Fig. 1
CT AP view of type I AIIS variant in a left hip. There is a smooth ilium wall between the caudad level of the AIIS and the acetabular rim

Fig. 2
CT AP view of type II AIIS variant in a left hip. Bony prominences (black arrow) are present on the ilium wall extending from the caudad area of the AIIS to the acetabular rim

Fig. 3
CT AP view of type III AIIS variant in a left hip. The AIIS (white arrow) extends distally to the anterosuperior acetabular rim, characterized by a downward “spur appearance”
Systematic Approach to the Evaluation and Surgical Treatment
A systematic approach for each patient who presents with symptomatic FAI and possible subspine impingement should include combined information of a detailed history, an anatomically based clinical examination, and the interpretation of clinically relevant findings of all available imaging modalities. These diagnostic tools will enable the clinician to successfully make a “four-layered” – osteochondral, inert, contractile, and neuromechanical layer – diagnosis, which is essential to formulate a safe and successful treatment plan [31–33].
Clinical Presentation
The clinical presentation in patients with subspine impingement includes tenderness to palpation over the AIIS that recreates typical pain and anterior hip or groin pain with straight or prolonged hip flexion [34]. On physical examination, hip flexion range of motion is limited. Partial pain relief and persistent hip flexion limitations after intra-articular anesthetic hip injection may be observed [6]. This may be explained by the fact the AIIS deformity may not have been the single cause for the preoperative symptoms since studies have shown the concomitant presence of abnormal cam morphology [35]. Furthermore, cam lesions may have contributed to anterior impingement against the AIIS, consistent with recent studies that showed that impingement in such cases, when the hip was flexed to greater than 90°, occurred between the AIIS prominence and the anterior aspect of the femoral neck [6–8, 36]. In the presence of intra-articular FAI, the minimal relief of groin and/or anterior pain during straight hip flexion after intra-articular injection of a local anesthetic implies the coexistence of extra-articular subspine impingement [37]. Such cases combining both intra- and extra-articular deformity/impingement underscore the significant advantage of using the arthroscopic approach to decompress an abnormal AIIS, which enables the surgeon to address simultaneously all potential intra- and extra-articular sources of hip pathology.
Imaging Modalities
Radiographs may reveal calcification within the direct or indirect head of the rectus femoris origin, evidence of prior AIIS avulsion injury (Fig. 4), a prominent AIIS deformity, extending to the level of or caudad to the level of the anterior–superior acetabular rim (on AP view of the pelvis and lateral view of the femur), excessive anterior and distal extension of AIIS viewed on false-profile view, crossover sign with increased anterior acetabular rim sclerosis (on AP view of the pelvis), and impingement cysts located at the distal femoral neck (Fig. 5) [6–8, 38]. Impingement cysts in AIIS/subspine impingement are located more distal on the femoral neck than typically seen with FAI impingement [6–8, 39]. The 3D computed tomography (CT) images are invaluable tool for preoperative assessment [6–8]. The 3D surface rendering computed tomography images could delineate the shape and deformity of the AIIS facilitating the classification and consequently generating the appropriate for each patient surgical plan. They could provide the clinician with the specific location of osseous impingement and the unique pattern of FAI impingement in each patient (Figs. 1, 2, 3, 6, and 7a, b). Magnetic resonance imaging (MRI) may also demonstrate abnormalities of the AIIS or subspine area. This area should always be evaluated on hip MR examinations in addition to the cartilage, labrum, capsule, and periarticular soft tissues such as tendons, muscles, and bursae (Fig. 8) [34]. Except for radiography, CT, and MRI, advanced dynamic imaging modalities such as dynamic ultrasonography and three-dimensional dynamic imaging analysis could facilitate the assessment of subspine impingement. A CT-based, dynamic computer model software program (A2 Surgical, Saint-Pierred’Allevard, France) [6–8, 40] allows the execution of motion paths that may be unique for each painful hip. Reproduction of zones of proximal femoral and prominent AIIS and/or acetabular bone-to-bone contact, via straight flexion beyond 90°, offers great insights for preoperative planning and could tailor the appropriate treatment of each patient (Fig. 9a, b) [41].


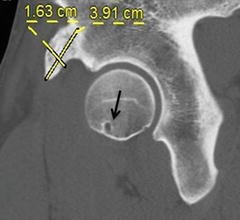
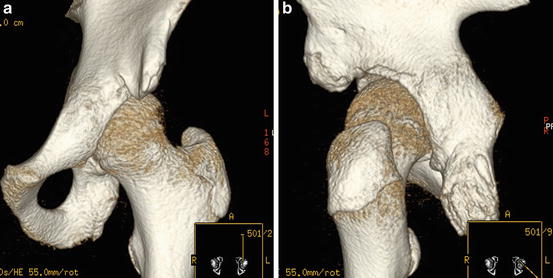
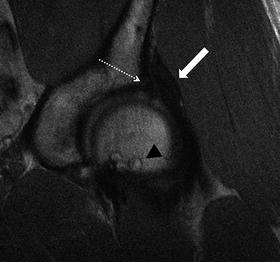
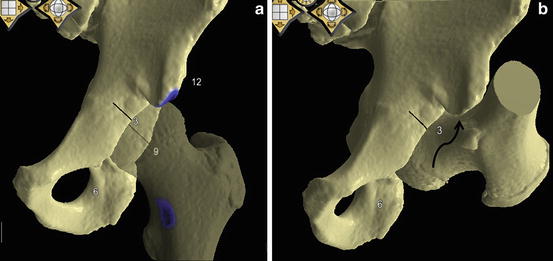

Fig. 4
AP view of the pelvis demonstrating calcification of the rectus femoris origin (arrow) in the left hip in an athlete with a history of chronic avulsion of the direct head of the rectus femoris that was treated nonoperatively

Fig. 5
Lateral view of the left hip of a patient with a history of chronic avulsion of the direct head of the rectus femoris. Prominent AIIS (arrow) extending caudad to the level of the anterosuperior acetabular rim, and herniation pits (dotted arrow) at the distal femoral neck confirm the presence of subspine impingement
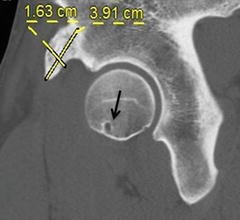
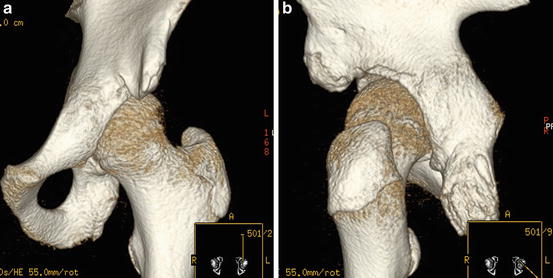
Fig. 7
a–b The prominent AIIS is well demonstrated in the 3D CT reconstruction AP view (a) and the “ischium AIIS” view (b) of this left hip before arthroscopic subspine decompression was performed
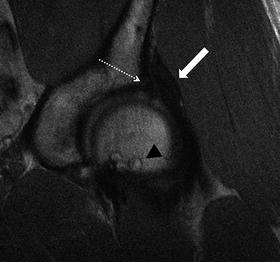
Fig. 8
MRI coronal view of a left hip (same patient with Figs. 4, 5, and 6) revealing thickening of the rectus femoris (arrow) secondary to chronic avulsion of the direct head of the rectus femoris that was treated nonoperatively, anterosuperior labral tear (dotted arrow) and associated herniation pits (arrowheads) at the distal femoral neck
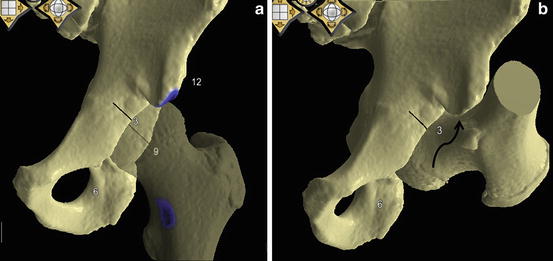
Fig. 9
a–b CT-based dynamic software images of a left hip showing areas of impingement between a type III AIIS (extending caudad to the level of the anterosuperior acetabular rim) and the distal femoral neck. (a) Hip in neutral position. The blue color highlights the area of bony impingement of the AIIS against the inferior part of the femoral neck with straight flexion. (b) Hip in 112° of flexion. The curved arrow illustrates the area of AIIS impingement
Treatment: Arthroscopic Approach
Decompression of a symptomatic AIIS prominence was described in the past, through the Smith-Petersen approach, either as a single procedure [24] or after arthroscopic exploration of the joint [36], but recently, the concept of arthroscopic decompression has been popularized in several studies demonstrating satisfactory short-term results [6–8, 30]. The rationale of arthroscopic decompression of prominent AIIS is supported by short-term outcomes series showing improvement in hip function and ROM [8]. This type of extra-articular arthroscopic procedure appears to be safe given that no associated complications have been reported. Despite the proximal and possible medial dissection of the capsule, no cases of fluid extravasation into the abdomen or retroperitoneum were observed. Furthermore, no cases of postoperative hip flexion weakness, complete detachment of the direct head of rectus femoris insertion from the AIIS, or formation of heterotopic ossification (HO) have been described. The concept of arthroscopic subspine decompression in AIIS variants that extend to and below the acetabular rim is further emphasized by a recent study [7]. In a cohort where FAI patients were matched for age, femoral version, and alpha angles, a CT-based dynamic computer model revealed that these prominent types of AIIS were associated with a decrease in hip flexion and internal rotation compared to the normal AIIS variants [7].
The significant advantage of arthroscopic approach is that it allows the hip surgeon to address patients with coexisting intra- and extra-articular causes of hip pain by utilizing a single arthroscopic procedure [6–8]. Preoperative planning is of paramount importance and should include 3D CT reconstruction views to evaluate the extension of the AIIS prominence, both anteriorly and distally. Should a cam deformity be present, concomitant decompression could be performed to increase the range of straight flexion without bone-to-bone contact. Any intra-articular abnormalities, such as labral or chondral injury, should be addressed as well to optimize the surgical outcome. The development of advanced and less invasive arthroscopic techniques, including extensile arthroscopic capsulotomies, has improved the central and peripheral compartment access and visualization facilitating, therefore, acetabular rim and AIIS evaluation and resection, treatment of labral and chondral injury, and osteoplasty for cam decompression.
Surgical Technique
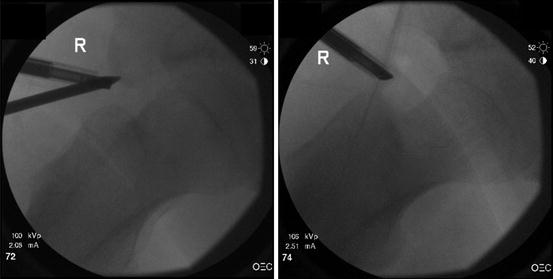
The positioning of the patient depends on surgeon preference, but for both supine and lateral positions, the feet should be well padded, and a large perineal pad should be used to optimize distraction and to minimize traction-related complications, such as pudendal nerve injury. Adequate distraction results in approximately 10 mm of joint space opening confirmed by fluoroscopy. Majority of surgeons utilize either two or three portals depending on their preoperative plan and preference. The two most widely accepted portals are the anterolateral (lateral) and the true anterior or modified anterior portal. Additional used portals are the distal anterolateral accessory portal (DALA) and various percutaneous distal portals that facilitate the anchor placement, especially in the anterior acetabular rim, suture management, and work (femoroplasty and capsule closure) in the peripheral compartment. The aforementioned portals allow better visualization and safe access to the hip joint [42]. The anterolateral pertrochanteric portal is established first under fluoroscopic guidance, followed by the mid-anterior portal (slightly more lateral to the traditional anterior to avoid injury to the lateral femoral cutaneous nerve) under arthroscopic visualization from the lateral portal. The mid-anterior portal may be placed more distally in cases with AIIS impingement in order to facilitate access to the anterior portion of the joint. Care should be taken to keep minimum 6–7 cm between the portals, which will allow sufficient working space between instruments. Having established the lateral and mid-anterior portals, based on each patient’s individual bone anatomy, a diagnostic arthroscopy is performed to evaluate the labrum, capsule, femoral head and acetabular cartilage, and ligamentum teres (Fig. 10a). The interpretation and correlation of intraoperative findings with the clinical examination and imaging findings will confirm the layered diagnosis and enable the surgeon to follow the preoperative surgical plan. Afterwards, the interportal cut is performed, connecting the anterolateral with the mid-anterior portal. This capsular cut will improve the visualization and enable the surgeon to work on the acetabular rim and subspine area. It should be limited only to the area of labral injury because unnecessary capsular cutting beyond the two portals may lead to postoperative capsular instability, especially in the setting of static overload such as acetabular undercoverage, increased femoral or acetabular version, femoral valgus, and dynamic instability [43, 44].
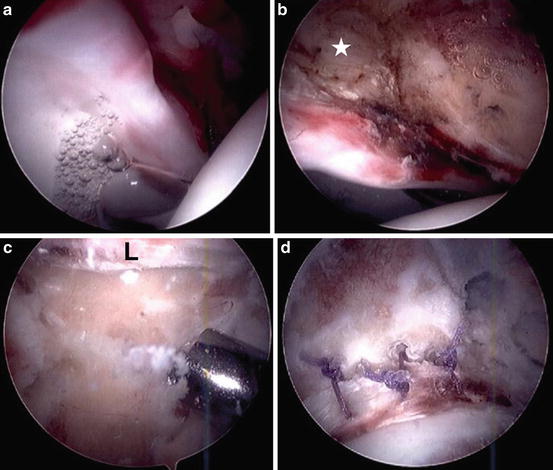
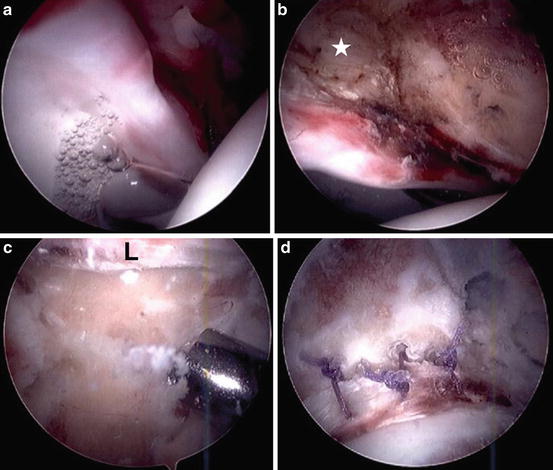
Fig. 10
a–d (a) View from the anterolateral portal in a right hip showing no discreet labral detachment, no cartilage wear on the femoral head, early grade 1 chondral delamination on transition zone cartilage from cam lesion, and anterior capsular inflammation. (b) View from the anterolateral portal demonstrating significant capsular-sided labral erythema, rectus inflammation, and distal extension of the AIIS (white asterisk) below the acetabular rim. (c) Subspine decompression with a 5.5 mm bur. View from the mid-anterior portal confirms that the resection of the acetabular rim distally to the AIIS extends all the way to the transition zone of the chondrolabral junction. (d) Arthroscopic view showing adequate subspine decompression, rim correction, and labral refixation. L labrum
Based on preoperative imaging and intraoperative visualization, the margins of the AIIS abnormality and associated capsular-sided labral damage are defined. Depending on the distal and anterior extension of the AIIS in relation to the acetabular rim, the degree of labral damage and capsular-sided erythema may vary in severity. The capsule is then elevated off in this area using both low-energy radiofrequency ablation and motorized shavers bur (extra-long 5.5-mm full radius), but care is taken not to primarily detach the labrum from the rim. A flexible radiofrequency probe may be helpful to dissect the capsule around the AIIS and in the area of acetabular rim if focal overcoverage coexists (Fig. 10b). After the capsule has been elevated, and the AIIS is fully exposed, subspine decompression can be performed utilizing motorized burs (5.5 mm in diameter) (Fig. 10c). Resection of the prominent AIIS can be confirmed both arthroscopically and under fluoroscopic imaging (Figs. 10d, 11). Over-resection proximally should be avoided in order not to endanger the insertion of the direct head of rectus femoris; if it is significantly destabilized, reattachment may be required although this complication has not been reported in the literature to date. If the prominence of the AIIS extends medially as well, decompression of the medial border should be performed especially if there are clinical, radiological, and intraoperative findings of symptomatic psoas impingement against the AIIS. The medial portion of the AIIS has been shown to be devoid of tendinous origin and a safe zone for decompression [30]. If the estimated time of traction will exceed 90 min due to significant work required in the central compartment (rim trimming, AIIS resection, labral repair), then the AIIS decompression can be performed or completed without traction to decrease the incidence of extended traction-related complications [45]. Potential disadvantage of this approach is that after completion of the AIIS decompression, labral attachment integrity should be reassessed. When the AIIS prominence extends straight distally to the rim level and therefore significant bone resection may be required, the labrum may need to be repaired at the completion of the decompression, which is not possible without traction. The subspine decompression is considered successful when the resection of the acetabular rim distally to the AIIS extends all the way to the transition zone of the chondrolabral junction minimizing, thus, the likelihood for residual postoperative rim-impaction impingement (Fig. 10c). However, intraoperative fluoroscopy should be used to confirm the extent of AIIS resection, especially distally (Fig. 11). Radiological and intraoperative recognition of the extent of the AIIS prominence relative to the acetabular rim both anteriorly and distally is of paramount importance. It has been shown that AIIS extending to or below the level of the anterior–superior acetabular rim may be partially or completely responsible for the appearance of a radiographic crossover sign in hips with anteverted acetabulum [46]. The use of fluoroscopic imaging may prevent unnecessary resection of acetabular hyaline cartilage and production of iatrogenic acetabular dysplasia. In the setting of normal acetabular version, preoperative crossover sign on a well-positioned AP view of the pelvis may be corrected after adequate isolated AIIS resection [46]. Extended subspine decompression combined with rim resection and damage to the transition zone cartilage may necessitate labral refixation. Destabilized labrum should be reattached to the rim with modern arthroscopic techniques (Fig. 10d). At this point, a third portal is established; the DALA portal is placed in line with the anterolateral portal, approximately 5 cm distally which will enable the positioning of the anchor/anchors along the acetabular rim and could be used as a working portal for the femoroplasty in the peripheral compartment later, if needed. Depending on the femoral torsion, the DALA portal may be placed slightly more anterior in retroverted femurs to reduce the possibility of instruments’ impaction against the anterior facet of the greater trochanter. Whether the labrum should be debrided or repaired, it is based on the size of the tear, the degree of detachment, and the quality of the labral tissue, aiming to preserve as much labral tissue possible and reestablish the normal seal effect of the labrum. Anatomic labral refixation can be accomplished with small diameter anchors. Labral eversion should be avoided, and depending on labral tissue quality, sutures should be placed either intra-substance or circumferentially around the labrum (Fig. 10d).