3.2 The cardiovascular system
Chapter 3.2a The physiology of the cardiovascular system
At the end of this chapter you will be able to:
Estimated time for chapter: Part I, 60 minutes; Part II, 60 minutes.
Introduction
This section of Stage 3 focuses on the cardiovascular system, also known as the ‘circulatory system’. Like Chapter 3.1a, this chapter is divided into two parts. If you are using this book as a study course, then, because of its length, you are advised to work through the two sections of this chapter in separate study sessions.
Part I – The vessels and the heart organ
Sometimes the lymphatic system first referred to in Chapter 2.1d, is also included as part of the cardiovascular system. However, in this book, for the sake of clarity, the lymphatic system is treated as a separate system.
The blood (haematological system) is not conventionally considered to be a part of the cardiovascular system. The blood is described in Section 3.4.
The blood vessels
Arteries
One important disease of arteries, arterial thrombosis, has already been described in this text (Chapter 2.2d).
Veins
One important potentially life-threatening venous disease, deep vein thrombosis, has already been described (Chapter 2.2d). The more common and benign condition of varicose veins is described later in this section (Chapter 3.2d).
The transfer of nutrients from capillaries to the tissues
Healthy blood that has just passed through the digestive system will contain a high concentration of basic nutrients, including simple sugars, cholesterol, triglycerides, fatty acids, amino acids from proteins, vitamins and minerals (see Chapter 3.1a for a reminder of the origin of the basic nutrients and how they are processed by the digestive system). Once the blood has passed through the capillaries of the lungs, it will also contain a high concentration of oxygen. Chapter 1.1b explained how oxygen is one of the essential ingredients which, together with glucose and other simple nutrients, is used by the mitochondria of every cell in the body to produce the energy required for many vital cellular processes.
The body relies on the transport processes of diffusion, osmosis and active transport for nutrients and oxygen to enter the bloodstream from the tissues of the digestive system and the lung. These processes are described in detail in Chapter 1.1c.
It is worth remembering for the present that just under half of the volume of the blood is made up of blood cells that are too large to move between the gaps in the capillaries. A good proportion of the composition of the remaining plasma consists of dissolved protein molecules, which are also too large to pass through the gaps in the capillaries. Therefore, the movement of fluid across capillary membranes is selective for the remaining small molecules, such as water itself, salt and sugars. This is the property of semipermeability, as first described in Chapter 1.1c.
An understanding of these forces that affect the movement of fluid between the blood and the tissues is a helpful foundation for the study of the important condition of oedema, which is described in Chapter 3.2f (see Q3.2a-3) .
.
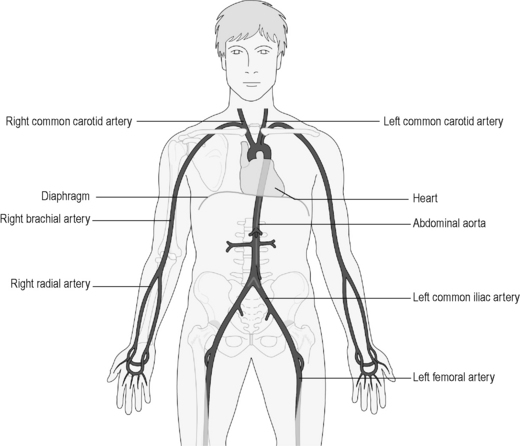
The pathway of the arteries
Figure 3.2a-I illustrates the pathway of the major arteries that lead away from the heart. The diagram shows how the blood is directed from the heart to all parts of the body. The arch of the largest blood vessel in the body, the aorta, is shown leaving the top of the heart and then descending to run deep in the body, through the diaphragm to the pelvis. Here, it splits into two main branches, which supply blood to each leg.
Figure 3.2a.II shows how the major branches of the aorta in the neck, the common carotid arteries, branch to supply blood to the head. One branch, the internal carotid artery, divides to enter the skull and supply the brain with blood (see Q3.2a-6) .
.
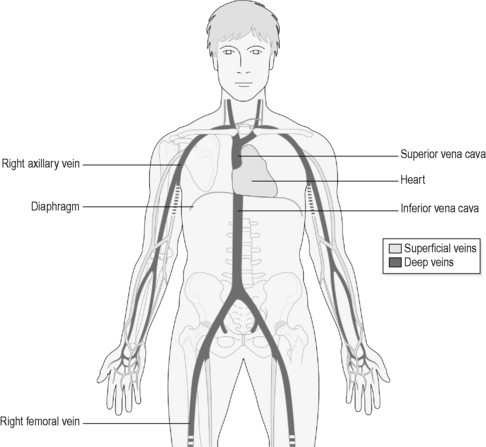
Now turn back to Figure 3.2a-I, which shows how arterial branches from the aorta divide down each limb to take blood to the hands and the feet. Compare this with Figure 3.2a-III, which shows the pathways of the veins that return the blood to the heart, ending in two major vessels called the ‘superior vena cava’ and ‘inferior vena cava’. Note how the basic pathways of the veins mirror those of the arteries. This is the pattern for almost all parts of the body, in that an artery delivering blood to a body part runs very close to the vein that is draining the blood away from that part.
In addition to superficial veins, there is also a system of ‘deep veins’. The blood draining from the surface of the body runs first into the superficial veins, and then enters the deep veins through vessels that penetrate the deeper tissues called ‘perforators‘. It is important to be clear about the distinction between superficial and deep veins in order to understand the pathology of the condition of varicose veins, described in Chapter 3.2c.
The structure of the heart
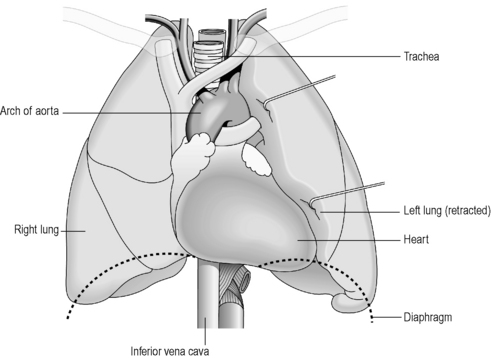
The heart is a fist-sized organ that sits just to the left of midline in the chest (see Figure 3.2a-I). It is situated between the two lungs, and together these organs fill the space that overlies the diaphragm (the thoracic cavity; Figure 3.2a-IV). These organs are so closely related that the inside surfaces of the lungs bears the impression of the shape of the heart upon them.
The heart is largely made up of cardiac muscle (the myocardium), and is divided into four chambers. It might be helpful now to turn back to the description of the tissue types given in Chapter 1.2d for a reminder of the characteristics of cardiac muscle, and how the cardiac muscle cells communicate with each other through specialised ‘joints’ (see Q3.2a-7) .
.
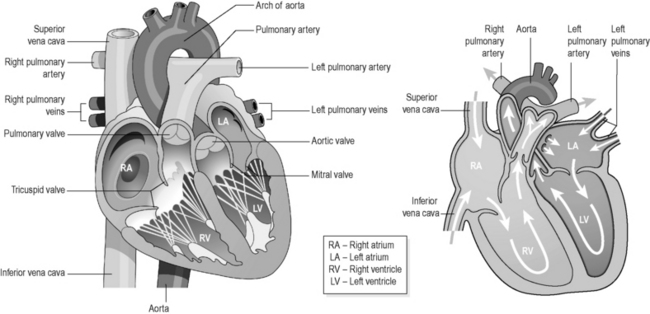
To understand the action and some of the structural disorders of the heart, it is important to understand that the heart is divided into two halves: the right half deals with the flow of the blood from the body and to the lungs, and the left half deals with the flow of the blood from the lungs and to the body. Each half has two chambers known as the ‘atria’ (plural of ‘atrium’) and the ‘ventricles’, and together these form the four chambers of the heart. There are two valves situated in each half of the heart. Their function is to ensure that the blood flow is always one way. Figure 3.2a-V illustrates the position and shape of the four chambers and the valves of the heart, and the direction of blood flow through the two halves of the heart.
The flow of blood through the heart
The double structure of the heart means that blood can flow through the heart twice in each full circulation of the body. It might help when reading the following description of the flow of the blood to use Figure 3.2a-V to visually trace the pathway the blood takes.
The flow of blood through the left side of the heart
When blood has passed though the capillary network of the lungs, it has given up its carbon dioxide and is rich in oxygen, all through the effortless process of diffusion (see Chapter 3.3a for more detail about the structure of the blood vessels in the lungs). This oxygen-rich blood is a brighter shade of red than the darker venous blood. It flows through the pulmonary vein and into the left atrium of the heart. The left atrium contracts to force the blood through the mitral valve, and thus into the muscular left ventricle. The left ventricle then contracts, and this forces the blood through the aortic valve into the arch of the aorta, the widest part of the widest blood vessel in the body. The pressure of the blood in the contracting right ventricle closes the mitral valve, also making a subtle clapping noise. Just as was described for blood leaving the right ventricle, blood rushing into the aorta does not flow back into the left ventricle when it finishes its contraction. This is because the aortic valve also closes in turn, making its own clapping noise as it does so.
• oxygenated blood from the lungs enters the left heart
• the left heart pumps oxygenated blood to all the tissues of the body
• tissues absorb oxygen so that the blood becomes deoxygenated
• deoxygenated blood from the body returns to the right heart
• the right heart pumps deoxygenated blood to the lungs
• blood absorbs oxygen from the lungs so that it becomes oxygenated
• oxygenated blood from the lungs enters the left heart … and so on (see Q3.2a-9) .
.
The blood supply to the heart
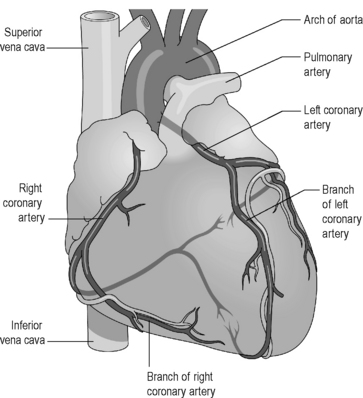
Figure 3.2a-VI illustrates how vessels, known as the ‘coronary arteries’ (‘cor’ is the Latin root meaning ‘heart’), branch from their origin at the aorta to wrap around the heart muscle. An understanding of this blood supply will be good preparation for the study of coronary heart disease (Chapter 3.2e) which is the most important cause of death, after cancer, in developed countries.
Part II – The blood pressure and the Chinese medical view
The blood pressure
Adequate blood pressure is essential to ensure a steady flow of nutrients to all parts of the body. In times of physical stress the blood pressure rises, but this is appropriate to the body’s needs. It is only if the blood pressure remains at too high a level for the body’s requirements for too long that long-term damage to the circulatory system can occur. The condition of high blood pressure (hypertension) is explored in more detail in Chapter 3.2d.
Control of blood pressure
Two of the many chemicals that are integral to the activation of the SNS are the hormones adrenaline and noradrenaline. A release of adrenaline from the adrenal glands will lead to an increased heart rate, constriction of the artery walls and an increase in blood pressure. This is explained in more detail in Section 5.1 (see Q3.2a-13) .
.
Measurement of blood pressure
 Information Box 3.2a-II The heart and pericardium: comments from a Chinese medicine perspective
Information Box 3.2a-II The heart and pericardium: comments from a Chinese medicine perspective
The functions of the Heart according to a conventional and Chinese perspective can be summarised in the form of a correspondence table (for an introduction to the Organ correspondence tables, see Appendix I). This table illustrates the idea that the functions of the fleshy pump, which conventional medicine calls the heart, may be the domain of not only the Heart Organ in Chinese Medicine, but also the Kidney and Liver Organs. It will follow from this that diseases of the conventionally viewed cardiovascular system may manifest in Chinese medicine syndromes involving the Heart, Kidney and Liver Organs.
Correspondence table for the functions of the Heart as described by conventional and Chinese medicine
| Functions of the heart | Functions of the Heart Organ1 |
|---|---|
• Acts as a pulsatile pump to enable circulation of the blood (Heart and Liver Organs) • The origin of the heart muscle impulse (the pacemaker) (Heart Organ) • Contributes to the maintenance of blood pressure (Heart Organ and Kidney Yang) • Will respond to bodily requirements by an alteration in the strength and rate of pumping (Heart Organ and Kidney Yang) | ‘The Heart is like the monarch and it governs the mind’ |
1 Maciocia G 1989 The foundations of Chinese medicine. Churchill Livingstone, Edinburgh.
Correspondence table for the functions of the Pericardium as described by conventional and Chinese medicine
| Functions of the pericardium | Functions of the Pericardium1 |
|---|---|
| • It is a fibrous membrane that surrounds the heart and allows its free movement. It also protects from mechanical injury. The serous fluid it encloses contains protective antibodies and immune cells (Heart, Liver and Kidney Organs) | ‘The Pericardium is an ambassador and from it joy and happiness derive’ • Like the Heart it governs blood (bone marrow, heart, blood vessels) • Like the Heart it houses the mind (brain) • Together with the Kidneys and Triple Burner Organs it has been associated with the Gate of Vitality (Ming Men) (possibly the healthy function of the metabolic processes that go on in all the cells and particularly the sympathetic nervous system) |
1 Maciocia G 1989 The foundations of Chinese medicine. Churchill Livingstone, Edinburgh.
 Self-test 3.2a The physiology of the cardiovascular system
Self-test 3.2a The physiology of the cardiovascular system
1. What are the broad differences between arteries and veins?
2. How does the structure of capillaries suit their function?
3. Why do you think the circulation flows as a figure-of-eight, with the heart at the cross of the eight shape?
4. What do you think might be the result if one of the three major coronary arteries suddenly becomes blocked by a thrombosis?
5. How do you think a coronary artery thrombosis might affect the conduction system of the heart?
6. Why is it recommended to take the blood pressure in a patient who has been resting for at least 5 minutes?
Answers
1. Arteries are the vessels that carry blood away from the heart. They contain muscle and elastin in their walls and carry blood under high pressure. They can alter in width to control the blood flow within them. They tend to run at a deeper level than veins.
2. Capillaries have a single-celled endothelial wall that permits ready exchange of substances by diffusion. This allows the passage of nutrients, such as oxygen, saccharides and amino acids, from the blood into the tissues, and the passage of wastes, such as carbon dioxide, from the tissues back into the blood. The complex branched structure of capillaries enables blood to be circulated very close to the diverse cells throughout the body.
3. The figure-of-eight shape has two loops: one loop is the circulation through the lungs, also known as the pulmonary circulation. The other is the circulation through the rest of the body, also known as the systemic circulation. The double pumping action of the heart ensures that blood flows evenly through this double loop. In this way, all deoxygenated blood arriving at the heart from the body is passed through the lungs to be reoxygenated before it returns to the body tissues.
4. A sudden occlusion of a coronary artery will lead to an infarction of the heart muscle supplied by that artery. Because the heart has a high demand for nutrients and oxygen, an infarction can develop rapidly within a few hours, but will have the red flags of severe cramping pain developing seconds after the occlusion. This of course is the mechanism of a heart attack (also known as a ‘myocardial infarction’).
5. The infarction due to a coronary thrombosis can lead to disturbance or death of the cardiac muscle fibres, which are central to the conduction system of the heart. If this occurs, a patient having a heart attack may suffer from an irregular heartbeat, or even cardiac arrest (cessation of adequate pumping action of the heart).
6. It is known that both exercise and emotional stress can cause the blood pressure to be raised. If this is a temporary response, as long as the pressure not too high, then it is considered an appropriate bodily response. Taking the blood pressure under these conditions might give a misleadingly high reading.
Chapter 3.2b The investigation of the cardiovascular system
The investigation of the vessels and circulation
The investigation of the vessels and circulation includes:
• a thorough physical examination
• Doppler assessment of the blood flow in the vessels
• tests such as a Doppler ultrasound scan and angiography to visualise the vessels in the thorax, abdomen, pelvis and legs.
These investigations are now considered briefly in turn.
Physical examination of the vessels and circulation
The physical examination of the vessels and circulation involves the stages listed in Table 3.2b-I (see Q3.2b-1) .
.
Table 3.2b-I The stages of the physical examination of the blood vessels and circulation
Blood tests
Blood tests can be performed to exclude certain conditions that can contribute to disease of the vessels. The most common tests to be performed are serum tests to check for raised blood lipids (such as cholesterol) and glucose (indicative of diabetes). The erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) (see Chapter 2.4d) may be measured to exclude the rare inflammatory conditions that may affect the blood vessels. A full blood count (FBC) is performed to exclude anaemia, because in anaemia the oxygen-carrying capacity of the blood is markedly reduced and this can worsen the symptoms of vascular disease. For this reason, it is important to diagnose and treat anaemia in someone with disease of the blood vessels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 .
. .
. .
.
 Information Box 3.2a-I
Information Box 3.2a-I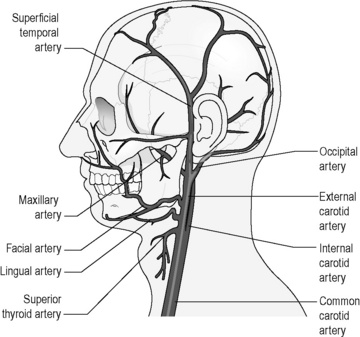
 .
.
 .
. .
. .
.
