4.3 The urinary system
Chapter 4.3a The physiology of the urinary system
At the end of this chapter you will be able to:
Introduction
The component parts of the urinary system are illustrated in Figure 4.3a-I. It can be seen how the kidneys are situated in the upper part of the back of the abdomen. They rest protected against the ribs between the levels of T11 and L3. The influential acupoints on the back of the Kidney Organ (Shenshu Bl-23) lie directly over the lower parts of the kidneys. The ureters run from the medial aspect of each kidney, down the posterior border of the abdominal cavity, to open into the bladder. The bladder sits protected within the pelvis. Note from the diagram how small the bladder is. Even when uncomfortably full the bladder rarely rises very much higher than the level of the pubic symphysis (the region of acupoint Qugu Rn-2). The urethra (similarly spelled to the more proximal ureter, but a different anatomical structure) is the tube that links the bladder to the external world. It is very short in women, but longer in men because of its passage through the penis.
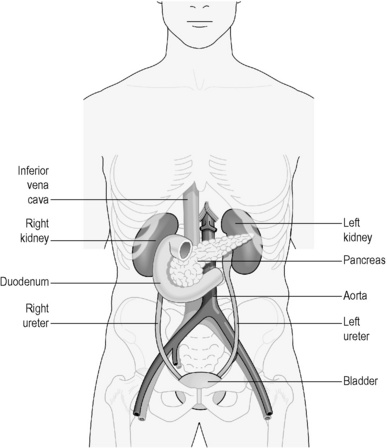
Figure 4.3a-I • The component parts of the urinary system (excluding the urethra) and related abdominal structures.
The physiology of the kidneys
The position and structure of the kidneys
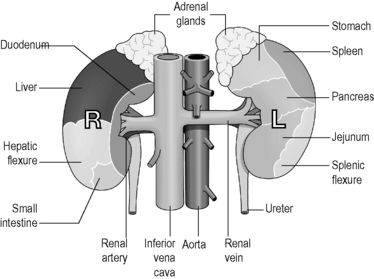
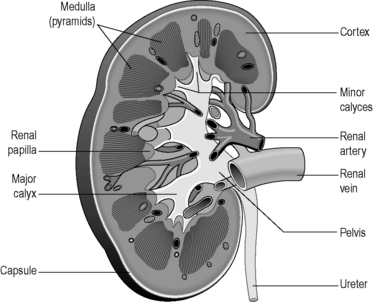
The tissue of the kidney consists of thousands of tiny tubes called ‘nephrons’. Each of these tubes has its origin in the outer parts of the substance of the kidney (the renal cortex). The nephrons converge to open out into wider tubes called ‘collecting tubules’, which drain into a space in the core of the kidney called the ‘renal pelvis’. The renal pelvis drains downwards into the ureter. The collecting tubules are situated in the deeper tissue of the kidney, which is known as the ‘renal medulla’. Figures 4.3a-II and 4.3a-III illustrate the external and internal structure of the kidneys in some detail. Figure 4.3a-II shows the position and size of the adrenal glands, and Figure 4.3a-III indicates the location of the renal cortex, medulla, pelvis and ureter.
The formation of urine in the kidneys
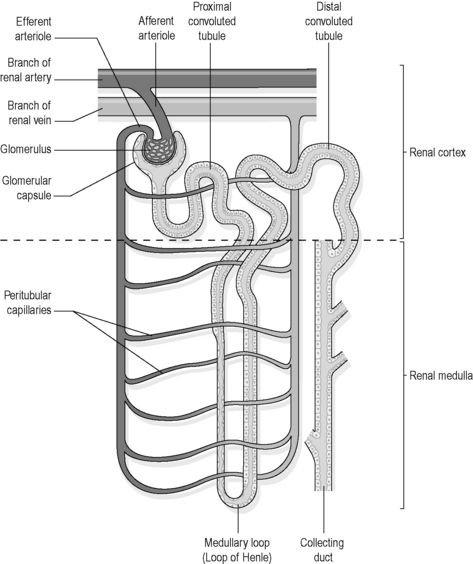
Figure 4.3a-IV shows how the blood that reaches the nephron first enters a cluster of capillaries called the ‘glomerulus’. Here, because of a sudden restriction of easy flow, fluid containing salts, wastes and water is forced out of the glomerulus. From here this fluid passes into the cup-like origin of the nephron. However, substances such as plasma proteins and blood cells are too large to be squeezed out, and so these remain within the blood vessel. This process of draining water and small molecules from the blood into the nephron is called ‘simple filtration’.
The physiology of the bladder
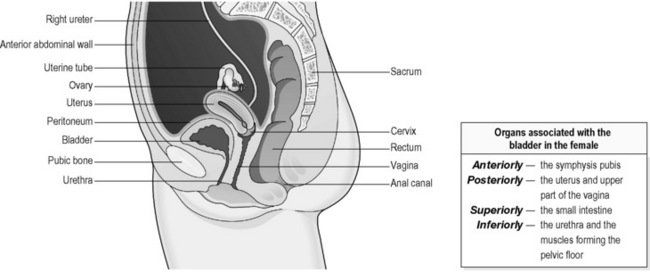
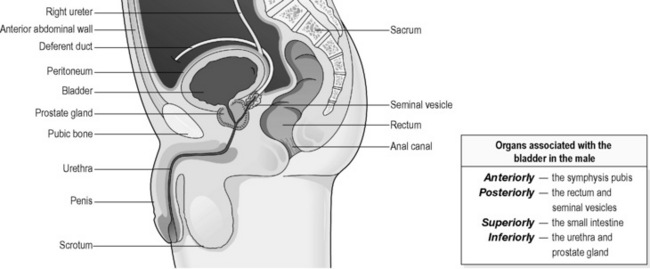
The bladder is a hollow, pear-shaped organ, the function of which is to act as a reservoir for urine. Figures 4.3a-V and 4.3a-VI show a vertical section through the pelvis of a woman and a man, respectively. These diagrams illustrate the position of the bladder within the pelvis. Note how in the woman the bladder sits just in front of the cervix and womb. In the man the prostate gland sits at the neck of the bladder, surrounding the first part of the urethra.
The physiology of the urethra
 Self-test 4.3a The physiology of the urinary system
Self-test 4.3a The physiology of the urinary system
1. The urine in the bladder is usually sterile (i.e. free from infectious agents). If bacteria enter the bladder and multiply, this sort of infection is called cystitis.
2. In severe chronic kidney disease the tissue of the kidney, including the nephrons, has become permanently damaged. How do you think this might affect:
Answers
Chapter 4.3b The investigation of the urinary system
At the end of this chapter you will:
Introduction
The investigation of the urinary system involves:
• a thorough physical examination
• examination of the blood to assay waste products and salts in the serum, autoantibodies and other markers of specific diseases, and also to look for anaemia
• imaging tests to examine the structure of the urinary system, including ultrasound scan, CT scan and plain X-ray images
• imaging tests to examine the function of the urinary system, including intravenous urography (IVU), cystourethrography and radioactive isotope scans
• examination of the inside of the bladder (cystoscopy)
Physical examination
The physical examination of the urinary system involves the stages listed in Table 4.3b-I.
Table 4.3b-I The stages in the physical examination of the urinary system
Imaging tests to examine the structure of the urinary system
A plain X-ray image, although it cannot show any detail about the soft tissues, may be used to reveal the presence of kidney stones, also known as ‘calculi’. Figure 4.3b-I shows the X-ray images of the passage over time of a calculus down the left ureter.
Imaging tests to examine the function of the urinary system
Until recently, the most common of the imaging tests of function would involve the intravenous injection of a solution that contained iodine. This solution, when concentrated, shows up on X-ray images. After injection, serial X-ray images can be taken of the abdomen. The whole procedure, known as an ‘intravenous urogram’ (IVU) or ‘excretion urogram’, reveals the passage of the ‘dye’ through the urinary system, from when it is first concentrated from the blood by the kidneys and then drained into the bladder. This test can reveal abnormalities in the structure of the kidneys and ureters, as well as in their function of filtering the blood. An excretion urogram is shown in Figure 4.3b-II. An increasingly popular and more accurate form of the IVU is the CT urogram in which the CT scanner is used to locate the obstruction in the urinary system instead of a series of X-ray films.

Figure 4.3b-II • Excretion urogram showing a pale patch of contrast in the calyx of the left kidney
•The pale patch represents a large calculus (kidney stone).
 Self-test 4.3b The investigation of the urinary system
Self-test 4.3b The investigation of the urinary system
1. One of your patients goes to the local hospital department of renal medicine every 6 months because she has an abnormality of her kidneys which may lead to progressive kidney failure. This pattern of attendance would be normal in the routine hospital follow-up of a chronic disease. What investigations do you think she might have to undergo as part of her hospital appointment?
2. Gerald is in his mid-70s, and is experiencing increasing difficulty in passing urine. He is referred to a urologist for investigation of possible disease of the prostate gland. What investigations do you think Gerald might have to undergo? (As you think about your answer, bear in mind that severe obstruction to the flow of urine, such as can result from enlargement of the prostate gland, may eventually lead to kidney damage due to back-pressure.)
Answers
1. This patient will be given a brief physical examination which focuses on the assessment of blood pressure, a visual assessment of skin colour and an abdominal examination.
2. Gerald will be given a brief physical examination which focuses in particular on the abdomen and the prostate gland. The suprapubic area will be palpated to exclude an enlarged distended bladder.
An ultrasound scan of the bladder and prostate may be performed.
Chapter 4.3c Diseases of the kidneys
At the end of this chapter you will be able to:
Estimated time for chapter: Part I, 100 minutes; Part II, 60 minutes.
Introduction
The conditions studied in this chapter are (see Q4.3c-1) :
:
• Part I – disease processes that affect the kidney:
• Part II – serious consequences of disease of the kidney:
Part I: Disease processes that affect the kidney
Glomerulonephritis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 .
.
 Information Box 4.3a-I
Information Box 4.3a-I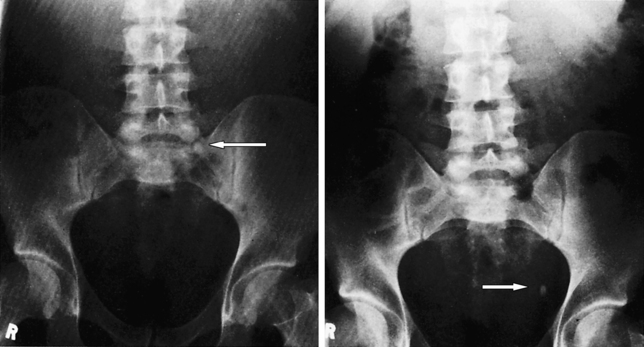
 .
. Information Box 4.3c-I
Information Box 4.3c-I
