Fig. 1
MRA image of a left hip reveals disruption of the posterior acetabulum (arrow). This was initially interpreted as a posterior labral tear but actually represents a posterior rim fracture (©2014 J. W. Thomas Byrd, MD)
Computed tomography (CT) can confirm the presence of a fracture and may be helpful for assessing the congruency of joint space reduction and some intra-articular fragments.
Treatment
Nonoperative Management
Most traumatic instability can be treated nonoperatively. Of course, dislocations require emergent reduction to minimize the risk of developing avascular necrosis of the femoral head. Unless there is a compelling reason for arthroscopic intervention, such as a nonconcentric reduction or obvious entrapped fragment, an initial trial of conservative treatment is preferable. Three months is a reasonable time frame for resolution of the acute phase of the injury and a clearer assessment of whether an athlete continues to have mechanical symptoms or clinical findings that may warrant arthroscopic intervention. In addition to subsidence of acute symptoms, this is an opportunity for some intra-articular damage to declare itself. For example, impaction injury to the articular surface of the femoral head may lead to subsequent chondrocyte cell death and articular delamination that may not be evidently close to the time of the initial injury. Arthroscopy , at a later date, may provide a clearer reflection of the severity of intra-articular pathology. Often the injuries heal, arthroscopy is not necessary, and athletes can resume sporting activities without symptoms. Long-term consequences may still be less certain, and thus athletes are educated about warning signs of symptoms that might warrant reevaluation in the future.
The presence of a posterior rim fracture does little to alter the treatment strategy, or likely outcomes, of posterior subluxation episodes. The fracture may only partially heal or develop a fibrous union, but this is rarely a source of residual symptoms or cause for surgical intervention. Surgery is usually necessitated due to other intra-articular pathology.
Most patients with posterior subluxations recover well and can resume athletic activities (Fig. 2). However, some do poorly, with rapidly progressive joint deterioration, and can be facing an arthroplasty even within a year of the index injury (Fig. 3). There are few indicators to predict which will do well and which may rapidly decline. Thus, a deliberate, responsible rehab strategy is important for all cases. A protocol is outlined in Table 1. Protective weight bearing is maintained for 4 weeks, during which time hip flexion is limited to 90°. A follow-up MRI is performed at 1 month, looking for resolution of soft tissue edema and any joint effusion. Subchondral edema may start to develop in the femoral head as an indication of the impaction injury to the joint surface. This is common and is not necessarily a harbinger of poor results or an indication of early AVN [19]. In the cases of posterior rim fractures, a follow-up CT scan can be helpful just to assure that no further displacement has occurred. Loaded hip flexion is avoided until 6 weeks, and then the athlete is progressed with a functional program as symptoms allow. Return to unrestricted activities at 8–10 weeks is not unreasonable, as long as the athlete remains pain-free. A later MRI may be obtained to rule out signs of late onset avascular necrosis.
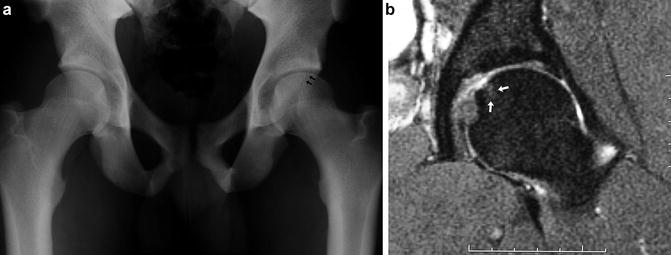

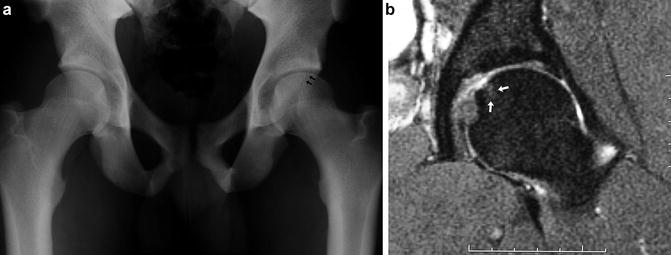
Fig. 2
A 20-year-old NFL rookie defensive back sustained an acute injury to his left hip in the first quarter of a game. He completed the game and then was evaluated for persistent pain. (a). AP radiograph reveals a posterior rim fracture (arrows). (b). Follow-up MRI at 6 weeks reveals localized superomedial area of subchondral edema in the femoral head on T2 coronal images indicative of concomitant impaction injury to the femoral head. This had no residual consequences as he returned to play at 7 weeks post-injury and has had a 10+-year career including several Pro Bowl appearances (©2014 J. W. Thomas Byrd, MD)

Fig. 3
A 31-year-old NFL wide receiver sustained an acute injury to his left hip. (a). 3D-CT image reveals a small posterior rim fracture (arrows). (b). However, within 3 weeks, an AP radiograph shows evidence of early joint space narrowing of the left compared to the uninjured right hip. (c). Follow-up coronal MRI shows significant subchondral edema of the femoral head with concomitant articular loss and persistent pronounced effusion. He developed quickly progressive posttraumatic osteoarthritis culminating in a resurfacing arthroplasty 1 year following his index injury (©2014 J. W. Thomas Byrd, MD)
Table 1
Hip Luxation Protocol
Hip Luxation Protocol (Stable Posterior Acetabular Fracture) |
Initial x-rays, CT scan & MRI (high-resolution!) |
Stable fracture pattern without obvious major intraarticular damage, then candidate for conservative treatment |
Crutches, partial WB 4 weeks |
Minimize risk of fracture displacement |
Slight loading stimulates healing process |
At 4 weeks fracture should be “sticky” |
4 weeks |
Limited CT scan |
Check for signs of displacement |
Alignment good & painfree, then transition off crutches |
Follow-up MRI |
Check for resolution of soft tissue edema |
Check for early signs of subchondral femoral edema (bone bruise) indicative of FH impaction injury |
May necessitate more conservative approach because of uncertain prognostic significance |
4–6 weeks, avoid loading of flexed hip |
Functional progression at 6 weeks, if pain-free |
Return to unrestricted activities 8–10 weeks, if pain-free |
F/U x-rays at 1, 2, 3 & 6 months |
F/U MRI 3 & 6 months |
Assess for early signs of AVN |
Assess for progression/resolution of subchondral edema, if present |
F/U CT scan, if needed due to symptoms |
Bony bridging of fracture often partial/incomplete |
May develop asymptomatic fibrous union |
Acute Surgical Management
There are many complex fractures that may warrant early ORIF, but that is not the subject of this chapter. Early arthroscopy may be indicated for a nonconcentric reduction or entrapped fragments (Fig. 4). Commonly, arthroscopy will reveal more extensive damage than that identified by the imaging. This tendency of MRI to underestimate the damage should be kept in mind, as some athletes who fail to respond to conservative care may have more occult joint pathology. The timing of surgery should also take into consideration concerns about soft tissue extravasation. Normally, the risk of extravasation should not be any greater than that encountered in association with other extensive arthroscopic procedures to correct FAI that often involve large capsular exposures. Early arthroscopy should be avoided when there is an acetabular fracture that communicates with the intrapelvic region [20].
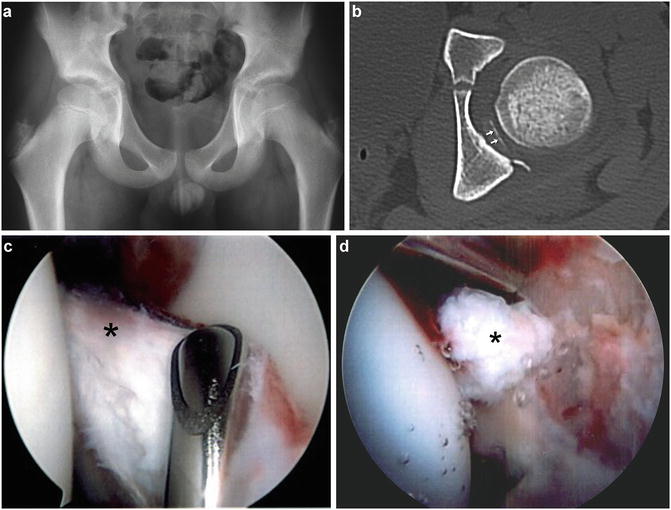
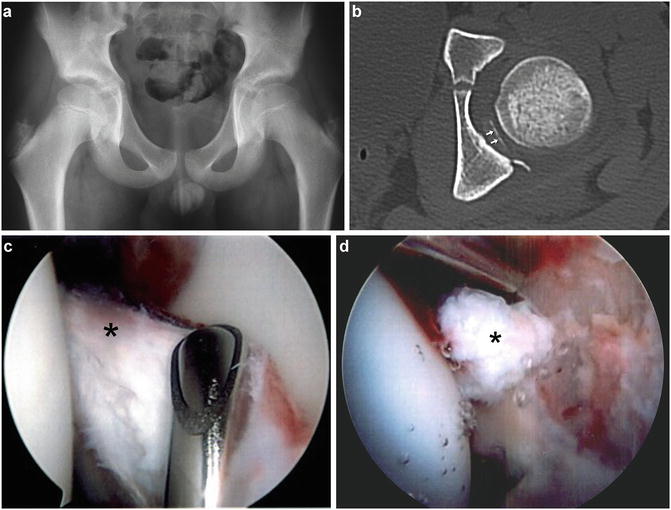
Fig. 4




A 10-year-old male sustained an acute left hip injury when involved in a pileup during a football game. Subsequently, he was unable to bear weight because of pain. (a). AP radiograph reveals open physes and a seemingly concentric reduction. (b). CT scan reveals an entrapped fragment (arrows). (c). Arthroscopic view from the anterolateral portal reveals the fragment (asterisk). This was attached to the posterior capsule, which was also entrapped within the joint. The fragment was excised and capsule reduced with an uneventful recovery. (d). Also noted was a rupture of the ligamentum teres (asterisk) which was debrided (©2014 J. W. Thomas Byrd, MD)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








