2.4 Infectious disease
Chapter 2.4a Principles of infectious disease
At the end of this chapter you will be able to:
Estimated time for chapter: 75 minutes.
Introduction to the study of infectious diseases
The infectious agents are summarised in Table 2.4a-I. They may be microscopic, in which case they are called ‘microbes’. If a microbe is a bacterium or a single-celled animal such as an amoeba, the term ‘microorganism’ may also be used, denoting that the microbe is a life form. Viruses are non-living microbes. Most infectious diseases are caused by microbes, but larger creatures such as worms can also cause infectious diseases. When the infectious agents are arthropods (insects and mites) the term ‘infestation’ may be used to describe the disease process.
Table 2.4a-I The different types of infectious agent
| Agent | Description |
|---|---|
| Microbes | |
| Viruses and prions | Non-living particles capable of replication; prions are made of protein alone, and viruses of a combination of protein and genetic material |
| Bacteria | The smallest life form; bacteria consist of single cells, but are more simple in structure than the generalised cell described In Chapter 1.1b |
| Fungi | Yeasts and moulds; like bacteria, these are composed of very simple cellular units |
| Protozoa | Single-celled animals such as the amoeba; the cells of protozoa contain all the organelles of the simple cell described in Chapter 1.1b |
| Larger organisms | |
| Roundworms, flukes and tapeworms | E.g. threadworm |
| Mites | E.g. head and body lice |
| Insects | E.g. fleas |
Immunity and infectious disease
The topic of immunity was introduced in Chapter 2.1d. The general level of immunity to a disease in a population is another major factor that affects the impact of the disease. Diseases that are very common in a population are termed ‘endemic’. Chickenpox and the common cold are diseases that are endemic in the UK, whereas malaria is endemic in a tropical country such as Uganda. It is common for a population in a locality which has been exposed from birth to an endemic disease to have less marked reactions to that disease than visitors to that locality. This is why travellers to foreign countries frequently succumb to infections that do not seem to affect the locals, leading to symptoms such as fevers and food poisoning.
The pathology of infectious disease
The infectious diseases can lead to damage that results from one or more of the seven processes of disease described in Chapter 2.2a. The flea bite is an example of how an infectious agent can give rise to inflammation, which is the most common disease process to result from infectious disease. However, infectious agents can also lead to disease by causing problems in the immune system, including cancerous change, and by causing degeneration.
Transmission of disease
There is an enormous number of possible routes of infection, illustrating the complex ways by which infectious agents have adapted themselves to find their way into their human hosts. Modes of transmission can be broadly considered in two categories: person-to-person spread and animal-to-person spread. Examples of these are listed in Table 2.4a-II.
Table 2.4a-II The different modes of transmission of infectious agents
Chapter 2.4b The different types of infectious disease
Infectious organisms
The main groups of infectious agents were introduced in the last chapter and summarised in Table 2.4a-I. Each one of these groups is in this chapter considered in turn, together with some of the diseases that they can cause.
Diseases caused by viruses
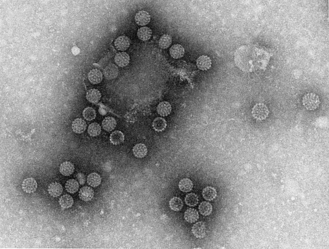
Viruses and prions are so small that, unlike bacteria and human cells, they cannot be seen using a simple microscope. Instead, a more powerful microscope, called an ‘electron microscope’, is required to produce images of these particles. Figures 2.4b-I and 2.4b-II show electron micrographs of two different viruses: the envelope-bounded DNA herpes simplex virus, and the icosohedral (20-sided) RNA rotavirus. The size of these viruses is measured in nanometres (nm), which are an unimaginable one-billionth of a metre (1 × 10−9 m) in size. These viruses are 160 and 80 nm in diameter, respectively.
 Self-test 2.4a Principles of infectious disease
Self-test 2.4a Principles of infectious disease
1. How might you define infectious disease?
2. Name the processes of disease that you think might result from an infection (and which then lead to the various symptoms of infectious diseases).
3. What do you think are possible reasons why infectious disease causes such problems in refugee camps? Think broadly about the health of the population in the camp, and how infections are transmitted.
4. From your own knowledge, what do you think are the modes of transmission for the following infections:
Answers
1. Infectious disease is disease resulting from damage by infectious agents. The infectious agent has been transmitted by contact with an infected carrier, which can be either animate or inanimate.
2. Infectious disease may cause damage to human tissue through the processes of inflammation, disturbance of the immune system, development of cancer or degeneration. Inflammation is the most important of these four processes in terms of impact on human health.
3. Infectious disease is a particular problem in refugee camps, mostly because sanitation is poor and diseases such as cholera and typhoid can spread via water contaminated with human faeces.
cells, and so cannot, by definition, be considered a life form. Viruses cause disease both because they damage living cells, and also because they trigger an immune response. The high temperature, rash, aches and malaise characteristic of many viral infections are manifestations of the immune response generated against viruses circulating in the blood stream.
• disturbance of cell replication, leading to benign growths (e.g. wart virus)
• cancer, as a result of interfering with the proto-oncogene function in a cell (e.g. genital wart virus, which can be a trigger for cervical cancer)
• disturbance of the development of the fetus, leading to congenital malformation (e.g. rubellavirus) if the infection occurs in pregnancy.
An excessive immune response to viruses can also be damaging. Possible consequences include:
• bleeding within tissues (e.g. the viral haemorrhagic disease Lassa fever)
• delayed immune damage to the nervous system, which can manifest as numbness, weakness and mood changes (e.g. Guillain–Barré syndrome).
Viruses are classified into groups (families and subfamilies) according to their structure. Some of the major families of viruses are listed in Table 2.4b-I, and some of the diverse diseases that result from viral infections are listed in Table 2.4b-II (see Q2.4b-1) .
.
Table 2.4b-I Some different families of virus
| Class of virus | Description |
|---|---|
| Adenoviruses | A large group of DNA-containing viruses that commonly cause minor upper respiratory infections |
| Herpesviruses | DNA viruses responsible for cold sores, chickenpox and glandular fever. All are capable of causing latent infections that can reappear at a later date |
| Poxviruses | DNA viruses causing crusting diseases such as smallpox, cowpox, monkey pox and orf |
| Picornaviruses | Small RNA viruses causing diseases including poliomyelitis, viral meningitis and the common cold |
| Reoviruses | Small RNA viruses responsible for epidemics of infectious diarrhoea and mild respiratory symptoms |
| Retroviruses | Viruses that are able to replicate by inserting a protein called ‘reverse transcriptase’ into a cell. Includes the human immunodeficiency virus (HIV) |
Table 2.4b-II Various viral diseases
| Disease | Causative virus |
|---|---|
| Pharyngitis (sore throat) | Adenovirus |
| Cold sores | Herpes simplex |
| Genital herpes | Herpes simplex |
| Chickenpox | Varicella zoster |
| Viral encephalitis | Measles, mumps, herpes simplex |
| Viral meningitis | Coxsackie virus, measles, mumps |
| Rabies | Rabies |
| Croup | Respiratory syncytial virus |
| Glandular fever | Epstein–Barr virus |
| Kaposi’s sarcoma | Epstein–Barr virus |
| Smallpox | Variola |
| Poliomyelitis | Poliovirus |
| Mumps | Mumps virus |
| Lassa fever | Lassa virus |
| Viral pneumonia | Measles, varicella zoster, |
| Diarrhoea | Rotavirus, noravirus, adenovirus |
| Rubella (German measles) | Rubella |
| Yellow fever | Yellow fever |
| Influenza | Influenza |
| Measles | Measles |
| Common cold | Rhinovirus |
Diseases caused by bacteria
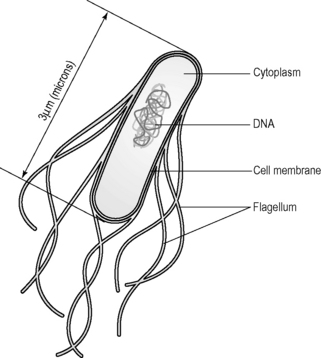
Bacteria (singular is bacterium) are microorganisms that consist of a single simple cell. The structure is far less complex than the typical animal cell described in Chapter 1.1b. Bacteria do not have nuclei or mitochondria, for example, but instead the copying of the genetic material and the energy-generating processes all take place around large molecules that are situated free within the cell cytoplasm. Nevertheless, the bacterium still uses basic nutrients and reproduces in a similar way. For this reason a bacterium is considered a life form. Bacteria are, on average, about one-tenth of the size of human cells, but can be seen through a simple microscope.
Figure 2.4b-III shows a simplified drawing of a rod-shaped bacterium, Escherichia coli (E. coli). The size of bacteria is generally measured in micrometres (μm), which are one-millionth of a metre (1 × 10−6 m) in size. An E. coli bacterium is 3 μm in length, which is 20 times longer than the diameter of the complex herpes simplex virus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 .
. .
. .
. . The newly emerging infectious diseases include hepatitis C and E viruses, Lyme disease, staphylococcal toxic shock syndrome, H5N1 avian influenza (bird flu), SARS (sudden adult respiratory distress syndrome) virus and nvCJD (new variant Creutzfeldt–Jakob disease) virus.
. The newly emerging infectious diseases include hepatitis C and E viruses, Lyme disease, staphylococcal toxic shock syndrome, H5N1 avian influenza (bird flu), SARS (sudden adult respiratory distress syndrome) virus and nvCJD (new variant Creutzfeldt–Jakob disease) virus.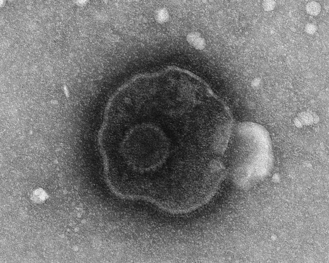
 .
. .
.