Tendon Disorders
Sheldon S. Lin
Eric Breitbart
Constantine A. Demetracopoulos
Jonathan T. Deland
ACUTE ACHILLES TENDON RUPTURE
The incidence of acute Achilles tendon rupture has increased over the past 50 years. A primary reason for the increase is the growing interest and participation in sports-related activities. More than 75% of all tendon ruptures occur during sports-related activities in patients between 30 and 50 years of age.
PATHOGENESIS
Etiology and Epidemiology
A sedentary lifestyle with weekend recreational athletics leads to an increased incidence of acute Achilles tendon rupture. The annual number ranges from 2 to 10 cases per 100,000 people in industrialized nations, but it is extremely rare in other parts of the world. Achilles tendon ruptures occur in younger patients (mean age 36 years) than those with other ruptured tendons (mean age greater than 60 years). Male predominance is seen in every series of Achilles tendon ruptures with a male-to-female ratio varying from 2:1 to 19:1. An increased incidence in white-collar workers or professionals with a more sedentary lifestyle has been noted. An increased incidence during the warmer months of May through August has been thought to result from the increased sporting activity during the “play season.” Achilles tendinopathy is the most common running-associated tendinopathy, and veteran runners (>10 years) have an increased risk of Achilles tendinopathy.
Less common causes of Achilles tendon rupture include the following:
Use of corticosteroids (local injection or systemic use leading to collagen necrosis) Use of anabolic steroids causing collagen dysplasia and
reduced tensile strength
Use of quinolone antibiotics
Gout, hyperthyroidism, renal insufficiency, and arteriosclerosis
Other predisposing factors include the following:
Prior Achilles tendon injury or tendinopathy
Infection, systemic inflammatory disease, and ochronosis
Hypertension and obesity
Pathophysiology
Several theories (degenerative, impaired healing, mechanical overload, etc.) have been proposed for the pathogenesis of Achilles tendon rupture. The “degenerative” theory describes a sequence of events with a sedentary lifestyle leading to a decrease in tendon vascularity. Subsequent microtrauma in a tendon with an impaired healing process leads to diffuse tendon degeneration and injury. Eventually, the impaired tendon undergoes a catastrophic failure (rupture) at a critical load.
The posterior tibial artery supplies blood to the proximal and distal parts of the tendon with the middle part supplied by the peroneal artery. In an anatomic study, the midsection of the tendon tends to be hypovascular, which may explain the high incidence of midsection tendon ruptures, especially in patients with compromised blood supply.
Several studies analyzing angiographic and histologic data support the concept of tendon degeneration. More than 15% of the patients with an acute Achilles rupture report prior symptoms. Histologic analysis of acute ruptured tendons reveals degenerative and necrotic tendon changes with hypoxic degeneration, mucoid degeneration, and calcifying tendinopathy resulting in increased water content and decreased collagen content. There is also an increase in denatured and damaged collagen in Achilles tendinopathy indicating an increased collagen turnover rate.
Structural changes of the Achilles tendon occur as a part of normal aging. These changes include decreased cell density, decreased collagen fibril diameter and density, and loss of fiber waviness, which may explain the increased prevalence of ruptures in older patients.
DIAGNOSIS
Physical Examination and History
Classically, an acute Achilles tendon rupture is diagnosed by the patient’s history.
Most patients describe feeling a direct blow localized to the posterior aspect of the ankle or hearing a “pop.”
It most commonly occurs during an explosive gastroc-soleus eccentric contraction.
Twenty-five percent of diagnoses are missed in the emergency department because of presence of active plan-tarflexion when non-weight bearing and swelling over the Achilles tendon, which makes palpation of the defect difficult. A history of steroid or flouroquinolone usage.
A history of endocrine disorders or systemic inflammatory conditions.
A positive Thompson squeeze test (0.96 sensitivity and 0.93 specificity).
A palpable defect (0.73 sensitivity and 0.83 specificity).
Clinical Features
Difficulty with ambulation and weakness on attempted pushoff is noted.
Physical examination demonstrates an indentation of the posterior aspect of the tendon initially. With the onset of soft-tissue swelling, these findings are frequently masked.
Ecchymosis and swelling commonly develop along the posterior aspect of the ankle (Fig. 8.1).
The calf squeeze test (Thompson sign) is the simplest and most reliable test to evaluate the continuity of the gastrocnemius-soleus complex. Absence of plantarflexion of the foot against gravity on squeezing of the calf with the patient in a prone position confirms a ruptured Achilles tendon.
Another finding is the “hyperdorsiflexion sign,” which results in a relatively dorsiflexed position compared with the intact contralateral side; however, this sign may be difficult to elicit following an acute injury, secondary to pain inhibition until sufficient time has elapsed after injury.
Radiographic Features
Plain radiographs are of limited value for an acute Achilles tendon rupture.
Rarely, an acute avulsion of the Achilles insertion with proximal migration of bony fragments can be seen.
Definitive treatment of this rare condition requires an advancement of the Achilles tendon and internal fixation of the bone-tendon complex (Fig. 8.2).
Magnetic resonance imaging (MRI) demonstrates an Achilles tendon rupture, but is not necessary for diagnosis or treatment (Fig. 8.3).
MRI is superior to other imaging technique for diagnosing partial ruptures of the Achilles tendon.
Ultrasound (US) can be used to assess the gap between the tendon ends. With the foot held in plantarflexion, the presence or absence of a gap between the tendon ends can help determine the success of nonoperative management of Achilles tendon rupture.
Serial US studies can be used to determine the proximal migration of the tendon tear and its potential for healing.
TREATMENT
Nonsurgical Treatment
Nonoperative treatment is associated is higher risk of rerupture compared with the risk associated with operative treatment (1.7% to 10%); however, it has significantly lower risk of impaired wound healing, wound infection, and nerve damage.
The use of serial casting or a solid removable boot in plantarflexion helps to join the ends of the ruptured tendon. It should be noted that immobilization in a cast or boot in neutral ankle position is inadequate care.
Surgical Indications
Recently, advances in surgical technique have led to superior results in most series compared with nonoperative management. Aggressive postoperative protocols have demonstrated the benefits of functional rehabilitation with improved function, increased patient satisfaction, acceptable complication rate, and avoidance of cast immobilization disease (muscle atrophy, loss of muscle or tendon strength, and stiffness). Currently, surgical repair with functional rehabilitation has gained increasing acceptance. Nonoperative management should be used for patients with significant medical issues or limited functional gains and expectation.
The AAOS Guideline has a consensus recommendation that surgical management should be approached with caution in a patient with the following conditions:
diabetes
neuropathy
history of tobacco use
obesity
a sedentary lifestyle
peripheral vascular disease
local or systemic
age more than 65 years dermatologic disorder
immunocompromised state
The basic concept of surgical repair of an acute Achilles tendon rupture is to durably restore the continuity of the ruptured tendon, such that healing occurs in a physiologic position, allowing for restoration of the normal muscle function. This goal may be technically challenging when the ends of the degenerative Achilles tendon are frayed.
Several suture and repair techniques have been advocated to achieve this goal. The first end-to-end suture technique for ruptured tendon was popularized by Bunnell and Kessler. Currently, more popular techniques include the six-strand suture technique, suture weave, Krackow stitch, and three-bundle technique. New percutaneous techniques have been described, with less initial pain and a smaller scar, but concerns exist regarding potential complications including sural nerve injury and possibly rerupture.
In addition to these various suture constructs, several augmentation techniques have been described, using either a gastrocnemius turndown flap or the plantaris tendon. Although these constructs do augment the soft tissues and theoretically may improve the strength of the repair, their routine use and benefit have not been confirmed in an acute Achilles repair.
Surgical Technique
Surgery can be performed either before significant swelling or after soft-tissue injury resolution.
The patient is placed in the prone position. Both feet can be prepped into the operative field to allow for side-to-side comparison of the resting dynamic tension of the repaired tendon.
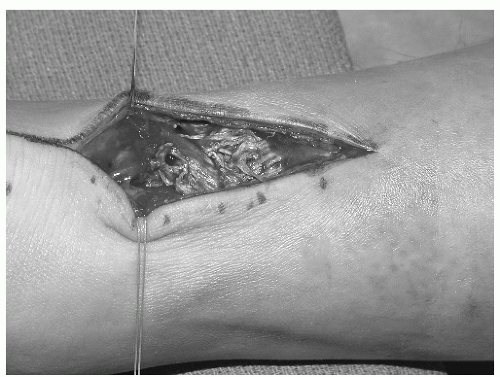
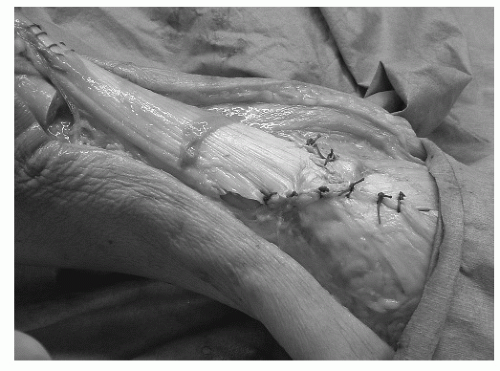
An incision is made over the rupture from medial to the posterior midline of the Achilles tendon to avoid injury to the sural nerve; the paratenon is split longitudinally and can be tagged with suture on the medial and lateral aspects to facilitate closure at the end of the operation (Figs. 8.4 and 8.5).
The ragged ends of the proximal and distal Achilles tendon are trimmed and repaired with a large (no. 3) nonabsorbable suture using a modified whip (Bunnell, Kessler, or Krackow) stitch. Depending on the size of
the tendon, one or two strands of suture can be used at each end (Fig. 8.6).
One critical step is to accurately assess the dynamic resting tension of the Achilles tendon.
The goal is to approximate the two ends of ruptured tendon together with the appropriate tension to achieve a comparable foot position similar to the opposite foot.
Subtle adjustments to the suture tension can be made to achieve appropriate tension of the tendon.
Once the ends are tied, the suture knots should be secured in the anterior position to minimize soft-tissue irritation and adhesions.
A circumferential 3-0 absorbable running suture can be used to reinforce the repair.
Another technique to reinforce the repair and minimize the soft-tissue adhesion is to release the plantaris tendon (absent in 15% of the patients) and fan it over the repair site (Fig. 8.7). This step may improve the outcome by preventing adhesions and reinforcing the surgical repair.
Subsequently, the paratenon is approximated with absorbable suture. The soft tissue is closed in the standard fashion, and a standard posterior splint is applied in mild plantar flexion.
Postoperative Management
Prolonged cast immobilization leads to “cast disease,” with muscle atrophy, joint stiffness, adhesions, and cartilage atrophy. Both nonoperative and operative techniques for Achilles repair have demonstrated significant permanent functional deficits (based on Cybex testing) following prolonged cast immobilization.
The basic concept of functional rehabilitation protocols is to avoid the morbidity of cast immobilization with an acceptable complication rate to facilitate the remodeling and maturation phase of tendon repair. Early limb and joint mobilization minimizes muscle atrophy and joint stiffness. During the remodeling phase, the functional activity may assist in the organization of the collagen fibers along their proper orientation to ideally resist the tensile forces. Subsequently, during the maturation phase, the rehabilitation protocol stimulates the intrinsic tendon healing processes with increasing collagen cross-linking, which leads to increased strength.
Functional Rehabilitation Protocol
Patients should be immobilized for 10 to 14 days for the incision to heal.
Once the sutures are removed (by day 14), weight bearing is initiated with a hinged range-of-motion (ROM) boot, removable splint, or ankle-foot orthosis (AFO) that permits ankle motion. Early functional weight-bearing and ROM exercise have superior outcomes compared with early immobilization.
Rehabilitation of the Achilles tendon begins with progressive ROM exercises and accelerated weight bearing.
Close attention for any symptoms of overuse during the retraining phase is necessary.
If excessive pain or swelling occurs, the rehabilitation protocol may be slowed down.
Initially, the patient is encouraged to perform progressive ROM exercises and increase their weight-bearing status to full weight by 4 weeks.
Isometric exercises are useful during the initial phase of rehabilitation. Active plantarflexion with passive dorsiflexion (stretching with a strap or towel) is encouraged, and pushoff strengthening can be started with a stair-climbing device.
By 10 to 12 weeks, single heel rise, increasing pushoff activities, and jogging exercise are started.
Complications
Acute Achilles tendon ruptures may be missed during the initial evaluation in as many as 25% of the patients, leading to misdiagnosis, unsuccessful management, or rerupture. If the diagnosis is uncertain, advanced imaging studies such as MRI or US may confirm the diagnosis, but these are generally unnecessary.
Complications exist for both the nonoperative and operative management of acute Achilles tendon rupture. For these reasons, there has been little consensus regarding their ideal management. The major complication of nonoperative management with cast immobilization is the incomplete return to function as a result of the loss of functional continuity of the tendon with appropriate dynamic resting length. Tendon reruptures are three to four times more common after nonoperative treatment.
The most serious operative complications include infection, adhesions, nerve injury, and wound dehiscence (Fig. 8.8). Soft-tissue dehiscence with infection can be disastrous as a result of the limited soft-tissue coverage options. Percutaneous surgery is associated with sural nerve damage, but overall it has reduced risk of complications. Postoperative thromboembolic events, such as deep vein thrombosis, are common in patients who receive an Achilles tendon rupture repair. Initial treatment comprises early weight-bearing and ROM exercises, oral antibiotics, and wound debridement. Adjunct treatments include local topical antibiotics (silver sulfadiazine) or exogenous growth factors (e.g., Regranex, Ortho-McNeil, Raritan, New Jersey) that may facilitate the granulation process. For large wound defects, a conservative approach may be attempted with local wound care or a wound suction device (Wound VAC, KCI, San Antonio, Texas). In rare instances, a free flap is required.
Results and Outcomes
Recently, improved outcomes and a trend toward fewer complications have been reported. A meta-analysis, published in 2005, of 12 trials involving 800 patients concluded that open operative treatment (3.5%) of acute Achilles tendon ruptures significantly reduces the risk of rerupture compared with nonoperative treatment (12.6%), but operative treatment is associated with a significantly higher risk (26.1%) of other complications. Operative risks may be reduced by performing surgery percutaneously (8.3% risk of complications). Postoperative splinting with use of a functional brace reduces the overall complication rate.
CHRONIC RUPTURES OF ACHILLES TENDON
Many patients have significant delay in diagnosis of an acute Achilles tendon rupture. Even though the patient is able to walk or function to some extent, compromised pushoff strength limits activities, such as sporting activities and climbing stairs. This delay in treatment leads to much more complex reconstructive options.
PATHOGENESIS
A delay greater than 4 to 6 weeks is considered a “chronic Achilles tendon rupture.” The tendon sheath becomes thickened, whereas repair tissue fills the gap. Any delay beyond 2 weeks allows the gap to fill with fibrous scar tissue in a disorganized pattern. Over time, the disorganized scar tissue can stretch and elongate, exacerbating proximal muscle tendon retraction.
DIAGNOSIS
Physical Examination and History
Clinical Features
The diagnosis of chronic Achilles rupture may be difficult to confirm on physical examination.
The physical examination may demonstrate a significant soft-tissue deficit, but often scar tissue fills the area resulting in loss of functional continuity.
One test, the hyperdorsiflexion sign (Matles test), demonstrates greater maximum passive dorsiflexion on the injured side than on the uninjured side when the patient is prone.
This loss of symmetry usually indicates a compromised Achilles tendon complex.
Decreased plantarflexion strength helps confirm the presence of a compromised Achilles tendon.
Manual testing may be performed, but is often difficult because of the secondary recruitment of other ankle plantarflexors.
Clawing of the toes and an increase in the medial arch of the foot may result from the accommodation by the flexor digitorum longus (FDL) muscle for the functional loss of the gastrocnemius and soleus muscles.
Although a patient may be able to perform a single heel rise, repetitive heel rises are too difficult.
The calf squeeze test (Thompson test) has a positive finding if the plantarflexion on the affected side is less than the unaffected side.
For equivocal cases and high-level professional athletes, objective testing can be used to determine the exact isokinetic strength and power.
Cybex motor testing can be performed through the motion of ankle dorsiflexion and plantarflexion and analyzed as a percentage deficit of the contralateral normal side.
A careful history regarding general daily activities, athletic interests, work issues, and treatment expectations is important.
Even though the patient is able to walk or function to some extent, significant compromised pushoff strength exists.
Activities such as single or repetitive heel rise or activities involving stairs often are not possible.
Radiologic Features
Plain radiographs usually do not demonstrate any significant osseous findings after a chronic Achilles rupture.
A subtle soft-tissue finding is the presence of increased density consistent with the calcification of the proximal or distal Achilles tendon end (Fig. 8.9).
One critical parameter is the size of the gap defect between the tendon ends. In many patients with chronic Achilles rupture, a palpable gap exists.
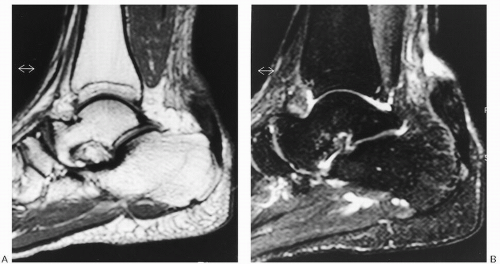
MRI or US can be used to confirm the diagnosis and determine the extent of retraction of the proximal tendon and length of the defect (Fig. 8.10).
Increased signal intensity on a T2-weighted image is present in the tissue at the gap deficit.
Some surgeons think an MRI study may be of limited value for the patient who has a chronic Achilles rupture because the patient will require surgical intervention; an intraoperative evaluation may be most useful to determine the type of Achilles reconstruction technique.
 Figure 8.9 Lateral X-ray of ankle demonstrating proximal calcified density consistent with retracted chronic ruptured Achilles tendon. |
Diagnostic Workup
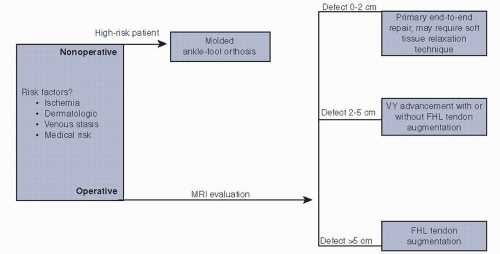
See Algorithm 8.1 for the diagnostic workup of chronic rupture of the Achilles tendon.
TREATMENT
Surgical Indications and Contraindications
The surgical reconstruction of chronic Achilles rupture requires significant soft-tissue dissection. Ideally, the clinical scenario is optimized by minimizing the various risk factors for wound compromise, such as having the patient quit smoking or discontinue the use of certain medications (e.g., immunosuppressant anti-inflammatory medications) as well as accomplish the appropriate workup for chronic swelling, venous stasis, or lower limb ischemia. Certain patients may not be surgical candidates for reconstruction if chronic dermatologic or arterial/venous problems are significant.
For patients with local surgical contraindications (chronic venous stasis ulcer, lower extremity ischemia) or significant medical contraindication, brace management is a nonsurgical alternative. The standard brace option includes a molded polypropylene AFO with or without spring-loaded hinge. The standard AFO permits passive dorsiflexion with resistance. The spring-loaded component may provide a significant amount of torque and strength. Even though this alternative may improve some functional deficits, most active patients who are candidates for surgical reconstruction will not tolerate a brace long term and desire surgical reconstruction.
Surgical Concepts
Several concepts must be considered regarding chronic Achilles tendon reconstruction. Ideally, the repaired gastrocnemius-soleus complex will heal with appropriate muscle tension and absence of muscle atrophy. End-to-end contiguous tendon repair is usually not obtainable because there is significant gap secondary to the proximal tendon retraction. The first concept consists of vascularity of the repair site. The blood supply to the Achilles tendon plays a critical role in the healing process. The blood supply arises from the paratenon, the musculotendinous junction, and the distal tendon insertion. Local scarred soft tissue often demonstrates suboptimal local vascularity, which can compromise the healing process. Several techniques involving autologous soft-tissue augmentation (i.e., strips of fascia lata, proximal Achilles turndown, and plantaris tendon weave) are avascular free tendon grafts. Even the V-Y tendon advancement involves significant soft-tissue dissection and comprises mainly of avascular tissue transfer. Even so, tendon healing does occur after a tendon advancement technique with resumption of strength and activities.
Another concept is the type of tendon transfer for augmentation of a deficient Achilles tendon. Flexor tendons, such as peroneus brevis, FDL, and flexor hallucis longus (FHL) have been proposed for the augmentation of the chronic Achilles tendon rupture. The selection of a donor tendon requires consideration of its phase, its relative strength, and the donor morbidity with regard to the loss of function. Theoretically, the FHL tendon transfer has the benefit of in-phase transfer, increased relative strength compared with the FDL, and minimal effect upon hallux function; therefore, it is currently the most commonly used technique. In addition, the transfer of the FHL most closely reproduces the axial contractile forces of the Achilles tendon and provides a local contiguous muscle for revascularization of the scarred tendon bed.
Most surgeons base their Achilles tendon reconstruction technique on the length of the gap deficit of the Achilles tendon, although other factors such as the length of delay, the age and athletic expectations of the patient, and muscle quality of the gastrocnemius-soleus complex may be important. The gap deficit is a key determining factor because certain techniques may be performed only
with minimal soft-tissue defect. One may be able to palpate the deficit and determine its length or it may be estimated preoperatively with MRI or US.
with minimal soft-tissue defect. One may be able to palpate the deficit and determine its length or it may be estimated preoperatively with MRI or US.
Surgical Technique
Defects 0 to 2 cm Long
For a minimal defect, it is possible to achieve a primary end-to-end repair without any additional augmentation or reconstruction. The muscle can usually be mobilized after the primary repair in a similar protocol to an acute rupture, with the foot held initially in minimal plantarflexion. For a defect of 1 to 2 cm, gradual soft-tissue relaxation stretching technique is used. After the sutures are placed in the proximal tendon, 10 to 15 lb of traction is applied manually or with a weight for 10 minutes to stretch and relax the contracted gastrocnemius-soleus complex. This technique should easily gain up to 2 cm in length and allow an end-to-end repair without significant foot equinus contracture. Occasionally, the scar completely fills the gap, but the tendon has “healed” in a lengthened fashion. One can consider Z-shortening tenotomy (opposite of Z-lengthening) with appropriate tensioning and repair with resection of the redundant tendon.
A standard posteromedial approach is used, similar to the repair of an acute Achilles rupture. This approach avoids the sural nerve and allows the use of the plantaris tendon, if necessary.
The paratenon should be carefully split and preserved for later repair.
The bulbous ends are identified, and both the distal and the proximal ends are resected to remove the disorganized fibrous scar tissue.
The end-to-end tendon repair is performed with no. 3 nonabsorbable suture using a standard technique (whip stitch or modified Krakow).
The paratenon and soft tissue are closed in a sequential fashion.
The postoperative protocol is similar to an acute Achilles tendon repair.
Defects 2 to 5 cm Long
For a larger defect, several options exist, including V-Y advancement with or without FHL tendon transfer augmentation. The V-Y advancement avoids sacrifice of a normal muscle tendon unit. This procedure relies on a functional muscle and theoretically may not work if significant scarring or severe atrophy exists within the gastrocnemius-soleus complex. Often, an atrophied gastrocnemius soleus muscle can still be mobilized and rehabilitated with sufficient function. The V-Y advancement technique has been reported in several series with restoration of plantarflexion strength and with minimal complications of soft tissue compromise and sural neuritis.
Advancement of the proximal Achilles tendon in a V-Y fashion has been described as an augmentation technique for chronic Achilles rupture (Fig. 8.11).
Using a longitudinal posterior incision, an inverted V-shaped incision is made in the muscle tendon junction of the gastrocsoleus aponeurosis. Care must be taken not to violate the underlying gastrocnemius muscle, which is attached to the anterior paratenon.
The arms (approximately 12 to 18 cm in length depending on the size of the defect) of the V must be at least one-and-a-half times the length of the gap deficit to allow for the appropriate proximal limb closure of the Y (Fig. 8.12).
The critical aspect is adequate soft-tissue dissection with preservation of the posterior muscle in continuity and advancement of the proximal soft tissue for tendon coverage.
An end-to-end repair is performed using the standard suture technique described earlier, and the limbs of the Y are closed with no. 2 nonabsorbable suture (Fig. 8.13).
Postoperative rehabilitation is as described earlier.
Defects Longer Than 5 cm
For a defect longer than 5 cm, few options exist. One option is to perform a turndown flap, but criticisms exist regarding the bulk of the tendon at the point of the turndown. Surgical options include the use of a flexor tendon transfer (FHL or FDL) alone or in combination with the V-Y advancement technique described earlier.
The procedure is performed with the patient in the supine position with contralateral hip bump. A thigh tourniquet is used.
Attention is first directed to the medial border of the foot, where the FHL is harvested.
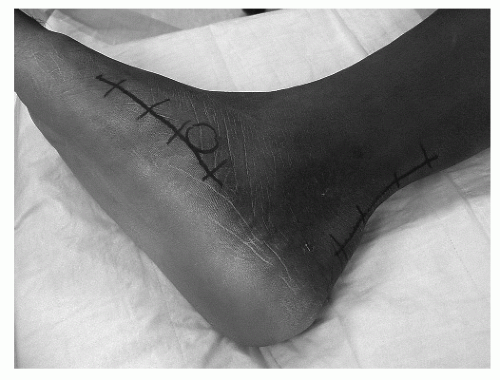
A longitudinal incision is made along the medial border of the midfoot just above the abductor muscle, from the navicular to the head of the first metatarsal (Fig. 8.14).
The skin and subcutaneous tissue are sharply reflected down to the fascia.
The abductor with the flexor hallucis brevis muscle is reflected plantar, exposing the deep midfoot.
The FHL and FDL are identified within the substance of the midfoot.
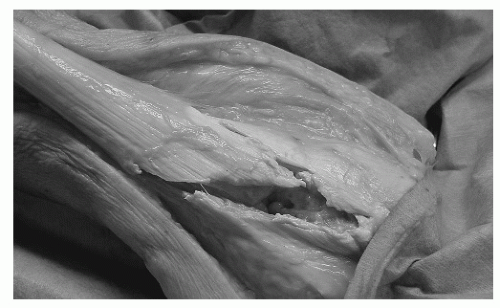
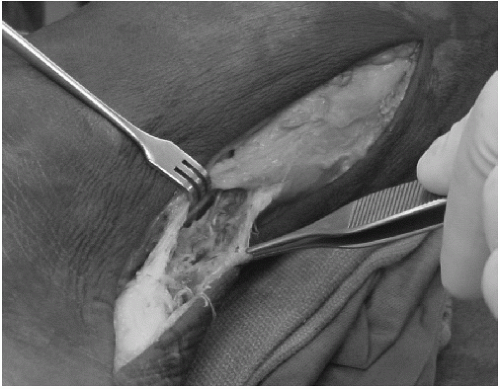
The FHL is divided as far as possible, allowing the distal stump adequate length for transfer to the FDL (Fig. 8.15). The proximal portion is tagged with a suture.
The distal limb of the FHL is sewn into the FDL with the toes held in neutral position.
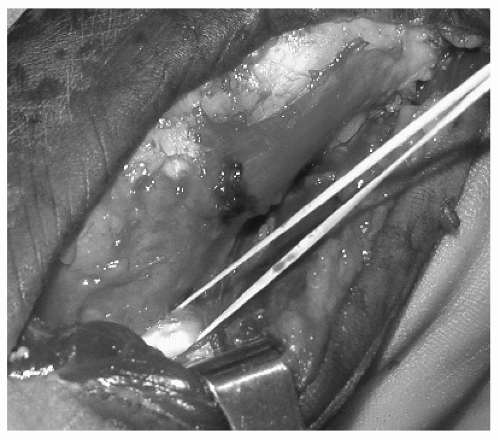
A second longitudinal incision is made along posteromedial aspect of the Achilles, starting from the level of its musculotendinous junction to 1 in below its insertion on the calcaneus (Fig. 8.16).
The paratenon of the tendon is opened longitudinally, and the substance of the tendon is evaluated (Fig. 8.17).
Care is taken to dissect deep to the paratenon to create full-thickness skin flaps and avoid any skin sloughs.
The deep fascia over the posterior compartment of the leg is incised longitudinally, and the FHL is identified.
The tendon is retracted from the midfoot into the posterior incision.
A transverse drill hole is made approximately 1.0 to 1.5 cm distal and anterior to the superior calcaneal process perpendicular to the calcaneus.
A lateral incision is made over the drill hole with care to avoid damaging the sural nerve. A curette is used to smooth the sharp edges.
A suture passer is placed through the bone tunnel from lateral to medial. The tagged suture is passed through the tunnel, drawing the FHL tendon through the drill hole.
A blunt hemostat is subcutaneously passed from the medial incision to the lateral incision, and the newly transferred FHL is passed proximal and medial.
The FHL is then woven from distal to proximal through the Achilles tendon with a tendon weaver, using the full length of the harvested tendon (Fig. 8.18).
Some surgeons advocate harvesting the FHL through the posterior incision as far distal along the medial calcaneus as possible. It is then anchored to the calcaneus just deep to the Achilles insertion with an interference screw.
Care is taken to maintain the foot in 10° of plantar flexion.
Complications
Rerupture: Higher incidence in patients with inflammatory disorders or on drugs such as steroids.
Ankle stiffness: Avoid extreme plantarflexion position of the foot, proper tension of repair.
Wound necrosis: Minimize with soft-tissue handling, full-thickness flap, and appropriate immobilization.
Infections: Potentially devastating, treat with wound care, possible skin graft or flap.
Results and Outcomes
In general, the surgical treatment of chronic Achilles tendon ruptures with some type of gastrocsoleus repair and FHL transfer has yielded good results.
NONINSERTIONAL ACHILLES TENDINOSIS
Renewed interest in sports activities and increased duration and training intensity have led to a significant increase in overuse injuries of the Achilles tendon. Noninsertional Achilles tendinosis comprises a wide spectrum of clinical presentations, with the most common subset of patients being the high-level athlete who presents with an inflamed Achilles tendon 2 to 6 cm above its insertion. Another subset of patients comprises the older, sedentary patient who presents with an inflamed heel consistent with insertional Achilles tendonitis (discussed elsewhere). A third subset
comprises young males with seronegative arthropathy who present with an Achilles insertional enthesopathy.
comprises young males with seronegative arthropathy who present with an Achilles insertional enthesopathy.
PATHOGENESIS
Etiology
The development of Achilles tendinosis has been attributed to an overuse phenomenon, especially running activities, leading to excessive forces on the Achilles tendon. Forces on the Achilles tendon approximate 10 times the body weight during running. A significant correlation between the incidence of Achilles tendinosis and the intensity of training or excessive training has been found.
Classically, the overuse phenomenon occurs in a high-end athlete who subjects his or her tendons to repetitive stresses beyond its ability to heal. Patients commonly report a change in training pattern or activity with the subsequent development of symptoms. Changes, such as increased duration, type of activity, or frequency of sports activities, are commonly noted findings. More subtle changes include alterations in athletic shoewear or local changes in the running environment. Whether the patient is a high-end athlete or mainly sedentary, alterations in training patterns or environment may lead to Achilles tendinosis.
Overuse injuries of the Achilles tendon are increasing and occur in 6.5% to 18% of all runners and in one study was diagnosed in 56% of elite middle-aged runners. A relatively high number of cases of noninsertional Achilles tendinosis occurs in other athletic activities, including those who dance ballet or play soccer, basketball, tennis, or racquetball. Repetitive overuse with increased biomechanical stress placed upon the Achilles tendon is a contributing factor in all of these activities.
Pathophysiology
The blood supply of the Achilles arises from the osseous insertion, musculotendinous junction, and ventral mesotenal vessels. Injection studies have shown that the ventral vessels are fewest 2 to 6 cm proximal to the Achilles tendon insertion, correlating to the area of reduced vascularity and the site of pathology. Neovascularization of the tendon is considered an important etiologic factor and a pain generator in Achilles tendinopathy. Doppler ultrasound has been used to demonstrate neovascularization in Achilles tendons with tendinopathy. Abnormal vessels have been found in the ventral aspect of the tendon adjacent to Kager triangle. These vessels are accompanied by proliferating nerves that are hypothesized to be integral in pain transmission.
TABLE 8.1 CLASSIFICATION OF NONINSERTIONAL ACHILLES TENDONITIS | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Classification
A histopathologic classification system has been developed for noninsertional tendinosis with three distinct subgroups (Table 8.1).
DIAGNOSIS
Physical Examination and History
Clinical Features
The triad of symptoms of Achilles tendonitis are pain, swelling localized 2 to 6 cm above the Achilles tendon insertion, and impaired performance.
Increased pain during exercise progresses to constant pain, independent of physical activities.
In acute paratenonitis, the tendon appears acutely swollen, edematous, and tender.
Gentle compression of the tendon at the swollen foci reproduces the symptoms.
Often crepitation is noted during ankle ROM.
For ambiguous cases, an MRI scan may differentiate whether tendinosis is present along with the finding of slight thickening of the paratenon (Fig. 8.19).
Paratenonitis with tendinosis has increased symptoms with maximum point tenderness and irregularity within the tendon substance.
The pain is more severe and reproducible with palpation of the diffusely thickened tendon.
Isolated tendinosis comprises an area of localized irregularity, swelling, and pain with significant weakness in pushoff strength.
Increased dorsiflexion motion may exist secondary to elongation.
 Figure 8.19 T2-weighted MRI study of Achilles, sagittal view, demonstrating increased signal within the paratenon consistent with Achilles paratenonitis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|