Gait abnormalities should be documented.
Footwear should be inspected for wear pattern and for foreign objects that may be protruding into the shoe.
Pulses, hair growth, warmth, and capillary refill should be examined for vascular disease.
Foot and heel abnormalities such as claw toes, hammer toes, bunions, skin breaks, ulcers, heel position (varus/valgus), or changes in foot shape, should all be documented thoroughly.
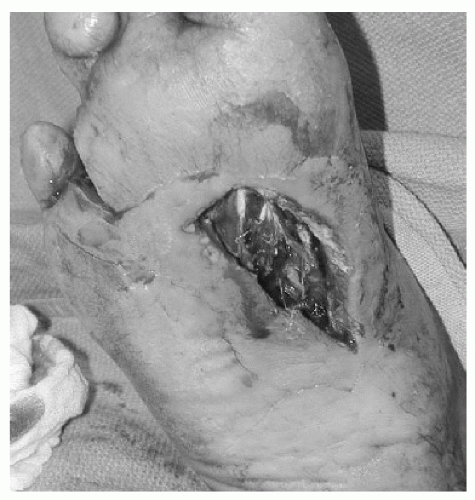
If ulcers are present, the location, size, and whether erythema or drainage is present (Fig. 5.1) should be documented.
The clinician should monitor for the presence of edema or signs of inflammation as early signs of neuroarthropathy or stress fractures.
Instability of joints should be tested.
Weakness in manual muscle testing may indicate tendon or neurologic dysfunctions.
Qualitative sensory examinations such as light touch, two-point discrimination, pin prick, and proprioception.
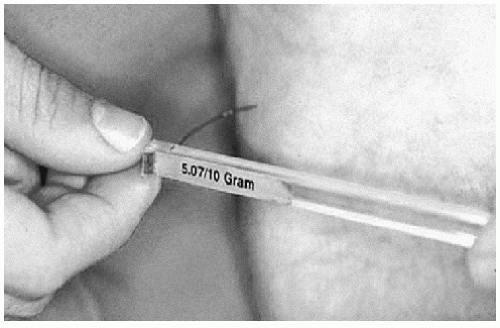
Quantitative sensory examination most commonly done using the Semmes-Weinstein monofilaments (Fig. 5.2). The monofilament is pressed onto the skin perpendicularly until it bends. The 5.07 monofilament is considered the standard for adequate sensation. However, it is important to keep in mind that 10% of patients who can feel the 5.07 monofilament can develop ulcerations.7
 Figure 5.1 A: Dorsal toe ulcer; B: Plantar MT head ulcer; C: Heel ulcer; and D: midfoot ulcer secondary to rocker bottom deformity. |
healing after amputations. However, the advent of toe pressure measurements has greatly improved the reliability of the ultrasound study. An absolute pressure of 40 mm Hg is considered the minimum toe pressure measurement needed for wound healing. However, falsely elevated values can be obtained in individuals with arteriosclerotic vessels. Other tests for assessing vascularity include the determination of skin-perfusion pressures and transcutaneous oxygen pressures. The former is a test to determine the minimum pressure needed to prevent reddening of the skin after blanching. The latter can be used to determine healing potential also after amputation.4 Pressures of less than 20 mm Hg have a high rate of wound infections, whereas readings higher than 30 mm Hg indicate adequate healing potential.
Total serum protein concentration greater than 6.2 g per dL
Serum albumin level greater than 3.5 g per dL
Total lymphocyte count greater than 1,500 per mm3
in vibratory, temperature, and pin prick perceptions; abnormal Achilles reflex; previous podiatric attendance; insensitivity to 10 g monofilament; reduced pulses; foot deformities; increased age; and abnormal ankle reflexes. Of these risk factors, prior or current ulcers, abnormal neuropathy disability score, and prior podiatric attendance were found to be highest risk factors for new foot ulcers. A combination of 10 g monofilament, neuropathy disability score, and palpation of foot pulses were recommended as a screening tool in general practice.21
important to determine infection because surrounding erythema or purulent drainage with an ulcer will usually require inpatient hospital admission for intravenous antibiotics and surgical debridement.
TABLE 5.1 WAGNER CLASSIFICATION FOR DIABETIC FOOT ULCERS | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 5.2 DEPTH/ISCHEMIA CLASSIFICATION FOR ULCERS DEVELOPED BY WAGNER AND MODIFIED BY BRODSKY | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
fifth MT tuberosity, toes, and skin overlying the anterior tibia. To reduce these complications, a well-fitting cast covering the toes should be applied and checked regularly for loosening, which could lead to pistoning-induced rubbing. Moreover, placing the cast with the ankle in neutral will help to prevent increased pressure along the anterior
often required for grossly infected wounds. The duration of therapy and choice of antibiotics will be based on culture data, extent of infection, and clinical response to treatment. Infectious disease consultation should also be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree