Total Knee Replacement: Valgus Release
The valgus arthritic knee presents as a complex deformity characterized by bone loss involving the lateral femoral condyle, contractures of the lateral soft tissue structures, and concomitant instability.
Patient Presentation and Symptoms
Patients with end-stage degenerative joint disease (DJD) and valgus knee deformity present with pain, limitation of activities of daily living, increasing angular deformity, and increasing instability.
Indications
Total knee replacement (TKR) with valgus release is indicated when nonoperative treatment modalities for end-stage DJD, both mechanical and pharmacological, have failed to relieve pain.
Contraindications
The major contraindication for TKR is infection, whereas relative contraindications include young age, high activity level, and obesity.
Physical Examination
The following steps should be followed as part of the
standard physical examination for end-stage DJD:
- Assess patient gait.
- Establish presence of deformity (valgus/varus, flexion contracture, extension contracture).
- Measure range of motion.
- Evaluate status of extensor mechanism and patellofemoral articulation.
- Assess stability [integrity of medial collateral ligament (MCL)].
- Perform neurovascular exam.
Diagnostic Tests
Standard anteroposterior (AP), lateral, Merchant, and alignment radiographs should be included in the diagnostic protocol for TKR candidates. Fluoroscopic examination may be
utilized to determine the degree of medial instability. A baseline electromyogram (EMG) should be performed on patients presenting with symptoms that may be attributed to lumbar sacral spinal disease, such as hypoesthesia, dysesthesia, and paresthesia.
Special Considerations
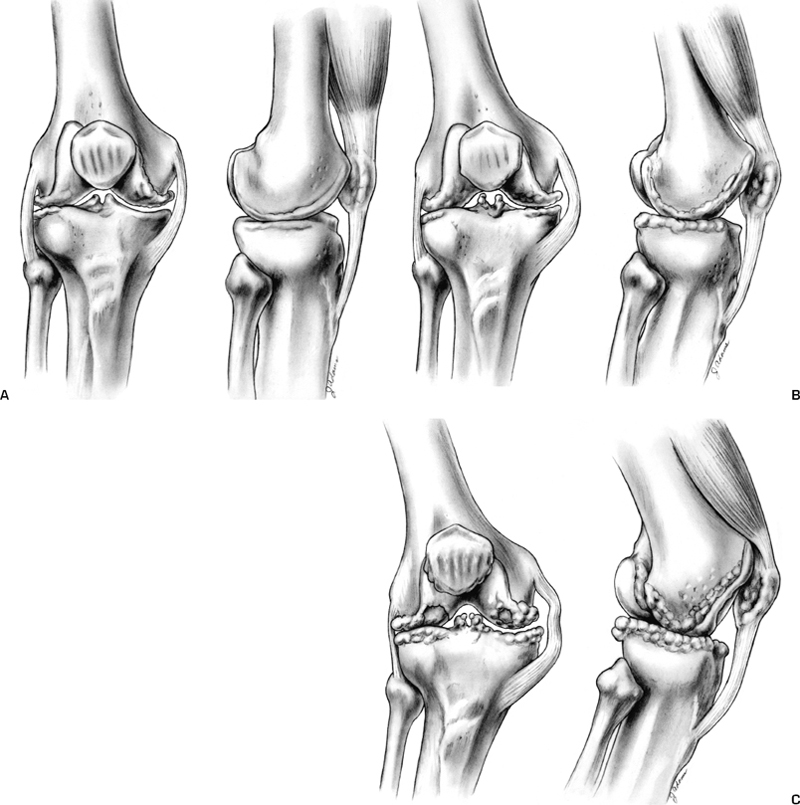
From a surgical perspective, valgus deformities may be classified into three major variants (I, II, III) based on the degree of deformity, the MCL status, and the amount of release that must be performed (Fig. 36–1). Variant I cases, accounting for 80% of all valgus deformities, occur secondary to bone loss in the lateral compartment. This variant is characterized by mild lateral femoral condylar and tibial plateau deficiencies, with slight soft tissue sleeve asymmetry (Fig. 36–1A). These patients correct to neutral alignment with varus stress. In variant II cases the medial soft tissues are also intact; however, the degree of deformity, bone loss, and soft tissue asymmetry are greater (Fig. 36–1B). These cases account for 15% of all valgus deformities and do not correct to neutral alignment with varus stress. Variant III deformities, distinguished by attenuation of the medial capsular ligament complex, marked lateral soft tissue contracture, and marked bony deficiency of both the lateral femoral condyle and the lateral tibial plateau, account for 5% of all valgus deformities (Fig. 36–1C).
Preoperative Planning and Timing of Surgery
Preoperative planning and discussion with the patient are the standard routines for TKR cases. The physician must advise the patient with valgus deformity of the potential for peroneal palsy. Surgical management is based on variant assignment. For variant I, the MCL is intact and minimal release is required; a posterior cruciate retaining (PCR) or posterior stabilized (PS) device may be used. In variant II, where a more generous concave release is necessary, the resultant joint line alteration may require the use of a PS device. In the case of an attenuated medial collateral ligament (variant III), concave release must be done to reestablish the mechanical axis and a posterior stabilized constrained (PSC) device should be used. Alternatively, some authors advocate MCL reconstruction.1 Radiographs are analyzed to determine appropriate angles of femoral/tibial resection and the need to augment bony deficiencies.
Special Instruments
A single set of instruments that allows for complete interchangeability between the three basic TKR prostheses types (PCR, PS, and PSC) is preferred.
Anesthesia
General anesthesia or epidural anesthesia with intravenous (IV) sedation (author’s preference) may be employed during TKR.
Patient Position
Surgery is performed with the patient in the supine position.
Surgical Procedure
Medial parapatellar arthrotomy is the most common surgical approach for TKR and is preferred by the author.
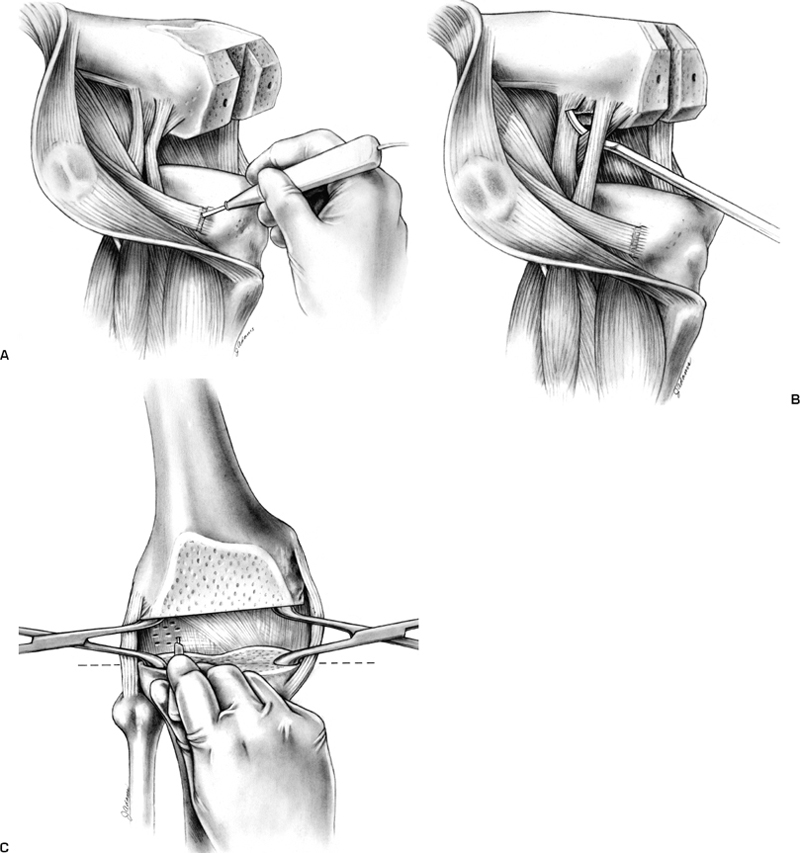
Because valgus deformity frequently requires lateral retinacular release, however, some authors recommend a lateral parapatellar arthrotomy.2 Using the intact medial femoral condyle and tibial plateau as a reference, bony resections are made. The following steps are then performed in sequential order, with restoration of the mechanical axis and stability analyzed after each release (Fig. 36–2). First, the peripheral osteophytes are removed. Next, contracture of the iliotibial band (ITB) is noted with the knee in full extension. Release may be performed using one of the following techniques:
- Release from Gerdy’s tubercle2 (author’s preferred method, Fig. 36–2A)
- Fractional lengthening with multiple stab wounds2,3
- Transection at the joint line.
The posterior lateral capsule/arcuate complex is then released from the distal femur by one of two methods:
- With the knee in flexion, using a curved osteotome (Fig. 36–2B)
- With the knee in full extension, by fractional lengthening via multiple stab punctures (Fig. 36–2C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








