Total Knee Replacement: Periprosthetic Patella Fractures
Etiology
Patella fractures following resurfacing in total knee arthroplasty have a reported incidence from 0.3 to 21%.1,2 Causative patient-related factors include the presence of osteoporosis, rheumatoid arthritis, male gender, high level of postoperative activity, and excessive postoperative flexion.3 Implant factors that have been reported to increase the risk of postoperative fracture include the presence of a large central patellar component peg, metal backed and inset patellar designs, and posterior cruciate ligament substituting implants.3,4 Technical factors include excessive (< 12 mm remaining thickness) or inadequate patellar resection, anterior patellar perforation, patellar malalignment leading to maltracking or dislocation,5,6 and diminished patellar vascularity following lateral release.3,7–10 Patella fractures following total knee arthroplasty without patellar resurfacing are reported to occur less frequently (0.05 to 6.3%) and are generally treated as patella fractures in a native knee.
Classification
Postoperative periprosthetic patellar fractures are classified by etiology as either traumatic or fatigue.11 Traumatic fractures occur either as the result of direct impact or indirectly as the result of a violent quadriceps contracture. Stress fractures are often located peripherally (laterally based) and, in general, do not interfere with patellar component fixation or extensor mechanism integrity. Stress fractures are often asymptomatic.
Treatment
Treatment options include nonoperative modalities with or without immobilization, open reduction and internal fixation (ORIF), fragment excision, component removal or revision, and patellectomy. The clinical factors that dictate appropriate treatment include the status of the extensor mechanism and the patellar component (Table 48–1).12,13 Patients with an intact extensor mechanism and no evidence of patellar component loosening can be treated nonoperatively.14 A disrupted extensor mechanism or patellar component loosening is generally an indication for operative treatment.11 Rarely, with a history of patellar instability and a recent fracture-dislocation, total knee revision is required to treat the underlying patellofemoral malalignment in addition to the fracture. In these cases femoral or tibial component malrotation is usually the underlying etiology.
Patient Presentation and Symptoms
- Traumatic mechanism:
- Pain
- Swelling
- Possible extensor lag
- Pain
- Stress fracture:
- Asymptomatic versus painful
- Rarely extensor lag
- Asymptomatic versus painful
Indications
- Disrupted extensor mechanism
- Loose patellar component
- Open fracture
Contraindications
- Intact extensor mechanism
- Well-fixed patellar component
Physical Examination
- Inspect the skin.
- Identify any localized tenderness.
- Occasionally a palpable defect in the extensor mechanism can be present.
- A hemarthrosis is often present in a traumatic fracture.
- Examine extensor mechanism integrity (straight leg raise and extensor lag).
- Occasionally these fractures can be asymptomatic (chronic or stress fractures).
| Patellar Component Loose | Patellar Component Stable | |
| Intact extensor mechanism | Nonoperative | Revise or remove component ± ORIF Consider nonoperative treatment if poor soft tissue status or medically complicated patient |
| Disrupted extensor mechanism | ORIF to reconstitute extensor mechanism | ORIF to reconstitute extensor mechanism |
| Fragment excision with extensor mechanism repair | Revise or remove component with extensor mechanism repair Fragment excision with extensor mechanism repair Patellectomy with extensor mechanism repair |
Diagnostic Tests
Anteroposterior (AP), lateral, and Merchant view of knee
Special Considerations
Prefracture knee function and ambulatory status
Preoperative Planning and Timing of Surgery
- Have revision components available for unexpected findings.
- Consider tibial polyethylene exchange if radiographic or gross evidence of wear.
- Internal fixation devises
- Stainless steel wire (18 or 16 gauge)
- Kirschner wires (K-wires)
- Cannulated screw sets
- Stainless steel wire (18 or 16 gauge)
- Timing:
- Within the first 10 to 14 days as soft tissues allow for safe exposure (i.e., no blisters, abrasions, extensive ecchymosis)
- Within 6 to 8 hours if open (rare)
- Within the first 10 to 14 days as soft tissues allow for safe exposure (i.e., no blisters, abrasions, extensive ecchymosis)
Anesthesia
Regional anesthesia if possible (spinal/epidural), or general anesthesia if regional contraindicated
Patient Position
Standard total knee arthroplasty (TKA) supine positioning
Surgical Procedure
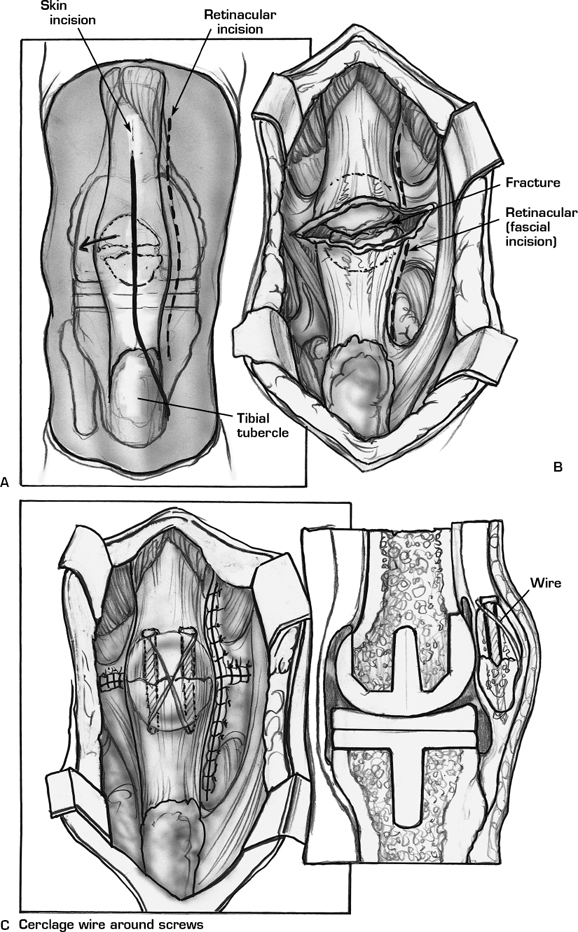
Surgical Approach
- Use previous TKA incision (the most appropriate lateral incision if it can be chosen)
- Medial parapatellar arthrotomy
Open Reduction and Internal Fixation (ORIF)
- Determine status of patellar component.
- Well fixed and well supported (> 60% supported): keep
- Well fixed but poorly supported (< 60% supported): remove
- Loose: remove
- Well fixed and well supported (> 60% supported): keep
- If more than two fragments are present, fix longitudinal fragments first to convert the construct to a two-piece transverse fracture if possible.
- Fix transverse fracture with 4.5 or 5.0 cannulated lag screws (Fig. 48-1).
- Reinforce with tension band wires placed through cannulated screws (Fig. 48-1).
- Use K-wires if unable to place screws secondary to retained component.
- A cerclage wire around the periphery of the patella can supplement fixation if needed.
Partial Patellectomy (Fragment Excision) (Fig. 48-2)
- Determine status of patellar component as above.
- Excise distal fragment preserving soft tissues.
- Suture patellar tendon with No. 5 braided, nonabsorbable suture using two Krackow-type stitches placed on the medial and lateral halves of the tendon.e
- Pass tails through three drill holes (two limbs in central hole) drilled to exit distal fracture surface adjacent to articular surface (posterior).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








