface, and other specimens show the focal areas of reparative tissue dotting the surface of the sclerotic lesion (Fig. 11–4). It would appear that patients are trying to perform their own abrasion arthroplasty as the opposing joint surfaces rub on each other during weight bearing. This normal activity may result in abrasion, bleeding, and focal repair (Fig. 11–5). Support for this theory is based on the reports in the medical literature that show widening of the knee joint space following realignment tibial osteotomy. Unfortunately, these reports are absent the intraarticular documentation of the preoperative status or the nature of the repair tissue.9–12
It was also believed that little or no lasting tissue repair would occur following debridement procedures.13,14 The basis for this skepticism was Convey et al’s15 report that full-thickness lesions of a large diameter did not repair and led to degenerative arthritis. Tissue repair did occur and the gross appearance was not that of hyaline cartilage (Fig. 11–6). It is softer to palpation and not glistening in appearance. It often is whiter than the adjacent hyaline cartilage. The microscopic examination of the reparative fibrocartilage showed small cartilage cells, unorganized in matrix of histochemical positive staining with Safranin O (Figs. 11–6B,C, 11–7, and 11–8). The lamina splendens is often restored (Fig. 11–8A). The tidemark has been restored as early as 6 months (Fig. 11–8B). There were varying amounts of type II collagen found up to 5 years following surgery.2 Still, the biomechanical properties were not that of hyaline cartilage.
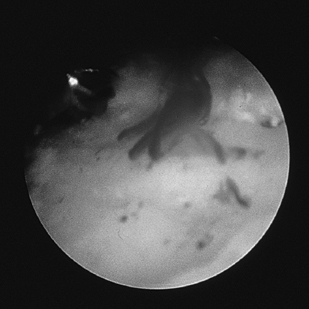
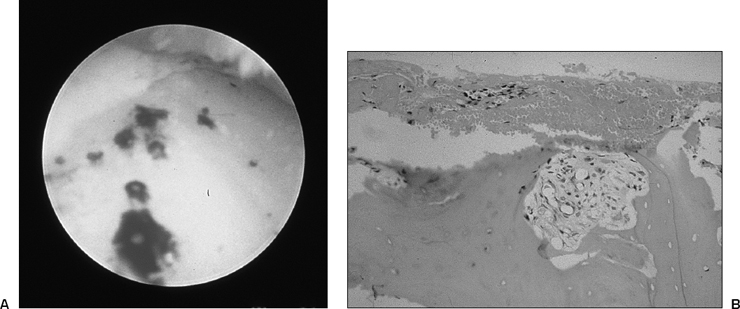
Figure 11-2 Natural pathologic history of sclerotic lesion with surface bleeding. (A) Arthroscopic view during diagnostic arthroscopy and prior to surgery shows naturally occurring hemorrhage on the surface of the sclerotic lesion (see Color Plate 11-2A). (B) Photomicrograph of biopsy of same lesion shows hemorrhage and blood clot attached to the surface of the sclerotic lesion (see Color Plate 11-2B). [Hematoxylin and eosin (H&E) × 100.]
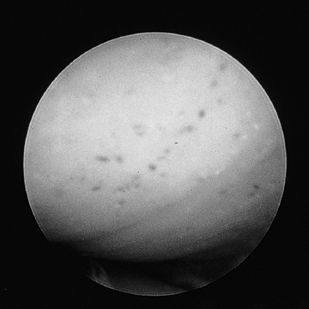
Figure 11-3 The sclerotic lesion. Arthroscopic view of sclerotic lesion on the femoral condyles of medial compartment. The lesion is yellow in color and has “dots” on the surface that represent the small vessels at the surface (see Color Plate 11–3).
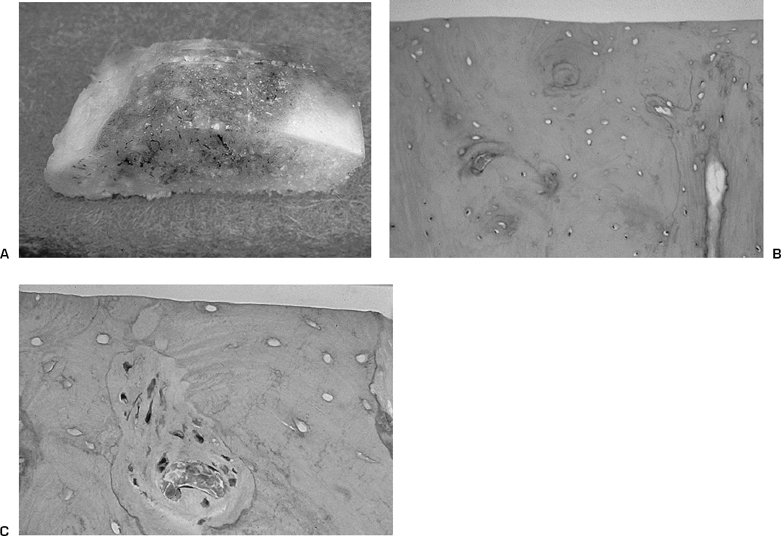
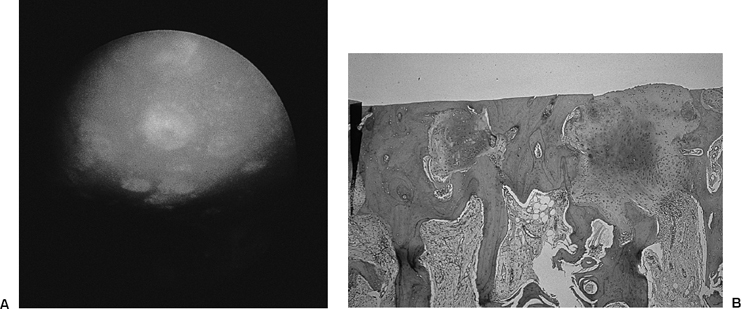
Figure 11-5 Natural history of the pathological attempt to resurface the sclerotic lesion. (A) Arthroscopic view of medial compartment shows the sclerotic lesion on femoral surface. Notice the small patches of fibrocartilage on the sclerotic lesion (see Color Plate 11-5A). (B) Photomicrograph of a similar sclerotic lesion showing patches of fibrocartilage in dense bone surface with hypervascularity below. (Safranin O × 40.) (See Color Plate 11-5B.)
Abrasion Arthroplasty as Compared to Microfracture Technique
Some of the confusion about AAA has been due to the subsequent introduction of the concept of microfracture.16 Abrasion was indicated for severe degenerative arthritis.2 Microfracture was introduced for the treatment of traumatic lesions. The AAA patient’s degenerative knee had exposed sclerotic lesions often on opposing surfaces. The traumatic lesion was usually isolated to one condyle. The degenerative lesion was often larger than 4 cm in diameter with little or no supporting shoulders of degenerative cartilage. The typical traumatic lesion is small in surface area with normal articular cartilage surrounding. The sclerotic lesion depth is to exposed bone. The traumatic lesion is typically to the level of the calcified cartilage. The surgical technique for AAA includes multiple tissue debridements. The surgical technique of microfracture typically accompanies reconstructive procedures on the ligaments. AAA includes a minimal surface abrasion of the sclerotic lesion to remove the dead osteones and expose the superficial vessels. No perforations are necessary to access bleeding. The original microfracture of necessity creates multiple perforations of the intact nonvascular calcified cartilage layer. There are two theoretical issues supporting the introduction of the concept of microfracture. First is that multiple penetrations have to be made into bone to access blood and the pluripotential cell. It is acknowledged that the penetrations were perceived necessary due to the intact avascular calcific cartilage layer. However, blood is present in the joint from injury and the subsequent surgery.17 It is not known what additional percentage of blood is contributed from the bone punctures. Therefore, only the issue of the pluripo-tential cell contribution needs to be validated as a benefit. There is no evidence that the microfracture increases the initial fixation of the blood clot. The second hypothetical is that the microfracture creates improved subsequent fixation of the repair tissue. No confirming or comparative study has been published. Although an opportunistic patellar surgical specimen following patellectomy shows that drill holes 4 mm in diameter and 8 mm deep will maintain a fibrous tissue plug for up to 1 year.2 The common denominator is that the blood clot must be protected, housed, and held in place until cellularity occurs. Non-weight-bearing ambulation is an effective method of achieving that end. It is not known if the blood clot in the puncture wounds following microfracture contributes to the fixation during the cellular maturation phase. It is not known if the bone penetrations retain fibrous tissue continuity with the surface. It is known that after abrasion arthroplasty the tissue remodeling is considerable and there are well-defined layers of tissue interfaces (Fig. 11–6). Recently Steadman has advocated including the abrasion technique to remove all the calcified cartilage in the trauma cases. The value of adding the abrasion to the microfracture is supported by laboratory studies mentioned above.18 Fibrocartilage tissue growth has been observed by second-look arthroscopy and confirmed by biopsy following both techniques.2,16 Since both surgical methods are presently so similar, the results would be anticipated to be similar when applied to a sclerotic lesion. Both methods have advanced the repair of articular cartilage surfaces and hold the possibility of opening the pathway to cartilage restoration. The necessity of treating these cartilage lesions associated with ligament injury is questioned by a recent natural history study.19
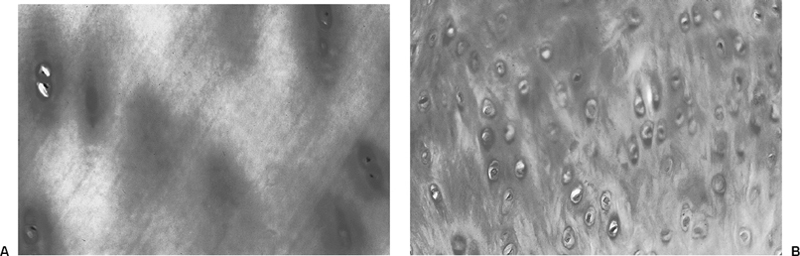
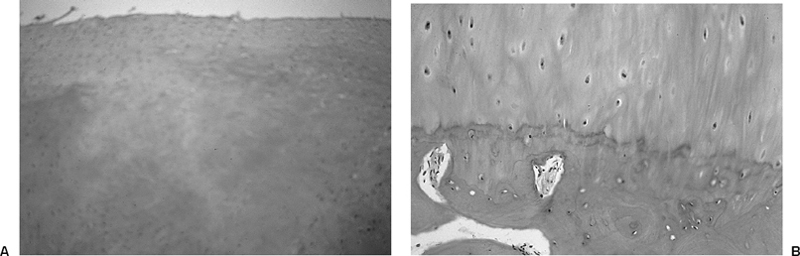
Figure 11-8 Second-look arthroscopy at 5 years following abrasion arthroplasty provides biopsy specimen. (A) Photomicrograph biopsy shows the surface of the regenerated fibrocartilage. There is a lamina splendins and fibrocartilage that is positive stained histochemically for mucopolysaccharides. (Safranin O × 40.) (See Color Plate 11-8A.) (B) Photomicrograph of regenerated tidemark at 5 years following abrasion arthroplasty. (Safranin O × 100.) (See Color Plate 11-8B.)
Controversy
Unfortunately, some 25 years after the introduction of AAA the procedure is still cloaked with misunderstandings and remains a controversial topic. The purpose of this chapter is to dispel, if possible, the confusion surrounding AAA in hopes of correcting misinformation, persistent misunderstandings, and misconceptions. This report includes what has been published, but more importantly new information is available from searching a database from an evidence-based clinical practice.
This new information is timely because a recent publication concluded that arthroscopic debridement for degenerative arthritis produced no different result than sham surgery in a double-blinded study on volunteers at a Veterans Administration hospital.20 This report stimulated controversy and numerous responses in the medical and lay literature.21–28 There are conflicting opinions. Jackson and Dieterichs28 reported a 4- to 6-year symptomatic review and concluded that patients with less severe osteoarthritis do better than those with advanced changes. They also supported the minimal debridement on the depth of articular cartilage lesions. Others reported there is a place for arthroscopic debridement in selective cases.29
It is important to note that there are marked differences between the detail of the data reported in the New England Journal of Medicine article25 and what exists in this clinical database on patients undergoing AAA. One group was composed of volunteers at a Veterans Administration hospital. Those in the clinical database were private patients. The volunteers were described only as having knee pain and x-ray evidence of osteoarthritis of the knee.20 The AAA cohort selected for this review in an evidence-based clinical practice were private patients with knee pain and x-ray evidence of severe osteoarthritis of the knee. In addition, the AAA patients had selected themselves, as they were advised that they were candidates for total knee arthroplasty. They were seeking an alternative treatment. The physical findings of those in the research report are not known.20 The physical findings of the AAA clinical cohort are detailed and are reported below. The severity of the osteoarthritis is not known for the research group since the intraoperative findings are not known.20 Those undergoing AAA had severe osteoarthritis of the knee with exposed bone on one or more condyles. The detailed intraoperative lesions on the AAA patients are documented below in this report. The therapeutic procedure performed on the experimental volunteers was recorded only as a lavage and debridement.20 The database on the clinical AAA experience was detailed as to tissue type, and the extent of the debridement is known and reported below. The question remains as to what was wrong with these volunteers and what was performed surgically.20
It does not appear possible to compare the two groups concerning material or methods due to lack of information in the controlled research study.20 It would be possible to say that both groups had pain and degenerative arthritis of the knee and had arthroscopic debridement. The comparison is being made between the outcomes of patients with osteoarthritis of unknown magnitude treated with lavage and debridement of a unknown type and the outcomes of a cohort of clinical patients, all of whom had documented severe degenerative arthritis of the knee and a carefully described operative tissue debridement.
Much of the following report is supported by the recent database search of information collected in the course of a clinical private practice. Therefore, this report is based on facts.
Indications
Abrasion arthroplasty is indicated for a patient seeking an alternative to total knee replacement. This patient has known severe degenerative arthritis of the knee confirmed by plain film x-ray. The diagnosis is confirmed by arthroscopy, with the presence of a sclerotic lesion on one or more condyle.
The recent database search showed 556 patients with initial clinical evaluation data who presented for an abrasion arthroplasty. The average age of the patients was 54 years. The range was 13 to 88 years. The youngest patient had previously lost all his articular cartilage during an adverse surgical event performed in another state that included the erroneous use of heated dilute acidic acid as an irrigating fluid. There were 343 females and 213 males. The lifestyle of the patients was sedentary in 26%, moderate in 14%, and vigorous in 0.1%. The self-assessment of their health was excellent in 21%, very good in 35%, good in 34%, fair in 7%, and poor in 0%. The type of work was student, 2%; homemaker, 5%; sedentary, 8%; physical, 14%; and retired, 13%. Ninety-five percent of the patients had private insurance. There were 3% workers’ compensation and 0.2% third-party liability cases.
The chief complaints were multiple in each patient, summarized as follows: pain, 70%; swelling, 40%; aching/sore, 39%; loss of activities, 26%; limping, 24%; grinding, 22%; loss of motion, 18%; and loss of work, 4%.
The previous surgical treatment was recorded in 63% of these patients, which included arthroscopic surgery in 32%, open surgery in 21%, and both in 10%. Nineteen percent had seen a specialist for nonoperative treatment, and 6% had previous physical therapy.
It would be helpful to know what conditions would predict a positive outcome and therefore shape the indications. There were no positive predictive characteristics observed that could affect patient selection. There was no relationship between the result and the age, the sex, existence of previous surgery, the side involved, the anatomic site of the lesion, the size of the lesion, the combination of the lesion sites, the extent of the multiple tissue debridement, the existence of mild varus or valgus, or the presence of a meniscus in the compartment.2
Steadman’s group30 reported that in traumatic cases a better outcome was observed in patients who were younger than 30, with normal alignment, acute lesions, and isolated defects, and who used continuous passive motion postoperatively. It has been reported that a lesion size of over 300 mm2 was not a predictor.
Bert and Maschka31 reported no relationship between the fibrocartilaginous tissue growth and the clinical result.
Contraindications
It was observed early on in the clinical experience with abrasion arthroplasty that patients with severe malalignment, ligamentous instability, and morbid obesity did not do well. Based on the initial results, these conditions are now considered contraindications. Ankylosis is also a contraindication, as is an active infection. The results are not predictable in workers’ compensation or third-party liability cases. It should not be performed in patients unable or unwilling to undergo 8 weeks of postoperative non—weight-bearing ambulation.
It also should be emphasized that an abrasion it is not intended for removal of intact degenerative articular cartilage. Only a superficial removal for loose cartilage fragments was performed.1,2
Physical Examination
The physical examination records showed a limp in 18%, bent knee gait in 12%, minimal limited range of motion in 55%, and effusion in 26%.
Diagnostic Tests
The typical preoperative tests included bilateral plain film x-rays: standing at extension and 45-degree flexion, Merchant patellar views, and supine and lateral views.2,32
Special Considerations
- The patient should have something wrong in the knee that produces symptoms. This statement may sound obvious, but instead it emphasizes the necessity to document clinical and surgical findings because a report that does not contain this critical information would be open to challenge.20
- Pathologic lesions By way of contrast, extensive clinical data are available to show the incidence of pathologic lesions in the clinical cohort undergoing arthroscopic debridement for degenerative arthritis of the knee. The intraoperative findings were complex and multiple in all patients. The findings were summarized as follows: excessive joint fluid, 52%; loose bodies, 41%; significant synovitis, 74%; torn medial meniscus, 80%; torn lateral meniscus, 46%. The data show these patients had significant other symptom-producing lesions as well as the exposed sclerotic bone confirming the severe degenerative status.
- Specific tissue debridement The debridement procedure was well defined in this database and included multiple tissue debridement, which was potentially symptom producing. The common denominator of the debridement in each case was the localized abrasion arthroplasty. In addition, the following summary reflects the multiple and varied nature of the lesions treated. There was loose body removal in 43%, limited synovectomy in 90%, and extensive synovectomy in 10%. There was localized partial-thickness chondroplasty performed superficially in 12%; half-thickness depth chondroplasty in 68%, and the chondroplasty of loose cartilage extend to the bone in 9%. There was 59% partial medial meniscectomy; 26% partial lateral meniscectomy; and 15% had both meniscal tears removed; 39% had resection of osteo-phytes.
- The not so special considerations should include the presence of symptom-producing intraarticular lesions amenable to debridement.
Preoperative Planning and Timing of Surgery
There is no critical timing for abrasion arthroplasty. To assess the initial patient management a search was performed on the data from the first patient encounter and disposition. All patients had an indication for a total knee replacement. Of this group that eventually came to arthroscopic debridement, 26% were scheduled at the initial visit, and 33% were advised at the initial encounter that this surgery was a future consideration. The others were advised that surgery was medically indicated. There was no rush to surgery. The patients were advised of the treatment alternatives and scheduled only after they arrived at the decision.
Special Instruments
The procedure is performed in an arthroscopic environment. It is best performed with motorized instrumentation rather than hand tools. The motorized instrumentation is available from Smith & Nephew Endoscopy (150 Minuteman Road, Andover, MA 08180). The motorized instruments provide for precision in the debridement depth and simultaneous tissue removal. They facilitate removing the loose articular cartilage margins of the lesion with unidirectional burr rotation that promotes repair tissue attachment to the adjacent intact cartilage.2 A variety of cutting tools are used and are often tissue type specific. A small rotating burr is favored over a curette for the above reasons.2 Some have advocated using hand instrumentation to create the abrasion.16 Other energy sources have been introduced. Recently two malpractice cases surfaced where the surgeons allegedly “followed Dr. Johnson’s abrasion technique” but with laser energy applied to the bone for the abrasion. Not unexpectedly, there was bone necrosis and increased morbidity. Litigation was settled in favor of the plaintiff in both cases.
Anesthesia
General anesthesia was the most common type. In some cases spinal or epidural was used for medical reasons. Rarely was local anesthesia used for this procedure, as the multiple tissue debridement was time-consuming.
Patient and Equipment Positions
The patient was placed in the supine position. The thigh was secured to the operating table with a Surgical Assistant clamping device (Smith & Nephew Endoscopy). The draping is such that it provides for arthroscopic approaches to the posterior compartments and the popliteal bursa. The foot of the table was dropped so that the knee could be flexed and extended.
Surgical Procedure
The surgical approach is via multiple portals.2 The procedure is initiated with an anterior lateral arthroscope portal followed by interchange of instrumentation and arthroscope to access the various compartments. Posterior approaches are often indicated.
Dressings, Braces, Splints, and Casts
A simple compression bandage is used. No closure is made of the puncture wounds, as they are small. The open wound allows for intraarticular fluids to exit. Drains are not necessary.
Discussion
One should not be misled by the recent New England Journal of Medicine report that arthroscopy is of no value in degenerative arthritis of the knee.20 This report on volunteers in a veterans hospital was lacking supportive documentation and information on the physical findings, the intraarticular pathology, and the specific tissue debridement performed. Without such information, their conclusion must be challenged. The following important findings are present in the evidence-based clinical practice database cited above. Not unexpectedly the results are different from those reported by Moseley et al.20
Patient Selection
Patient selection is critical to a successful outcome. Candidates for AAA should be seeking an alternative to total knee replacement. They should have severe degenerative arthritis of the knee plus clinical evidence of symptom-producing lesions amenable to debridement. The anticipated surgical debridement includes multiple tissues plus the abrasion.
Depth of the Abrasion
The depth of the abrasion is the most misunderstood aspect of this procedure. Traditional teaching was that the bone must be penetrated to gain access to the vascularity. That is not so. The blood supply is at the surface of a sclerotic lesion (Figs. 11–1 to 11–5). The superficial abrasion removes the dead osteones, creating a live tissue bed for a blood clot supplied from the exposure of vessels in the bone and bleeding from the synovium around the arthroscopic portals.17
Success Criteria Achieved
Ninety-five percent of patients achieved their objective of deferring a total knee replacement for up to 5 years.1,2,33 Admittedly this result was influenced by the fact they did not want a total knee replacement in the first place. The clinical benefits are probably due to the meniscectomy and removal of inflamed synovium and large fragments of articular cartilage including loose bodies.34
Palliative Procedure
It should not be proposed to the patient that AAA is curative.1,2,33 Although most patients achieve the objective of avoiding or deferring a total knee replacement, 66% of the patients still had symptoms. Notably, 99% reported continued activity restriction.
There were 143 patients in this recent cohort making 358 reports at 2 years or more following surgery, at which time 63% said they were improved, 4% said they were the same, and 9% said they were worse than before surgery. When asked specifically about existing clinical problems at 2 years or more following surgery, 34% reported they had none. That would include not having pain. This is in sharp contrast to Moseley et al’s20 conclusions. The remainder of the responses are shown in Table 11–1.
| No complaint | 34% |
| No pain | 30% |
| No activity limitation | 13% |
| No swelling | 22% |
| Walks normal | 32% |
| Range of motio n the same | 41% |
| No stiffness | 18% |
| No grating | 26% |
| No locking | 53% |
| No buckling | 50% |
| No aid to walking | 74% |
∗This database included 358 postoperative evaluations on the 143 patients between 2 and 10 years. The discrepancies in percentages are due to patient answering no to general question and erroneously responding with a yes to subsequent related subheading questions.
Specific Areas of Benefit
Various areas of improvement were evaluated after 2 years. All patients (100%) had a preoperative complaint of some type. After 2 years the incidence fell to 66%. All had activity limitation and subsequently 87% were still limited. The incidence of swelling went from 92 to 78%; normal walking from 79 to 68%; range of motion improved 10%; stiffness went from 99 to 82%; grating went from 85 to 76%; locking occurred in 50% and was reduced to 47%; buckling occurred in 60% and was reduced to 50%; aids to walking were used by 37% preoperatively and 26% after 2 years.
Extensive Assessment of Effect of Arthroscopic Abrasion Arthroplasty on Pain
There were 710 patients who had an abrasion of any size or location; 41% (n = 289 patients) had a follow-up evaluation in the database at 1 to 10 years.
At the initial patient encounter, 92% of patients who were to subsequently undergo an abrasion arthroplasty indicated they had pain as one of their major complaints; 43% of this group had an initial postsurgery follow-up evaluation in the database at between 1 and 10 years; 32% of all patients at follow-up between 1 and 10 years indicated pain was a major complaint. At year 1, 30% indicated they still had pain.
To further evaluate the issue of pain, the patients were divided into three groups based on the size of the lesion having an abrasion: small, moderate, and large. The database was searched for any response to pain in the follow-up forms at 1 to 10 years so as not to overlook any positive response; 32% of those patients with only a small abrasion group had pain, 38.5% of those with only a moderate-size abrasion had pain, and 38.8% of those with a large abrasion had pain. These clinical patients’ responding to improvement in pain differed from the research report that said there was no pain benefit.20 Something must be different, but such a determination is not possible to make due to the lack of important information in Moseley et al’s20 report.
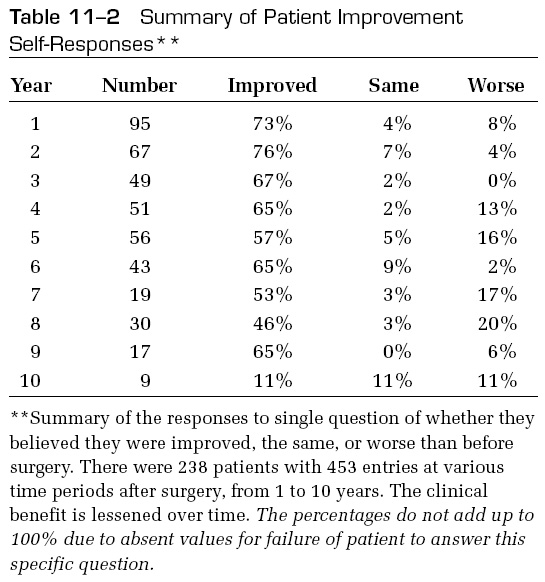
Lessened Benefit Over Time
This database search showed that the percentage reporting improvement over their preoperative status lessened over time. There were 238 patients whose clinical findings had 453 follow-up reports at 1 year or more. The improved response went from 73% in year 1 to 53% by year 7 and down to 11% by year 10 (Table 11-2). It should be noted that the number of patients responding dropped in the last few years of the study, due to time lapse and attrition due to the elderly cohort.
Physical Examination Results
At 2 years 42 patients were examined; 52% had no stiffness or swelling, and 25% had stiffness and swelling after activity1 Seven of the 42 patients still used a cane. In 55% crepitus existed at 2 years and in 90% at 5 years. There was minimal loss of range of motion, with an average loss of 4.5 degrees extension and flexion to 122 degrees at 5 years.12,33
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








