Anatomy and Biomechanics of The Foot and Ankle
Constantine A. Demetracopoulos
Jonathan T. Deland
An understanding of the functional anatomy of the foot and ankle is mandatory if any meaningful attempt at addressing the pathoanatomy is to be undertaken. This chapter provides basic anatomy and biomechanics of the foot and ankle as a basis for treating its disorders.
TERMINOLOGY
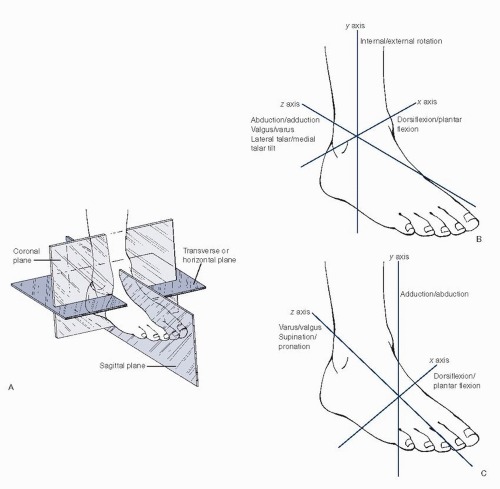
Understanding the terminology used to describe the various positions of the foot and ankle is necessary for effective communication. Unfortunately, there are ambiguities in the literature as different terms are used to describe the same positions and motions. In most descriptions of extremity position and motion, the midsagittal plane of the body is used as a reference when describing varus, valgus, abduction, and adduction. In the foot, hallux varus and hallux valgus are consistent with this convention (Fig 1.1). In terms of describing abduction or adduction of the hallux, the reference shifts to the longitudinal axis of the foot defined as a plane through the mid axis of the second metatarsal to the heel. Movement of the hallux away from this axis is termed abduction, whereas the opposite motion is termed adduction.
Motion and position of the foot and ankle are most easily defined using a familiar triaxial orthogonal coordinate system (Fig 1.2).
Pronation of the foot refers to the triplanar motion of the foot combining abduction, eversion, and dorsiflexion, resulting in elevation of the lateral border of the foot.
Supination refers to the triplanar motion combining adduction, inversion, and plantarflexion, resulting in elevation of the medial border of the foot.
The position of the heel (i.e., the calcaneus) is described relative to the talus using the ankle coordinate system. The positional terms equinus and calcaneus are sometimes used and are synonymous with calcaneal plantarflexion and dorsiflexion, respectively.
ANATOMY OF THE FOOT AND ANKLE
Skin and Subcutaneous Fascia
The skin on the dorsum of the foot is thin, loosely connected to its underlying fascia, and nearly void of subcutaneous fat. This makes the skin relatively mobile, giving some leeway in dorsal surgical exposures and making palpating the underlying structures relatively easy. In contrast, strong vertical fibrous elements of the heel, medial and lateral borders, and ball of the foot tightly bind the skin on the plantar surface of the foot. These vertical fibers form adipose-filled chambers, or septa, that are enlarged under the heel and ball of the foot, acting as shock absorbers. Traumatic or surgical destruction of the septa or atrophy of the adipose tissue by steroid injection can permanently impair their shock-absorbing function, leading to pain. The robust blood supply of the plantar skin originates mainly from the medial and lateral plantar arteries and the common plantar digital arteries, allowing the surgeon substantial leeway as to the orientation and number of incisions that can safely be made in this region. The superficial intradermal and subdermal venous system anastomoses with a dorsal system medially and laterally. Lymphatic drainage from the plantar aspect of the foot flows to the dorsal aspect through the webspaces, accounting for why infections in the plantar surface of the foot can cause swelling dorsally.
Bony and Joint Anatomy
The foot has 26 bones, a variable number of sesamoids (usually two) and accessory ossicles, with 34 joints. Classically, the foot is divided into the forefoot, midfoot, and hindfoot.
Forefoot
The forefoot contains 5 metatarsals and 14 phalanges, and extends up to the tarsometatarsal joint (Lisfranc joint). By
convention, sequential numbering of the toes and their associated metatarsals (or “rays”) starts medial at the hallux, designated number 1, to lateral, designated number 5. Similarly, the intermetatarsal spaces and webspaces are numbered from 1 to 4 from medial to lateral, respectively. The hallux has 2 phalanges, whereas the lesser toes each have three. Approximately 15% of people have only 2 phalanges in their fifth toe. Metatarsals 1, 2, and 3 each have an associated cuneiform at their base. The metatarsals 4 and 5 have an articulation with the cuboid at their base. The metatarsals are unique in that they are the only long bones to support weight perpendicular to their longitudinal axis. The distal metatarsal epiphysis (metatarsal head) has two plantar enlargements called condyles. The lateral (fibular) condyle is more prominent than the medial (tibial) condyle. The lengths of the metatarsals vary. Most commonly, the first metatarsal is shorter than the second with a progressive cascade of shortening in the remaining rays. All of the metatarsals incline to some extent with respect to the weight bearing surface. The first metatarsal has the highest inclination (15° to 25°), with the remaining metatarsals demonstrating decreasing angles from medial to lateral: second metatarsal at 15°, third metatarsal at 10°, fourth metatarsal at 8°, and fifth metatarsal at 5°. In normal stance, the metatarsal heads rest evenly on a flat surface. The first ray bears two-fifths of the weight distribution, whereas the four lesser rays share the remaining three-fifths. The fourth, and first and to a lesser extent the first metatarsals are mobile in the sagittal plane, whereas the second and third are relatively fixed in position by stable articulations at their respective cuneiforms.
convention, sequential numbering of the toes and their associated metatarsals (or “rays”) starts medial at the hallux, designated number 1, to lateral, designated number 5. Similarly, the intermetatarsal spaces and webspaces are numbered from 1 to 4 from medial to lateral, respectively. The hallux has 2 phalanges, whereas the lesser toes each have three. Approximately 15% of people have only 2 phalanges in their fifth toe. Metatarsals 1, 2, and 3 each have an associated cuneiform at their base. The metatarsals 4 and 5 have an articulation with the cuboid at their base. The metatarsals are unique in that they are the only long bones to support weight perpendicular to their longitudinal axis. The distal metatarsal epiphysis (metatarsal head) has two plantar enlargements called condyles. The lateral (fibular) condyle is more prominent than the medial (tibial) condyle. The lengths of the metatarsals vary. Most commonly, the first metatarsal is shorter than the second with a progressive cascade of shortening in the remaining rays. All of the metatarsals incline to some extent with respect to the weight bearing surface. The first metatarsal has the highest inclination (15° to 25°), with the remaining metatarsals demonstrating decreasing angles from medial to lateral: second metatarsal at 15°, third metatarsal at 10°, fourth metatarsal at 8°, and fifth metatarsal at 5°. In normal stance, the metatarsal heads rest evenly on a flat surface. The first ray bears two-fifths of the weight distribution, whereas the four lesser rays share the remaining three-fifths. The fourth, and first and to a lesser extent the first metatarsals are mobile in the sagittal plane, whereas the second and third are relatively fixed in position by stable articulations at their respective cuneiforms.
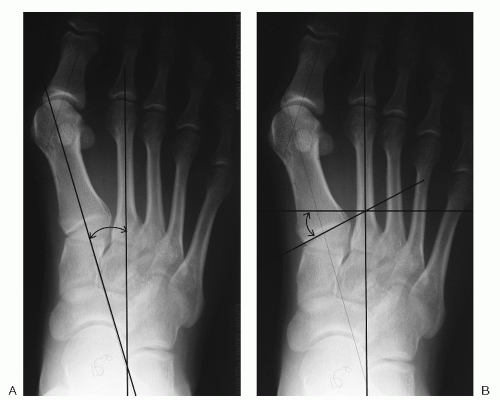
 Figure 1.1 Hallux valgus (A) and hallux varus (B) as referenced from the midsagittal plane of the body. |
The trapezoid-shaped base of the first metatarsal and the distal surface of the medial cuneiform comprise the first tarsometatarsal joint. A facet on the lateral base of the first metatarsal that articulates with the medial base of the second metatarsal is sometimes present. The medial inclination of this joint in the transverse plane varies but is usually between 8° and 10°. Greater angles may correlate with varus alignment of the first metatarsal. The angle between the first and second metatarsals (the first intermetatarsal angle) is typically less than 10° (Fig 1.3). Motion at the first tarsometatarsal joint does not lie directly in the sagittal plane but rather from dorsomedial to plantar lateral. The plantar first metatarsal cuneiform ligament provides the major restraint for dorsiflexion. Plantar intermetatarsal ligaments interconnect the bases of metatarsals two through five. The first ray, however, has no such connection to the second ray. The absence of an intermetatarsal ligament allows the first ray more mobility in the sagittal plane. Hypermobility of the first tarsometatarsal joint has been implicated in hallux valgus and metatarsus primus varus and is sometimes a component of adult acquired flatfoot deformity.
Hallux and First Metatarsophalangeal Joint
The first metatarsophalangeal (MTP) joint of the hallux is a shallow ball-and-socket type joint with a passive arc of motion between 40° to 100° in dorsiflexion and 3° to 43°
in plantarflexion. Motion in abduction and adduction, however, is limited. The head of the first metatarsal is camshaped and somewhat larger than the base of the proximal phalanx. Therefore, motion of this joint is more complex than that of a simple hinge, in that the center of rotation is dynamic. Fan-shaped ligaments originating from the medial and lateral epicondyles of the metatarsal head constitute the medial and lateral collateral ligaments responsible for static restraint to valgus and varus stress, respectively. Plantarly, the strong fibrocartilaginous plantar plate provides additional stability to the MTP joint. It is formed by the confluence of the plantar fascia and the plantar portion of the MTP joint capsule. The plantar plate attaches firmly to the base of the proximal phalanx, but only loosely at the plantar aspect of the metatarsal neck as part of the joint capsule. It is designed to withstand both tensile force in line with the plantar fascia as the MTP joint goes into dorsiflexion, and compressive force from the metatarsal head during weight bearing. The MTP joint capsule itself is a confluence of ligaments and tendons, including the collateral ligaments, the plantar plate, the metatarsosesamoid and phalangeosesamoid ligaments, the abductor and adductor hallucis (AH) muscles, the extensor digitorum brevis (EDB), and the flexor hallucis brevis (FHB).
in plantarflexion. Motion in abduction and adduction, however, is limited. The head of the first metatarsal is camshaped and somewhat larger than the base of the proximal phalanx. Therefore, motion of this joint is more complex than that of a simple hinge, in that the center of rotation is dynamic. Fan-shaped ligaments originating from the medial and lateral epicondyles of the metatarsal head constitute the medial and lateral collateral ligaments responsible for static restraint to valgus and varus stress, respectively. Plantarly, the strong fibrocartilaginous plantar plate provides additional stability to the MTP joint. It is formed by the confluence of the plantar fascia and the plantar portion of the MTP joint capsule. The plantar plate attaches firmly to the base of the proximal phalanx, but only loosely at the plantar aspect of the metatarsal neck as part of the joint capsule. It is designed to withstand both tensile force in line with the plantar fascia as the MTP joint goes into dorsiflexion, and compressive force from the metatarsal head during weight bearing. The MTP joint capsule itself is a confluence of ligaments and tendons, including the collateral ligaments, the plantar plate, the metatarsosesamoid and phalangeosesamoid ligaments, the abductor and adductor hallucis (AH) muscles, the extensor digitorum brevis (EDB), and the flexor hallucis brevis (FHB).
Two longitudinally oriented cartilage-covered grooves separated by a rounded ridge called the crista run along the plantar surface of the head. The FHB muscle consists of the medial and lateral portion each with a tendon insertion onto the plantar base of the proximal phalanx of the hallux. Contained in each tendon is a sesamoid bone that articulates with its respective overlying groove. The articulating surface of the sesamoid is also covered with hyaline cartilage. Interconnecting the two sesamoids is a thick intersesamoid ligament that maintains the relationship of the sesamoids and the proper course of the FHB tendons. The presence of these sesamoids gives the tendon a mechanical advantage when pulling at an angle (i.e., when the hallux is in a dorsiflexed position). Morphologically, the size and shape of the sesamoids vary widely. More than 10% of medial (or tibial) sesamoids are bipartite and should not be confused with a fracture. This finding is bilateral in 90% of cases and is seen far more commonly in the medial sesamoid than in the lateral (or fibular) sesamoid. The medial sesamoid can be divided into three or four parts as well, whereas the lateral sesamoid is rarely divided into more than two. The sesamoids are the attachment sites for a number of structures (Fig 1.4).
Lisfranc Joint
Separating the forefoot from the midfoot is the Lisfranc joint complex. The Lisfranc joint is composed of the five metatarsals articulating with the three cuneiforms and the cuboid. It is through this complex joint that the forefoot is attached to the midfoot.
Three columns are described in the foot:
Medial column, consisting of the first metatarsal and the medial cuneiform
Intermediate or middle column, consisting of the second and third metatarsals and the middle and lateral cuneiforms
Lateral column, consisting of the fourth and fifth metatarsals and the cuboid
Several factors contribute to the stability of the Lisfranc complex. The base of the second metatarsal is recessed between the medial and lateral cuneiforms and rigidly attached to the middle cuneiform (Fig 1.5). This configuration forms a “keystone” mortise, which adds stability in
the transverse plane. The relative immobility of the second ray coupled with the potential stress risers of the flanking medial and lateral cuneiforms are likely factors resulting in the characteristic stress fractures seen at the base of the second metatarsal in dancers. Stability in the coronal plane is enhanced by the arch configuration created by the trapezoidal shape of the cuneiforms and the second and third metatarsal bases (Fig 1.6). Furthermore, stability is further enhanced by the plantar and dorsal tarsometatarsal ligaments (the former being significantly stronger) and the plantar intermetatarsal ligaments. Because of the bony configuration and the strong plantar ligaments, the metatarsal bases are much more likely to displace dorsal than plantar. The second metatarsal, instead of being attached to the base of the first metatarsal, is secured to the medial cuneiform by Lisfranc ligament. This ligament is the strongest of the Lisfranc joint complex, has a relatively broad attachment on the plantar surface of the medial cuneiform, and runs obliquely to insert onto the plantar aspect of the base of the second metatarsal (Fig 1.7). Disruption of this complex can lead to an avulsion fracture of the base of the second metatarsal. The fragment, still attached to the Lisfranc ligament, can be seen on plain X-ray study (the Fleck sign).
the transverse plane. The relative immobility of the second ray coupled with the potential stress risers of the flanking medial and lateral cuneiforms are likely factors resulting in the characteristic stress fractures seen at the base of the second metatarsal in dancers. Stability in the coronal plane is enhanced by the arch configuration created by the trapezoidal shape of the cuneiforms and the second and third metatarsal bases (Fig 1.6). Furthermore, stability is further enhanced by the plantar and dorsal tarsometatarsal ligaments (the former being significantly stronger) and the plantar intermetatarsal ligaments. Because of the bony configuration and the strong plantar ligaments, the metatarsal bases are much more likely to displace dorsal than plantar. The second metatarsal, instead of being attached to the base of the first metatarsal, is secured to the medial cuneiform by Lisfranc ligament. This ligament is the strongest of the Lisfranc joint complex, has a relatively broad attachment on the plantar surface of the medial cuneiform, and runs obliquely to insert onto the plantar aspect of the base of the second metatarsal (Fig 1.7). Disruption of this complex can lead to an avulsion fracture of the base of the second metatarsal. The fragment, still attached to the Lisfranc ligament, can be seen on plain X-ray study (the Fleck sign).
 Figure 1.4 (A) Anatomy of the first metatarsophalangeal joint. (B) Plantar perspective. (C) Cross-sectional anatomy through the first metatarsophalangeal head. |
 Figure 1.5 Foot model demonstrating the recessed base of the second metatarsal between the medial and lateral cuneiforms. |
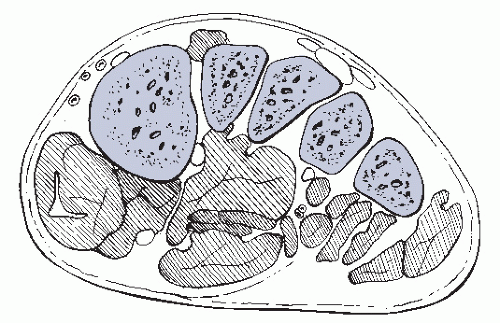 Figure 1.6 Wedge-shaped bases of the second and third metatarsals create a “keystone” effect that stabilizes the arch in the coronal plane. |
Midfoot
The five bones of the midfoot are relatively immobile with respect to one another. As a unit, they provide a mechanical link between the forefoot and the hindfoot. Furthermore, the midfoot provides protection for the passage of neurovascular structures as well as tendons from the ankle to the foot. The midfoot contains the navicular, the cuboid, and the three cuneiforms and extends from the tarsometatarsal (Lisfranc) joint distally to the transverse tarsal (Chopart) joint proximally.
The navicular has a concave posterior surface where it articulates with the talus and a convex anterior surface, divided into three facets, where it articulates with each of the three cuneiforms. The medial portion possesses a tuberosity that is the main insertion site of the posterior tibial tendon. The plantar surface provides the attachment sites for the superomedial calcaneonavicular ligament and the inferior calcaneonavicular ligament (spring ligament complex). The superomedial component of the spring ligament also attaches medially directly deep to the posterior tibial tendon. The dorsal surface provides attachments for a number of ligaments including the talonavicular ligament, the
dorsal cuneonavicular ligaments, and the dorsal cuboideonavicular ligaments. The dorsal surface receives the medial slip of the bifurcate ligament (calcaneonavicular part), a strong Y-shaped ligament arising from the superior aspect of the anterior process of the calcaneus.
dorsal cuneonavicular ligaments, and the dorsal cuboideonavicular ligaments. The dorsal surface receives the medial slip of the bifurcate ligament (calcaneonavicular part), a strong Y-shaped ligament arising from the superior aspect of the anterior process of the calcaneus.
The navicular is largely responsible for transmitting forces from the hindfoot to the forefoot. For this reason and because there is a relatively poor blood supply to its central third, it is subject to stress fractures and avascular necrosis. Furthermore, the talonavicular joint is most susceptible to non-union after a triple arthrodesis (talonavicular, calcaneocuboid, and subtalar joints).
The cuboid is part of the lateral column of the foot, positioned between the anterior surface of the calcaneus and the bases of the fourth and fifth metatarsals. Posteriorly, it forms a saddle-shaped joint with the calcaneus. Anteriorly, two facets separated by a slight ridge allow a mobile articulation with the base of the fourth and fifth metatarsals. The medial surface has an articulating surface for the lateral cuneiform and sometimes for the navicular. The cuboid is stabilized to the calcaneus dorsally by the lateral slip of the bifurcate ligament (from the calcaneus) and the dorsal calcaneocuboid ligament. Plantar stabilizing structures include the plantar calcaneocuboid ligament (short plantar ligament) and the deep fibers of the long plantar ligament. A groove (or sulcus) is found on the plantar aspect of the cuboid. The superficial fibers of the long plantar ligament, on their way to the second, third, and fourth metatarsal bases, pass over the peroneal groove, converting it to a fibroosseous canal (cuboid tunnel) through which the peroneus longus (PL) tendon passes.
The cuneiforms articulate with the navicular posteriorly and their respective metatarsals anteriorly. The medial cuneiform is the largest of the three and is oriented with the thin edge of its wedge shape pointing dorsally. It also serves as the partial insertion site for several tendons including the PL, the posterior tibial tendon, and the anterior tibial tendon, as well as Lisfranc ligament.
The middle and lateral cuneiforms are rigidly attached to the bases of the second and third metatarsals, respectively. These wedge-shaped bones fit like the stones of a Roman arch to provide the inherent bony stability to the medial longitudinal arch of the foot. Slips from the posterior tibial tendon find attachment sites on the plantar surfaces of both bones.
Transverse Tarsal Joint (Chopart Joint)
The midfoot is separated from the hindfoot by the transverse tarsal joint (Chopart joint), which includes the talonavicular and calcaneocuboid joints.
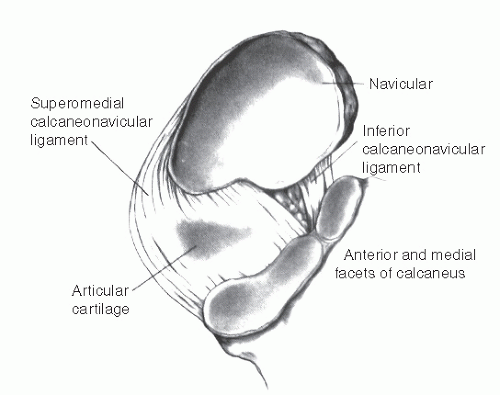
The talonavicular joint is a ball-and-socket type joint that is the key part of a complex motion system called the acetabulum pedis. The acetabulum pedis is a deep socket that receives the head of the talus formed by the navicular, the anterior and middle facets of the calcaneus, the superomedial and inferior calcaneonavicular ligaments (spring ligament complex), and the calcaneonavicular slip of the bifurcate ligament (Fig 1.8). In conjunction with the calcaneocuboid joint, the acetabulum pedis allows motion in both the longitudinal and transverse planes. These motions contribute to the shock-absorbing ability and the stability of the foot during weight bearing. Additionally, it allows for appropriate alignment between the forefoot and hindfoot when walking on uneven terrain.
The spring ligament complex consists of three anatomic components: the superomedial calcaneonavicular ligament (the largest and strongest portion of the spring ligament complex), the inferior (or plantar) calcaneonavicular ligament, and the third ligament. The superomedial component includes the medial talonavicular capsule and is confluent with the tibionavicular portion of the superficial deltoid ligament. It is triangular in shape and contains fibrocartilage as a result of its articulation with the talar head. The superficial fibers of the superomedial calcaneonavicular ligament have additional attachments to the posterior tibial tendon. The inferior calcaneonavicular ligament is a narrower, entirely fibrous structure that lies in the plantar-most aspect of the acetabulum pedis. The third ligament is distinct from the superomedial calcaneonavicular ligament. It originales from the notch between the anterior and middle facets of the calcaneus and attaches to the navicular tuberosity. The spring ligament complex, particularly the superomedial component, is considered the primary static restraint to deformity of the talonavicular joint. Insufficiency of this ligament is a major contributing factor to adult acquired flatfoot deformity.
Any motion of the talonavicular joint or subtalar joint must involve the calcaneocuboid joint. The anterior calcaneal articular surface is concave vertically and convex transversely. The posterior aspect of the cuboid features a reciprocal undulating surface. Congruency of the two opposing surfaces is at a maximum when the heel is in varus and the forefoot supinated, which is the position of the foot during pushoff.
Hindfoot
The hindfoot contains the calcaneus (os calcis) and the talus. The calcaneus is the largest tarsal bone and forms the heel of the foot. Its complicated shape has six surfaces:
The superior aspect articulates with the talus via three articular surfaces (the anterior, middle, and posterior facets).
The anterior surface articulates with the cuboid.
The posterior surface is the insertion site of the Achilles tendon.
The medial surface has a bony shelf called the sustentaculum tali, which supports a part of the talar head through the middle facet and is the attachment site to a number of ligaments.
The lateral surface features a bony prominence called the peroneal tubercle, which separates the PL and peroneus brevis (PB) tendon.
The inferior surface is the major weight-bearing surface for the hindfoot, which serves as an attachment site for the plantar fascia and a number of intrinsic muscles and ligaments.
The talus is the second largest tarsal bone and is divided into three regions: the head, neck, and body. The neck of the talus connects the body to the head. The neck projects anteriorly, plantarward, and medially from the body, which is important to realize for reconstruction after fracture. The sulcus tali is a deep groove on the inferior portion of the neck oriented obliquely in an anterolateral, to posteromedial direction. Where the talus articulates with the superior surface of the calcaneus, the sulcus tali aligns with a corresponding groove (sulcus calcanei) to form a bony canal called the sinus tarsi. Attached to the sulcus tali and inserting onto the sulcus calcanei is the strong bilaminar interosseous talocalcaneal ligament.
Most of the talar body is covered with articular cartilage. Superiorly it articulates with the tibial plafond, and medially and laterally with the respective malleoli. Inferiorly, it articulates with the posterior facet of the calcaneus.
Almost the entire head of the talus is covered with articular cartilage. It articulates with the tarsal navicular anteriorly and the anterior and middle facets of the calcaneus inferiorly.
The posterior aspect of the talus has two bony prominences: the medial and lateral talar tubercles, between which passes the flexor hallucis longus (FHL) tendon. The lateral tubercle is more prominent and may ossify separately from the rest of the talus, forming an accessory ossicle called the os trigonum. It is the second most common accessory bone of the foot and may play a role in posterior ankle impingement syndromes. The lateral talar tubercle can fracture (Shepherd fracture) and mimic an os trigonum.
The lateral talar process is a bony projection located inferiorly on the lateral surface of the talus. Its underlying surface articulates with the posterior articular surface of the calcaneus. This process can fracture (snowboarder’s fracture) and is part of the differential diagnosis for lateral ankle pain.
The talus has no tendon or muscle insertions or origins.
Subtalar Joint
The subtalar joint is the articulation of the inferior surface of the talus as it sits “sidesaddle” medially over the superior surface of the calcaneus. This articulation consists of three facets: an anterior facet located on the superomedial aspect of the anterior process, a middle facet on the sustentaculum tali, and a posterior facet, which is the largest of the three. The anterior and middle facets are often one contiguous joint surface. A groove in the calcaneus which separates the anterior and middle facets from the posterior facet forms the floor of the sinus tarsi. The anterior process may be involved in a congenital anomaly whereby it is joined to the lateral aspect of navicular by a fibrous or bony bridge (calcaneonavicular tarsal coalition). Similarly, a coalition may occur in the middle facet (talocalcaneal tarsal coalition). These account for more than 90% of all tarsal coalitions and occur with almost equal frequency.
The deltoid ligament, the calcaneofibular ligament (CFL), the lateral talocalcaneal ligament (LTCL), the cervical ligament (CL), the interosseous ligament (IO), and the inferior extensor retinaculum (IER) stabilize the subtalar joint. The lateral structures have been categorized as superficial, intermediate, and deep (Fig 1.9 and Box 1.1). With progressive inversion of the heel, the lateral ligaments rupture in the following order: CFL, LTCL, and then the IO. The role of the CFL as primary lateral stabilizer of the subtalar joint is a matter of some debate. The orientation of its fibers as well as other anatomic variations (e.g., the LTCL is absent in more than 40%) in this region either contribute to or detract from its role. Subtalar joint range of motion is estimated to be 24°; however, there is wide variability among the population and it is difficult to measure clinically. Furthermore, what constitutes laxity or instability is not clearly defined. One study demonstrated that sectioning the CL or the IO increased subtalar motion a maximum of 2.6°. Because the range of subtalar motion is small to begin with, this increase may be significant,
clinically manifesting as symptoms of instability or sinus tarsi syndrome.
clinically manifesting as symptoms of instability or sinus tarsi syndrome.
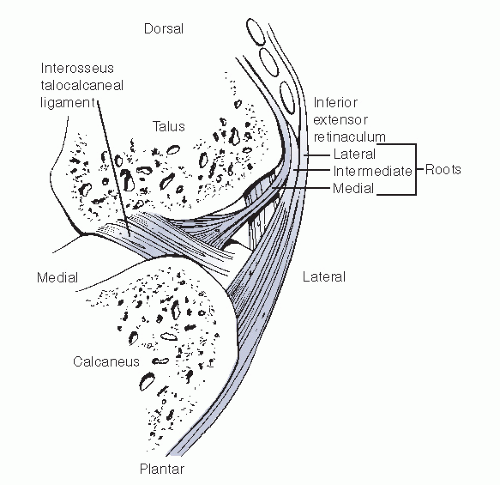 Figure 1.9 Lateral stabilizers of the subtalar joint. (Adapted from Harper MC. The lateral ligamentous support of the subtalar joint. Foot Ankle Int 1991;11:354-358.) |
BOX 1.1 LATERAL LIGAMENTOUS SUPPORT OF THE SUBTALAR JOINT
Superficial Layer
Lateral root of the inferior retinaculum Lateral talocalcaneal ligament Calcaneofibular ligament
Intermediate Layer
Intermediate root of the inferior retinaculum Cervical ligament
Deep Layer
Medial root of the inferior retinaculum Interosseous talocalcaneal ligament
From Harper MC. The lateral ligamentous support of the subtalar joint. Foot Ankle Int 1991;11:354-358.
Ankle Joint
The body (or dome) of the talus resides in an articulation created by the distal tibia and fibula. This mortise is formed by the tibial plafond (flat roof) or pilon superiorly and the medial and lateral malleoli. The posterior flare of the distal tibial metaphysis is often referred to as the posterior malleolus. The medial malleolus is the distal-most extension of the tibia and is divided by a longitudinal groove into a small anterior and larger posterior colliculus. The inner surface is lined with hyaline cartilage and articulates with the medial aspect of the talus. In a similar fashion, the distal-most aspect of the fibula articulates with the lateral portion of the talus. More proximally, the fibula is set in a tibial recess posterolaterally. The ligaments of the ankle are divided into three groups: syndesmotic ligaments, lateral ligaments, and medial ligaments.
Tibiotalar Syndesmosis
The syndesmosis, located at the level of the tibial plafond, maintains the relationship between the fibula and tibia and comprises four ligaments:
anterior inferior tibiofibular ligament (AITFL)
posterior inferior tibiofibular ligament (PITFL)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree