Study
No. of patients
Study design
Mean age
Mean follow-up
Scoring scales
Outcomes
Espinosa et al. [23]
60
Level III retrospective comparative
30 year
12 and 24 months
Merle d’Aubigné clinical score
Open repair had statistically significant better outcomes
Tönnis arthrosis classification
Larson et al. [24]
94
Level III retrospective comparative
30 year
40 months
Harris Hip Score (HHS), short form 12 (SF-12), and a visual analog scale (VAS)
Repair had statistically significant better outcomes
Krych et al. [28]
36
Level I RCT
39 year
36 months
Hip Outcomes Score (HOS)
Repair had statistically significant better outcomes
Philippon et al. [29]
122
Level II prospective cohort
40.6 year
27 months
Modified Harris Hip Score (mHHS)
Repair had statistically significant better outcomes with FAI
Labral Refixation Technique
Once adequate distraction has been obtained, the anterolateral portal is established approximately 1 centimeter (cm) anterior and proximal to the anterior aspect of the greater trochanter. A spinal needle is introduced into the hip under fluoroscopic guidance, and a guidewire is placed through the spinal needle. A 4.5 cannula passed over the guidewire into the hip joint between the labrum and the femoral head. The 70° arthroscope is inserted through the cannula, and the anterior hip triangle is visualized. An anterior portal is created about 1 cm inferior and 1 cm lateral from the intersection of the vertical line from the anterior superior iliac spine (ASIS) and the horizontal line from the tip of the greater trochanter under direct visualization. At this point, the anteromedial aspect of the labrum can be visualized, and a probe can be used to palpate potential areas of detachment as well as cartilage delamination. Switch the arthroscope into the anterior portal to visualize the anterolateral extent of the labrum. Using a long handle arthroscopic scalpel (Samurai, Pivot Medical Sunnyvale CA), incise the hip capsule 5–8 mm away from the labrum to connect the anterolateral and anterior portals. The arthroscope needs to be switched back to the anterolateral cannula to complete the interportal capsulotomy. The length of the capsulotomy may vary depending on the extent of pathology, but generally about 4 cm is required. Be sure to incise the entire width of the capsule to allow for instrument exchange and excursion.
The labrum is evaluated according to the Seldes criteria [4]. The size and location of the chondrolabral injury can be approximated with a probe. The tissue quality and the labral width are also considerations when deciding how to treat the labrum. Based on preoperative imaging as well as the labral evaluation, the area of pincer deformity that requires rim trimming can be determined (Fig. 1).


Fig. 1
Acetabular labral tear. An arthroscopic view of a right hip with a 70° scope in the anterolateral portal demonstrates a labral tear within the anterosuperior acetabular region with a wave sign of delaminated cartilage
A small shaver is introduced through the anterior portal, and the capsular tissue adjacent to the labrum is gently debrided. The shaver is positioned next to the capsular tissue, and the suction will allow the capsular tissue to be selectively debrided avoiding iatrogenic labral damage. It is critical to avoid injury to the superficial layer of the labrum to maintain the integrity of the labrum. A radiofrequency device (HipVac, ArthroCare, Austin, TX) is then introduced into the joint to ablate the remaining capsular tissue from the acetabular rim and the meticulously peel back the labrum from the acetabulum. Through the anterior portal, a 5.5 mm arthroscopic spherical burr is used to resect the anteromedial aspect of the pincer deformity (Fig. 2). Next, the arthroscopic burr is placed through the anterolateral portal to access the anterolateral aspect of the pincer deformity. If there are areas of anteroinferior iliac spine (AIIS) impingement, subspine decompression can be performed prior to labral refixation. The authors prefer to avoid labral takedown in most cases to preserve the chondrolabral transition zone in order to maintain the biologic interface and to facilitate more anatomic labral refixation and restoration of suction seal. In some cases, a formal labral takedown may be necessary in cases of global acetabular overcoverage. The fluoroscopic imaging can also be used to confirm the extent of bony rim resection.


Fig. 2
Acetabular rim preparation. An arthroscopic view of a right hip with a 70° scope in the anterior portal with the arthroscopic burr through the anterolateral portal
Anchor placement can begin after the adequate osseous and soft tissue preparation. With the arthroscope in the anterior portal, 8 × 110 mm clear plastic cannula (Smith & Nephew, Andover, MA) is placed over a Wissinger rod in the anterolateral portal to refix the anterolateral labrum between 10 o’clock and 1 o’clock for a right hip. The drill guide is positioned through the cannula on the acetabulum as close to the articular cartilage surface as possible without penetration at the 11–12 o’clock position. The authors recommend using as small a suture anchor as possible to allow for accurate placement of anchors. While the assistant is drilling, the drill tip can be sounded to prevent violation of the subchondral plate. Meanwhile, the arthroscope is placed into the joint to view the cartilage surface to ensure that the drill is not between the subchondral bone and cartilage surface. Once the suture anchor (1.4 mm Nanotack, Pivot Medical, Sunnyvale, CA) is malleted into place, the sutures can be passed through the labrum. Anchor pull-out strength is always gently checked to confirm anchor seating. If the labrum size and tissue quality are normal, then mattress stitches are preferred with the first pass using a tissue-penetrating device (Nanopass, Pivot Medical, Sunnyvale, CA) at the chondrolabral junction, and the suture is retrieved through the widest aspect of the labrum. If the labrum is either hypoplastic or the tissue appears degenerative, then a simple loop is passed around the labrum. Next, the sutures are tied using reverse half hitches and alternating posts. Another anchor can be placed from this portal at the 12–1 o’clock location.
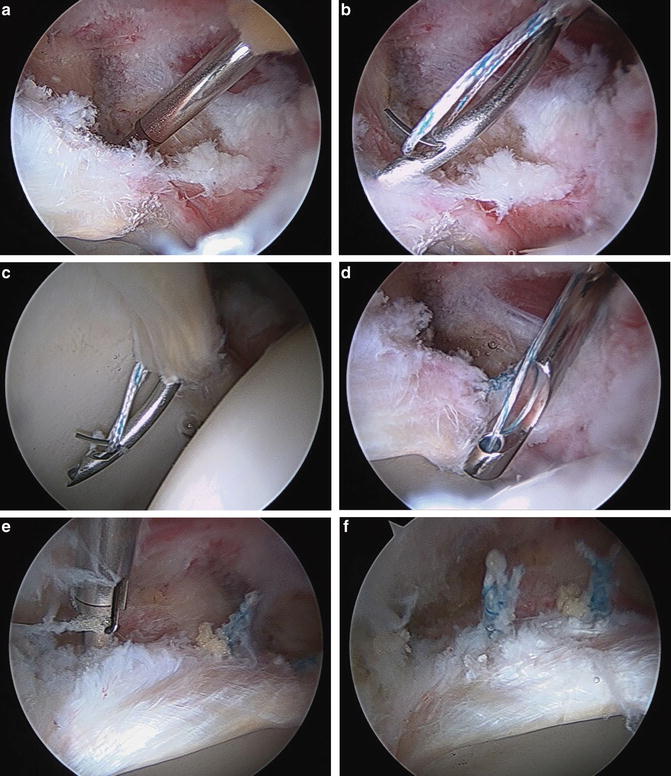
To access the anteromedial acetabulum, the arthroscope is placed in the anterolateral portal, and the clear plastic cannula is placed in the anterior portal. A percutaneous distal accessory anterolateral (DALA) portal is placed 4 cm distal and in line with the anterolateral portal. A drill guide is passed over a guidewire and placed on the acetabular rim (Fig. 3a). The drill is advanced using the same techniques previously described with a trajectory parallel to the floor. Once drilling begins, the cartilage within the joint is viewed ensuring there is no cartilage breaching with the drill. The anchor is inserted through the guide and gently malleted within the bone. Through the anterior cannula, the tissue penetrator is used to retrieve the suture closest to the labrum, and the labrum is pierced at the chondrolabral junction (Fig. 3b). The penetrator is passed into the joint and releases the suture. If performing a mattress configuration, the labrum is pierced in the widest aspect of the labrum with the penetrator (Fig. 3c). If performing a simple loop stitch, the penetrator is passed into the joint, and the sutures are then retrieved through the labrum and out of the cannula. Using the other suture as the post, a series of reverse half hitches and alternating posts are used to tie the knot (Fig. 3d–f). Labral refixation is completed when the labrum is firmly reattached to the acetabulum, and the suction seal of the joint is reestablished (Fig. 4). If a femoral osteoplasty is to be performed, the traction is taken off and the joint reduced. At the completion of the surgery, a dynamic assessment of the hip range of motion and the labral seal is confirmed.