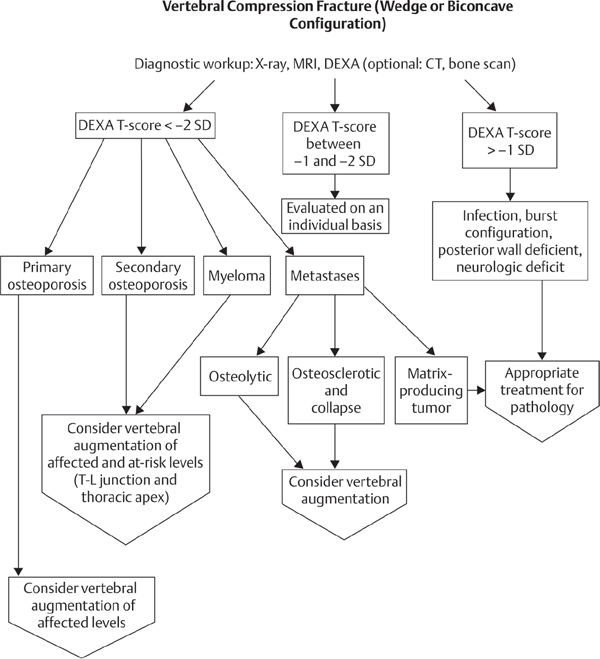
53 Within the next decade, spine surgeons will encounter an increasing number of patients with osteopenia/osteoporosis requiring surgical intervention for spinal disorders as the longevity of the general population increases. The patient with osteoporosis poses a considerable challenge for spine surgeons, with issues including frequent preoperative medical comorbidities and suboptimal nutrition to intraoperative and postoperative concerns regarding poor bone quality leading to hardware cutout and failure. Similarly, postoperative adherence to rigorous physical therapy protocols is unlikely in this patient population. As in a younger cohort of surgical spine patients, indications for surgery in the elderly continue to be neurogenic claudication, radiculopathy, myelopathy, mechanical back pain, progressive spinal deformity with or without vertebral fractures, or any combination of these findings. That said, a serious discussion with the patient and caregiver must be undertaken when a reasonable course of nonoperative care is feasible prior to surgical intervention in this high-risk population. Once nonoperative management has been exhausted and the patient has been medically cleared for the physiologic challenge of spine surgery, direct decompression of the involved neural elements remains the mainstay of treatment for spinal stenosis that gives rise to claudication and/or myeloradiculopathy. When diffuse multilevel spinal degenerative changes are present, it is helpful if the symptoms can be isolated to a particular spinal level or nerve root, thus allowing for a limited decompressive procedure and obviating the need for large, multilevel procedures. If indicated, a concomitant arthrodesis may be considered in the presence of deformity or preexisting instability or when surgical decompression creates instability as a result of excessive bony resection, as in a complete facetectomy or pars resection. Limited in situ fusion for instability or deformity may be effective without instrumentation when the risk of progressive deformity is minimal. Often, segmental instrumentation is necessary to correct deformity and to stabilize the destabilized spine. Such a construct must be able to withstand the three-dimensional forces across the area of fixation until fusion is complete. Pedicle screw instrumentation enables segmental control of all three columns of the spine from a posterior approach alone. The implant–bone interface remains the weak link in the instrumentation construct in the osteoporotic spine. The majority of instrumentation failures involve screw loosening and pullout, which may lead to failure of fusion or the development of recurrent or de novo deformity. Inserting larger-diameter pedicle screws and undertapping may enhance screw stability. Triangulating the screws in the axial plane to increase posterior pullout strength and diverging the screws in the sagittal plane to increase axial load-bearing capacity are important. Increasing screw length and diameter does increase screw pullout strength, although this effect may be less pronounced in osteoporotic bone. Precoating pedicle screws with hydroxyapatite has been shown to reduce the incidence of screw cutout significantly in preclinical and clinical series. At the sacrum, medially directed, triangulated bicortical purchase aiming toward the promontory may protect against distal construct failure. In certain instances, purchase within the ilium may be necessary, especially in long fusion constructs for deformity. Another strategy to improve construct rigidity in osteoporotic bone is to increase the number of levels instrumented. This approach must be weighed against the morbidity of the additional level surgery as well as the potential for junctional breakdown in the future. Several studies have indicated that the bone–screw interface may be improved by injecting bone cement (polymethylmethacrylate, PMMA) into the pedicle at the time of screw insertion. A two- to threefold increase in screw pullout resistance has been demonstrated with the use of bone cement injected into the vertebral body through a specially designed fenestrated-cannulated pedicle. Bioactive cements such as calcium phosphate and carbonated apatite have also been shown to contribute to the screw–bone interface and increase pedicle screw pullout strength. The surgeon may also augment the pedicle screw construct with offset sublaminar hooks or wires that are well suited for use in the osteoporotic spine by relying on the relatively spared cortical laminar bone for fixation. Another approach in reconstruction for the patient with osteopenic deformity is to utilize both the anterior and posterior column for support at a given level. Anterior devices may function to share load that would otherwise be concentrated on posterior pedicle screw or hook constructs. In general, anteriorly placed metallic interbody devices have a modulus mismatch with bone and tend to subside in osteopenic bone. Since the cortical rim is the strongest part of the vertebral body in axial loading, the graft or implant should have a wide footprint and engage as much of the rim circumference as possible. The potential benefit to use of interbody load-sharing devices must be carefully weighed against increased surgical time, risk, and morbidity associated with their use. Consideration may be given to staging such patients for an anterior release/reconstruction prior to tackling the posterior fusion construct. Segmental deformity correction with the use of posterior-based osteotomies may correct sagittal balance and indirectly minimize the stresses borne by instrumentation. Modest correction can be obtained using the Smith-Petersen osteotomy, and a greater correction can be obtained with the pedicle subtraction osteotomy. Accepting a lesser degree of deformity correction when full spinal balance cannot be achieved is an alternative to avoid implant overload and subsequent instrumentation failure. Such procedures severely stress the physiologic baseline of these patients and must be approached with caution. Outcomes in these patients can be optimized with a careful, well-thought-out surgical plan with appropriate decompression and judicious use of fusion with or without instrumentation to achieve the goals of surgery, including pain relief, improved physical function, and restoration of spinal alignment. Perioperative complications have been shown to occur with significantly greater frequency in patients older than 60, prolonging the postoperative recovery time to 6 months or longer in this population. Intraoperative and early postoperative surgical complications include neurologic injury, durotomy, infection, wound breakdown, and failure of fixation. Coexistent medical comorbidities, leading to prolonged intubation and intensive care unit (ICU) stay, are not uncommon in these patients. Complications for which patients with osteoporosis are specifically at risk include instrumentation failure, progression of deformity, and adjacent-level compression fracture. These complications are best avoided by meticulous surgical planning and an understanding of the capabilities of the instrumentation as well as of the biomechanical environment across which the instrumentation is applied. Albert TJ, Purtill J, Mesa J, McIntosh T, Balderston RA. Health outcome assessment before and after adult deformity surgery. A prospective study. Spine 1995;20(18):2002–2004, discussion 2005 PubMed This excellent article details health outcome analysis before and after adult deformity surgery. This chapter discusses the indications and techniques of kyphotic deformity correction using the pedicle subtraction and Smith-Petersen osteotomies. It also considers the complications and results of these osteotomies. Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br 2010;92(8):1061–1065 PubMed This excellent recent review focuses on the biomechanics of pedicle screw instrumentation and cross-connectors in challenging clinical scenarios. Chao EY, Inoue N, Koo TK, Kim YH. Biomechanical considerations of fracture treatment and bone quality maintenance in elderly patients and patients with osteoporosis. Clin Orthop Relat Res 2004; (425):12–25 PubMed An excellent overview of nonsurgical management of osteoporosis and the biomechanics of fixation in the osteoporotic spine. Andersson GBJ, Weinstein JN. Focus issue on osteoporosis. Spine 1997;22(24 Supplement) This issue presents an excellent compendium of articles on the medical management of osteoporosis and provides a framework for surgical management of the osteoporotic spine. Hu SS. Internal fixation in the osteoporotic spine. Spine 1997;22(24, Suppl):43S–48S PubMed This article provides a thorough discussion of biomechanical and patient factors to be considered along with surgical techniques and principles to improve fixation in the osteoporotic spine, including bailout and revision strategies. Manson NA, Phillips FM. Minimally invasive techniques for the treatment of osteoporotic vertebral fractures. J Bone Joint Surg Am 2006;88(8):1862–1872 PubMed Review of the current minimally invasive modalities for the treatment of osteoporotic vertebral compression fractures. CT, computed tomography; DEXA, dual-energy X-ray absorptionmetry; MRI, magnetic resonance imaging; SD, standard deviation; T-L, thoracocolumbar
Surgical Treatment of the Osteopenic Patient
![]() Surgical Indications
Surgical Indications
![]() Treatment
Treatment
![]() Outcomes
Outcomes
![]() Complications
Complications
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







