4.2 The musculoskeletal system
Chapter 4.2a The physiology of the musculoskeletal system
The physiology of the bony skeleton
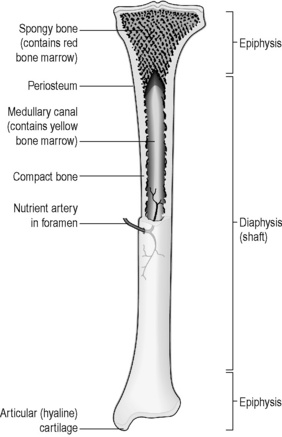
Long bones
The long bones (Figure 4.2a-I) in the body are the radius, ulna and humerus of the arm and the femur, tibia and fibula of the leg. They are characterised by a shaft and two widened ends known as ‘epiphyses’. The shaft is composed of dense, strong compact bone, with a central hollow that is filled with fatty yellow bone marrow. The epiphyses are the site of bone growth in the child, and are largely composed of soft, spongy cancellous bone containing bloody red marrow, all bounded by a rim of strong compact bone. The epiphyses are covered with hyaline cartilage in the regions where they make joints with other bones; elsewhere the long bones are bounded by a fibrous coat called the ‘periosteum’. Underneath the periosteum lie clusters of osteblasts and osteoclasts, the bone-forming cells that are responsible for bone remodelling and production. These cells are stimulated to form and reshape new bone when the periosteum or underlying bone becomes damaged. The design of the long bones confers strength, which is necessary for their main functions of locomotion, posture and manipulation.
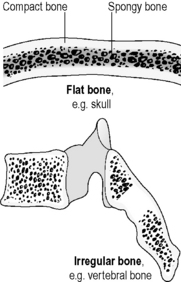
Short, irregular, flat and sesamoid bones
The short bones are less strong than the long bones because they are composed largely of spongy, cancellous, red, marrow-containing bone, and are bounded by a relatively thin protective rim of compact bone. This structure (Figure 4.2a-II) supports their functions of intricate movements (in the back, hands and feet), protection (skull bones, pelvis and ribs) and bone marrow production (see Q4.2a-2) .
.
The growth of bone in childhood and adolescence
The bones do not fully ossify until early adulthood. Until then, there are still some areas of cartilage or membrane that are actively forming new bone and allowing for growth. Because of this, the approximate age of a child can be estimated from an X-ray image of the bones, which shows the state of progression of ossification of the bones. Puberty is a time during which the surge of sex hormones causes an initial spurt of growth of long bones followed by ossification of the growth centres in the long bones (see Chapter 5.2a). This is why growth slows considerably once puberty has been reached.
The continued growth of bones
Vitamin D is an essential factor in the maintenance of the non-living (calcified) part of bone. In vitamin D deficiency the bones become softened. This leads to bowing of the bones during childhood (rickets) and pain and weakness in adulthood (osteomalacia). These conditions are discussed in more detail in Chapter 4.2d.
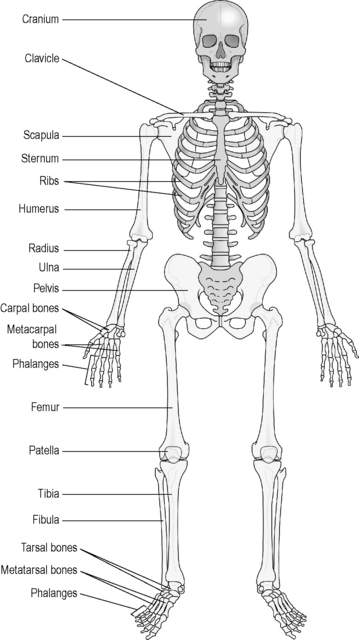
The structure of the skeleton
The skeleton can be considered as consisting of two parts: the axial skeleton and the appendicular skeleton. The axial skeleton (shaded bones in Figure 4.2a-III) forms the central bony core of the body, and consists of the skull, vertebral bones, sacrum, coccyx, ribs and sternum. All these bones are either flat or irregular, and so each is composed of a core of red-marrow-containing cancellous bone surrounded by a thin rim of compact bone. The skull and the vertebral column support and protect the fragile structure of the brain and spinal cord. The ribs and sternum likewise support and protect the lungs and the heart in the thorax, and the organs of the upper abdomen, including the liver, kidneys, pancreas and the spleen.
The appendicular skeleton (unshaded bones in Figure 4.2a-III) is so called because it consists of the appendages to the axial skeleton. These are the shoulder girdle (clavicles and shoulder blades), the upper limbs, the pelvic girdle (the hip bones) and the lower limbs. The bones of the shoulder girdle and the pelvic girdle are flat bones. The bones of the limbs are either long bones or irregular bones.
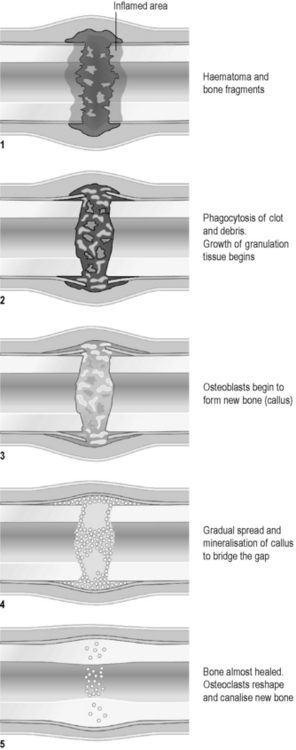
The healing of bones
The healing of broken bones can be compared to the healing of wounds in that it is the formation of a blood clot in the space between the broken ends that initiates the healing process. Figure 4.2a-IV illustrates the stages in the healing of the broken shaft of a long bone. The blood clot stimulates the inward movement of phagocytes and osteoblasts. The phagocytes remove unwanted debris, while the osteoblasts lay down an initially chaotic mass of new bone called ‘callus’. The callus is gradually remodelled by osteoclasts into new, ordered compact bone. In adults this process takes weeks to months, but it is significantly quicker in children (see Q4.2a-3 and Q4.2a-4) .
.
The physiology of the joints
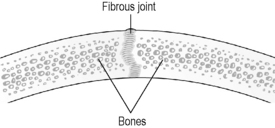
Fibrous joints involve two edges of bone that are linked by tough strands of fibrous connective tissue. The suture lines of the skull are an example of fibrous joints (Figure 4.2a-V). The movement at a fibrous joint is limited.
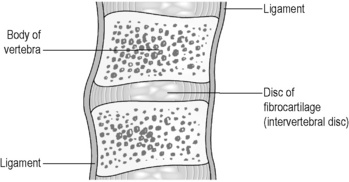
Cartilaginous joints offer the potential for more movement because the bones in these joints are linked by a pad of fibrocartilage, which has more spring and bulk than the fibrous strands of a fibrous joint. In the pubis symphysis and in between the vertebral bodies this fibrocartilage pad has a shock-absorbing function (Figure 4.2a-VI).
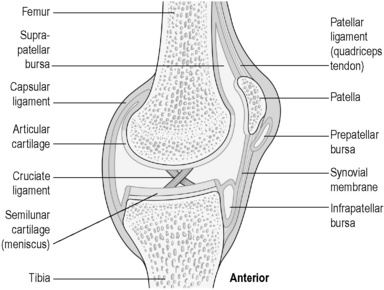
Synovial joints offer the most movement and have the most complex structure (Figure 4.2a-VII). The internal surface of the bones in synovial joints is lined with glassy smooth hyaline articular cartilage, and the rest of the joint space is bound by a fibrous joint capsule (the capsular ligament). The internal surface of the joint is lined with a fluid-secreting synovial membrane. The term ‘synovial’ has its root in the Greek word ‘ovum’ meaning egg. This is because the lubricating fluid contained within these joints has been likened in consistency to the white of an egg. The whole joint is given stability by means of fibrous bands (the ligaments) that link the bones and also by the muscle insertions (the tendons), which cross the joint to insert close to its margins.
Some of the synovial joints have unique additional features, for example the knee joint illustrated in Figure 4.2a-VII contains thickened C-shaped cartilage pads, which sit on the tibial plateau, and two cruciate (crossing) ligaments, which run through the joint space to provide anterior to posterior stability.
The physiology of the skeletal muscles
The muscle fibres contract in unison in response to motor nerve impulses (see Chapter 4.1a). Each muscle fibre receives electrical impulses from a nerve fibre via a specialised synapse called the ‘motor end plate’. At this synapse, the electrical impulse travelling down the nerve fibre leads to the release of a neurotransmitter chemical. This chemical stimulates the changes within the muscle fibre that culminate in a temporary contraction. The contraction is sustained only for as long as the nerve continues to stimulate the motor end plate.
Most skeletal muscles never attain a state of full relaxation. There is always a low level of nervous stimulation to the muscles, which gives them a firmness known as ‘tone’. This background level of tone is essential for correct posture. It is generated as a result of reflex nervous activity at the level of the spinal cord, and is modified further by nervous impulses originating from higher control centres in the brain (see Chapter 4.1a). If the nerve supply to a muscle is cut off, the muscle becomes completely flaccid, and loses the springy quality that is the normal state in good health.
 Self-test 4.2a The physiology of the musculoskeletal system
Self-test 4.2a The physiology of the musculoskeletal system
1. Why do you think it is that long bones are mostly made of compact bone, whereas the other types of bone are mostly composed of cancellous bone?
2. How is synovial fluid made? What is its purpose?
Answers
1. The long bones need to be strong because they have to withstand recurrent stress from lifting and weight bearing. Compact bone is a tissue that provides strength in the direction required. Strength is less important in the other bones. In the other bones (irregular, flat and sesamoid), cancellous bone minimises the weight of the bone and provides a site for the manufacture of the blood cells.
2. Synovial fluid is made by the cells of the synovial lining that covers the ends of the bones and the lining of the capsular ligament on the inside of the joint space. The fluid provides lubrication for the joint, contains immune cells, and also allows the passage of nutrients to the cartilage that covers the bony ends within the joint.
3. The muscles of the body are never in a state of full relaxation, even in sleep, because there is always a ‘background’ level of nervous stimulation of the muscles, which gives each muscle its tone. Without tone the muscles would become flaccid.
Chapter 4.2b The investigation of the musculoskeletal system
Introduction
An investigation of the musculoskeletal system might involve:
• a thorough physical examination
• investigations to examine the structure of the bones, muscles and joints (X-ray imaging, ultrasound imaging, magnetic resonance imaging (MRI) and bone scans)
• examination of the blood to look for disturbances in the hormones and chemicals that reflect bone disorders and autoimmune diseases
• examination of the synovial fluid of a joint
• arthroscopy, the endoscopic examination of the interior of a joint.
Physical examination
The physical examination of the musculoskeletal system involves the stages listed in Table 4.2b-I.
Table 4.2b-I The stages in the physical examination of the musculoskeletal system
Examination of the synovial fluid of a joint
There is a small risk of introducing infection into the joint with this procedure.
Arthroscopy
 Self-test 4.2b The investigation of the musculoskeletal system
Self-test 4.2b The investigation of the musculoskeletal system
1. A 35-year-old female patient is referred to a rheumatologist because she has developed a painful condition of the joints in which a number of the joints (wrists, elbows, hips and knees) are swollen and warm. One knee in particular is very swollen with fluid. The patient is unwell and slightly feverish, and the joints feel very stiff in the mornings. The GP suspects rheumatoid arthritis. What investigations do you think this patient might have to undergo?
2. Faith is 55 years old. She has pain in the centre of her back. The GP suspects osteoporosis and is considering prescribing treatment to help prevent fractures. What investigations do you think the GP might perform?
Answers
1. The patient will be given a thorough physical examination in which the swollen joints are assessed and any joint deformities noted.
An arthroscopy would be unnecessary in this case.
2. Faith may undergo X-ray imaging of the painful part of her back. This might reveal the ‘thinning’ of the bones, which is characteristic of osteoporosis, and might also show if any of the vertebrae have become compressed as a result of the condition.
Examination of joint fluid and arthroscopy are not relevant to this case.
Chapter 4.2c The treatment of musculoskeletal pain
At the end of this chapter you will:
Estimated time for chapter: 60 minutes.
Analgesics in musculoskeletal disease
Simple analgesics
Paracetamol has few side-effects in low doses, but in overdose it is highly toxic to the liver.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Commonly prescribed NSAIDs include ibuprofen and diclofenac.
Opioid analgesics
Muscle relaxants
An important drug used to relax tense muscles in musculoskeletal conditions is diazepam. This drug is most commonly prescribed for its effect in calming anxiety in minor mental illness (see Section 6.2).
Corticosteroids
Non-drug methods of pain relief in musculoskeletal disease
Manipulation and massage
Anaesthetic and surgical approaches to pain relief
 Self-test 4.2c The treatment of musculoskeletal pain
Self-test 4.2c The treatment of musculoskeletal pain
1. A 60-year-old patient is taking three 200 mg tablets of ibuprofen a day for a constant pain in both hips. This pain has been diagnosed as early osteoarthritis. Because she gets slight indigestion if she takes any more tablets than this, her GP recommends that she also takes up to 4000 mg/day of paracetamol to relieve her pain. She finds she often needs to take all these tablets. Do you think that this approach to symptom relief is a reasonable one in conventional terms?
2. A 27-year-old gardener has suffered a sudden onset of back pain while digging. He is in so much pain that he is unable to drive himself home, and finds that his only relief is to lie flat on the floor. The GP examines him on a home visit and finds excessive muscle spasm in the lumbar area. Flexion of the hip joint induces pain on the left-hand side which radiates into the buttock and down the back of the leg (sciatica).
Answers
1. The GP has prescribed reasonably in conventional medicine terms. Ibuprofen is the best choice for arthritis, as long as the patient can tolerate its side-effects. In the short term, maximum-dose paracetamol is considered relatively safe, and may complement the action of the ibuprofen.
Chapter 4.2d The diseases of the bones
Introduction
This chapter is concerned with the important diseases that affect the bones. The diseases of the bone marrow have already been summarised in Chapter 3.4e. The conditions studied in this chapter are:
 .
.
 Information Box 4.2a-I
Information Box 4.2a-I .
.
 .
. Information Box 4.2a-II
Information Box 4.2a-II .
. Information Box 4.2a-III
Information Box 4.2a-III Information Box 4.2a-IV
Information Box 4.2a-IV Information Box 4.2c-I
Information Box 4.2c-I Information Box 4.2c-II
Information Box 4.2c-II Information Box 4.2c-III
Information Box 4.2c-III Information Box 4.2c-IV
Information Box 4.2c-IV Information Box 4.2c-V
Information Box 4.2c-V Information Box 4.2c-VI
Information Box 4.2c-VI Information Box 4.2c-IX
Information Box 4.2c-IX :
: Information Box 4.2d-I
Information Box 4.2d-I



