Total Knee Replacement: Pearls of Posterior Cruciate Ligament Substitution
Patient Presentation and Symptoms
- Chronic knee pain
- Stiffness
- Recurrent swelling
Indications
- Chronic pain secondary to osteoarthritis, inflammatory arthritis, posttraumatic arthritis, and avascular necrosis
- Restricted motion and loss of function
- Failure to respond to nonsurgical management
Contraindications
- Active infection (absolute)
- Genu recurvatum with muscular weakness (relative)
- Stable arthrodesis (relative)
- Extensor mechanism disruption (relative)
Physical Examination
- Joint line tenderness
- Limited range of motion
- Varus or valgus deformity
- Flexion contracture
- Effusion
Diagnostic Tests
- Standard radiographs: weight bearing anteroposterior (AP) and 45-degree flexion posteroanterior (PA) views, Merchant, and lateral views
- Full-length AP, three-joint view
Special Considerations
History of remote infection of the ipsilateral knee should be excluded. Prior surgical incisions about the intended operative site should be evaluated and the date of previous procedures determined. The ipsilateral extremity should be carefully examined to determine neurologic or vascular deficits, and to exclude referred pain from the lumbosacral spine or hip.
Preoperative Planning and Timing of Surgery
- Evaluation of the mechanical axis of the ipsilateral limb and degree of deformity from the three-joint view radiograph
- Determination of the angle between the mechanical and anatomic axes of the ipsilateral femur for determining valgus angle of distal femoral resection.
- Preoperative medical management to optimize chronic medical conditions
Special Instruments
- Modular, posterior stabilized prosthesis system with multiple sizes of femoral and tibial components allowing matching of native sizes within a few millimeters
- Independent sizing of the femoral and tibial components
- Intramedullary alignment guide for distal femoral resection
- Posterior referencing femoral sizing guide
- Extramedullary alignment guide for tibial resection
- Spacer blocks for determining flexion and extension gap symmetry
- Caliper for determining patellar thickness
- Patellar reamer to allow accurate resection and creation of flat patellar surface
Anesthesia
Options are epidural anesthesia with intravenous (IV) sedation as needed and postoperative epidural patient-controlled analgesia (PCA), or general anesthesia with postoperative IV PCA.
Patient Position
Supine on regular operating room table
Surgical Procedure
- Anterior, midline skin incision beginning ~6 cm proximal to the superior pole of the patella and extending the same distance distal to the inferior pole
- Distal incision should run just medial to the medial edge of the tibial tubercle rather than over the prominence.
- Medial arthrotomy, beginning at apex of quadriceps tendon running distally, leaving ~0.5 cm cuff of tendon on the medial border. Arthrotomy is continued over the medial border of the patella and extends distally just medial to the border of the patella tendon
- Quadriceps snip if unable to evert the patella, beginning at the apex of the quadriceps tendon and extending proximally and laterally into the vastus lateralis at an angle of 45 degrees
Dressings, Braces, Splints, and Casts
- Postoperative drain placed intraarticularly prior to arthrotomy closure. The drain should be removed on the morning of postoperative day 1.
- Nonadherent gauze, covered with a dry gauze and light cotton roll, held in place by a compression stocking, allows for immediate range of motion.
Tips and Pearls
- Release of the contracted structures to restore equal soft tissue tension. The release in the valgus knee is performed after the basic bone cuts to facilitate exposure.
- Five-degree distal femoral valgus resection in valgus knees and 7 degrees in varus knees.
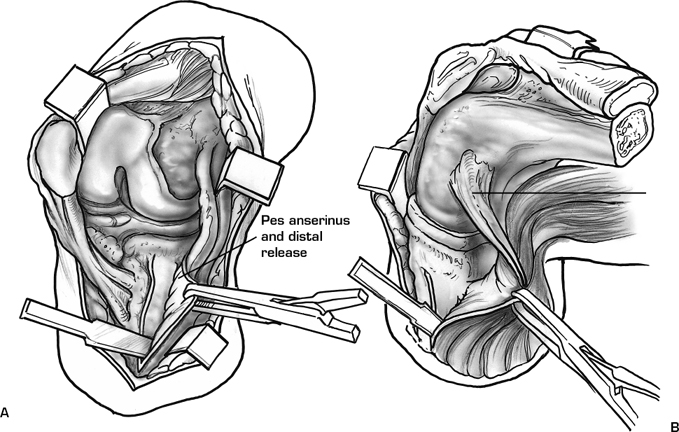
- In the varus knee, subperiosteal medial soft tissue elevation including the medial capsule, deep medial collateral ligament (MCL), distal insertion of the superficial MCL, and semimembranosus insertion should be performed (Fig. 39–1).
- Distal femoral resection equal in thickness to prosthesis.
- Identification of the prominence of the lateral epicondyle (origin of the lateral collateral ligament) and the center of the sulcus of the medial epicondyle (origin of the deep medial collateral ligament (Fig. 39–2).
- Determination of the epicondylar axis drawn between the two points identified in item 3 (Fig. 39–3).
- Placement of the femoral component parallel to the epicondylar axis regardless of specific instrumentation system used (Fig. 39–4).
- Posterior referencing instruments to select the femoral component that most closely duplicates the size of the native femur in the AP dimension.
- Posterior medial condylar resection equal to thickness of prosthesis.
- Tibial resection perpendicular to the mechanical axis with 10 mm of bone resected from the unaffected condyle (Fig. 39–5).
- Complete resection of the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL).
- In the valgus knee, the popliteus tendon is preserved. With distraction from a laminar spreader with the knee in extension, a graduated release is performed. First, a transverse incision is made through the posterolateral capsule, lateral to the popliteus tendon, at the level of the tibial bone cut. Next, multiple transverse “piecrust” stab incisions are performed through the lateral capsule, iliotibial band, and lateral collateral ligament (LCL) until equal medial and lateral tension is created.
- Posterior capsular subperiosteal elevation, and posterior condyle osteophyte resection are performed to eliminate flexion contractures, and to prevent impingement in high flexion.
- Use of spacers to evaluate size of the flexion and extension spaces and symmetry of medial and lateral soft tissue tension (Fig. 39–6).
- Selection of the tibial component that covers the tibia without overhang (small posterolateral overhang is tolerated and results from correct rotational alignment when using a symmetric tibial tray).
- Tibial rotation set over the medial one-third of the tibial tubercle.
- Creation of composite resurfaced patellar that is 1 to 2 mm thinner than native patella helps tracking
- Use of reamer to create flat patellar surface of desired thickness
- “No thumbs” test of patellar tracking; lateral patellar release with attempt to preserve the superior lateral genicular artery if there is any tendency to tilt or subluxation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








