5.1 Diseases of the endocrine system
Chapter 5.1a The physiology of the endocrine system
At the end of this chapter you will:
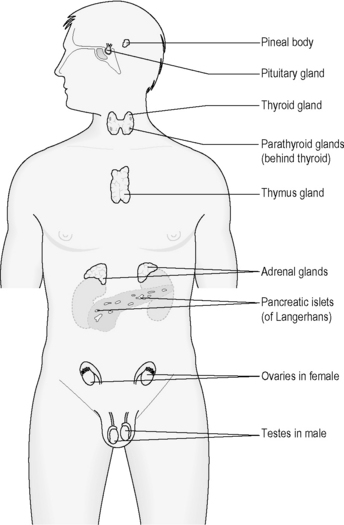
The organs of the endocrine system
Figure 5.1a-I illustrates the anatomical location of the organs of the endocrine system. This chapter focuses on the most basic physiology of those endocrine organs that are affected in the important endocrine diseases. These are:
The role of the parathyroid glands in calcium homeostasis is described in Chapters 4.2a and 4.3a. The function of the ovaries and testes will be explored in Chapter 5.2a. The pineal gland and thymus gland will be not discussed further in this text.
The negative feedback loop
These rather abstract concepts, which were introduced in Chapter 1.1c, can now be placed in more concrete terms. Endocrine cells play the role of both detector and control centre, while the release of hormone corresponds to the effector of the negative feedback loop. As a thermostat is designed to keep ambient temperature constant, the endocrine negative feedback loops work to keep bodily variables such as blood sugar or blood calcium at a steady level. This chapter offers many more examples of this negative feedback loop in action (for example see Table 5.1a-I), as each of the important endocrine organs is described in turn.
Table 5.1a-I The release of cholecystokinin (CCK): an example of the negative feedback loop in the regulation of hormones
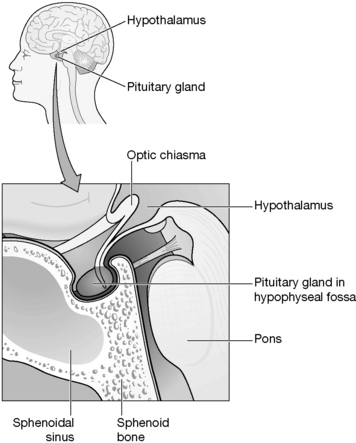
The pituitary and the hypothalamus
The pituitary gland is a pea-sized organ that projects downwards from an area at the base of the brain called the ‘hypothalamus’. The site of the pituitary is deep within the head, approximately at the level of the bridge of the nose (Figure 5.1a-II). The extra acupoint Yintang, which is considered in Chinese medicine to have a profound influence over mental functions, overlies the region of the pituitary and hypothalamus.
Table 5.1a-II lists the six hormones that are produced by the adenohypophysis.
Table 5.1a-II The hormones released from the anterior pituitary gland (adenohypophysis) and their functions
| Hormone | Function |
|---|---|
| Growth hormone (GH) | Stimulates growth in many tissues |
| Thyroid-stimulating hormone (TSH) | Stimulates the production of thyroid hormones |
| Adrenocorticotrophic hormone (ACTH) | Stimulates the production of cortisol from the adrenal gland |
| Prolactin (PRL) | Stimulates breastmilk production |
| Follicle-stimulating hormone (FSH) | Stimulates the development of the ovarian follicle (the first half of the menstrual cycle) |
| Luteinising hormone (LH) | Stimulates ovulation and the maturation of the ruptured follicle (corpus luteum) |
Growth hormone
 Information Box 5.1a-I Growth hormone: comments from a Chinese medicine perspective
Information Box 5.1a-I Growth hormone: comments from a Chinese medicine perspective
In excess, growth hormone leads to thickening of soft tissues and broadening of the bones (see Chapter 5.1e). This might be interpreted as accumulation of Damp and Phlegm. This again suggests that appropriate secretion of growth hormone is an aspect of the healthy function of the Spleen Organ.
ADH, TSH, ACTH, FSH, LH and prolactin
The role of ADH was mentioned in Chapter 4.3a. This hormone is released in response to an increased concentration of the salts in the blood. It reduces the amount of water that is lost through the urine, and is important in the control of the homeostasis of the concentration of the blood. TSH and ACTH relate to the healthy function of the thyroid and adrenal glands, respectively. PRL, FSH and LH are all important in the physiology of the reproductive system. The function of these five pituitary hormones is described in more detail in Chapter 5.2a.
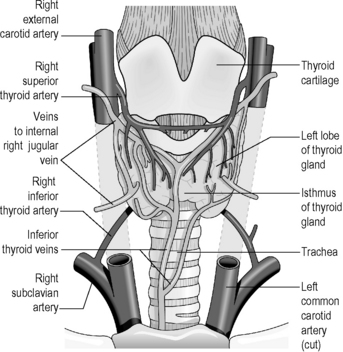
The thyroid gland
Figure 5.1a-III illustrates the thyroid gland, which is a bow-shaped organ situated just below the level of the laryngeal prominence (Adam’s apple) in the neck. The bow shape is a result of the gland being formed by two lobes separated by a narrow bridge of tissue called the ‘isthmus’. In health, the thyroid gland can be felt as a small region of vague softness below the voice box. This can be felt to rise and descend during swallowing.
 Information Box 5.1a-II Thyroid hormone: comments from a Chinese medicine perspective
Information Box 5.1a-II Thyroid hormone: comments from a Chinese medicine perspective
The consequence of an excessive secretion of thyroid hormones is the generation of a state similar to the general pattern described as Yin Deficiency (feelings of heat, anxiety and rapid heart rate). Insufficient secretion of thyroid hormones leads to a state that includes feelings of cold, lassitude, weight gain and slow heart rate (see Chapter 5.1c), which together can be compared to the pattern of Yang Deficiency. Thus these patterns suggest that the appropriate control of the thyroid hormones reflects an aspect of the fundamental balance of Yin and Yang.
The adrenal glands
Summary
 Information Box 5.1a-IV The hormones of the adrenal gland: comments from a Chinese medicine perspective
Information Box 5.1a-IV The hormones of the adrenal gland: comments from a Chinese medicine perspective
In conditions of prolonged stress, the hormones are secreted in excess. The problems of excessive blood sugar and hypertension suggest an imbalance of Spleen Qi and hyperactivity of Kidney Yang. Features of Accumulation of Damp and Phlegm may be observed in glucocorticoid and mineralocorticoid excess (see Chapter 5.1e). See Chapter 2.2c for a more detailed Chinese medicine interpretation of the diverse effects of excessive synthetic corticosteroids.
The pancreas
Insulin
• stimulating the conversion of excess blood glucose to glycogen, which can then be stored in the liver and muscles
• preventing protein and fat from being converted into sugar (thus counteracting one action of thyroxine)
• enabling the cells to take up glucose from the bloodstream (in the absence of insulin, cells are simply unable to utilise the glucose, however much there may be in the bloodstream; a state compared to ‘starvation in the midst of plenty’).
Summary
 Self-test 5.1a The physiology of the endocrine system
Self-test 5.1a The physiology of the endocrine system
1. Describe (i) the similarities and (ii) the differences between a hormone and a neurotransmitter.
3. Describe one important difference between the role of the hypothalamus and the role of the pituitary.
Answers
Both hormones and neurotransmitters act to communicate with other cells by connecting with ‘receptor’ proteins in the membranes of those cells. This connection stimulates an internal change within the cell, and thus a change in one cell has been communicated to another.
Hormones are released into the tissue fluid surrounding the endocrine cells, and often travel long distances via the bloodstream to reach their target sites.
Neurotransmitters travel a very short distance within the synaptic cleft before they reach their target site, on the membrane of a dendrite of another nerve cell.
3. To answer this question well you need first to make a distinction between the anterior pituitary (adenohypophysis) and the posterior pituitary (neurohypophysis). The neurohypophysis can be considered as a physical extension of the nerve cells of the hypothalamus. The two hormones released from the neurohypophysis are released in direct response to nervous messages reaching the hypothalamus. In this way they are similar in action to the hormone-releasing nerve cells of the hypothalamus itself.
Chapter 5.1b The investigation of the endocrine system
Introduction
The investigation of the endocrine system includes:
• a thorough physical examination
• blood tests to assess the levels of hormones in the blood
• urine tests to assess the levels of hormones excreted in the urine
• more complex blood and urine tests to assess the response of hormones to various stimuli (stimulation and suppression tests)
• imaging tests (in particular computed tomography (CT) scan and magnetic resonance imaging (MRI)) to visualise the structure of the endocrine organs.
Physical examination
The physical examination of the endocrine system involves the stages listed in Table 5.1b-I.
Table 5.1b-I The stages in the physical examination of the endocrine system
Imaging tests
For example, the pituitary gland can be clearly revealed by means of MRI. Figure 5.1b-I shows the sort of image that may be obtained. This image represents the upward growth of a pituitary tumour. Such growth can have marked endocrine consequences (as well as being very likely to impair vision by upwards pressure on the crossing of the optic nerve tracts) and also in the causation of headaches.

Figure 5.1b-I • MRI scan indicating a large pituitary tumour (extensive growth indicated by arrows).
 Self-test 5.1b The investigation of the endocrine system
Self-test 5.1b The investigation of the endocrine system
1. Janet is a middle-aged patient of yours who has been treated for hypertension for 3 years. Now her doctor is concerned that the root of her problem might be the result of excessive levels of growth hormone from her pituitary gland. This fits with that facts that Janet’s facial features have become more coarse over this time period and her shoe size has increased. The most likely cause of this syndrome is a tumour (usually benign) of the endocrine cells of the pituitary gland (see Chapter 5.1e).
Answers
1. Janet first will be given a thorough physical examination. She may be asked to bring photographs of herself in recent years, which may indicate a change in facial appearance. The specialist might observe that Janet’s hands and feet are broad for her build. As excessive growth hormone can affect the cardiovascular system in particular, this system will be examined with care. An enlarged pituitary gland can affect the vision, so the eyes and vision will also be examined in detail.
 .
. .
.
 .
. Information Box 5.1a-III
Information Box 5.1a-III .
. Information Box 5.1a-V
Information Box 5.1a-V Information Box 5.1c-I
Information Box 5.1c-I



