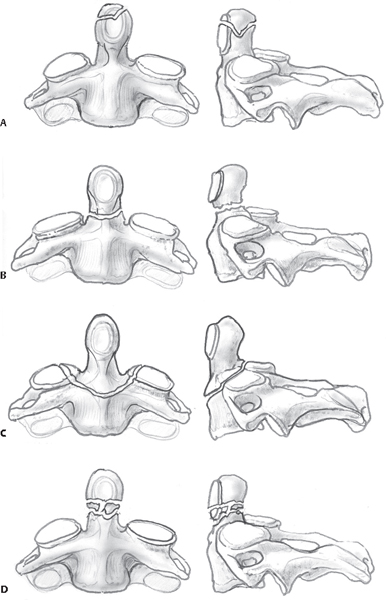
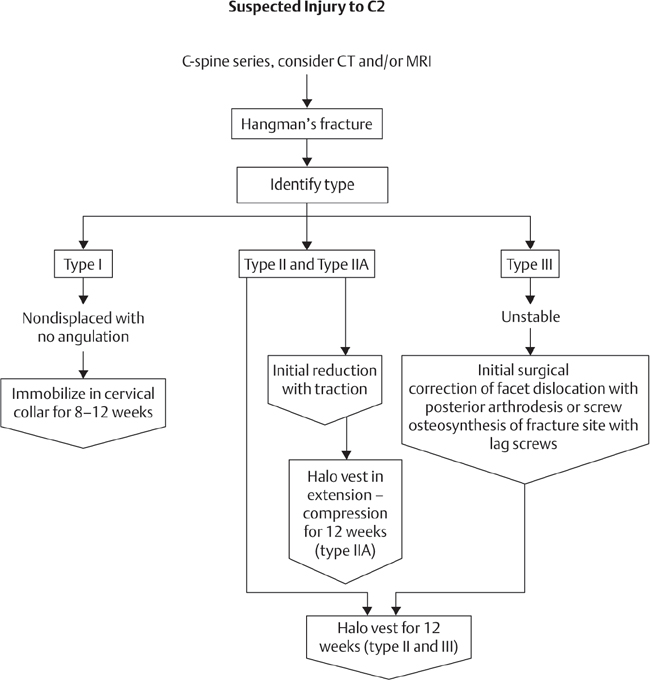
4 Odontoid fractures are the most common cervical spine fracture in the elderly, and their incidence is increasing.1 The odontoid process of C2 serves as a peg on which the C1 ring rotates: sixty degrees of axial rotation occurs at the C1–C2 articulation.2 Anterior translation of C1 relative to C2 is prevented primarily by the transverse ligament and secondarily by the alar and apical ligaments. Posterior translation is prevented by the odontoid articulation against the anterior arch of C1. Fractures of the odontoid may result in instability because the C1–odontoid complex can translate relative to the body of C2. Because of the capacious nature of the spinal canal in the upper cervical spine, odontoid fractures are rarely associated with an acute neurological deficit. However, in the setting of chronic instability due to an odontoid nonunion, late-onset myelopathy has been observed.3 Anderson and D’Alonzo4 described the most commonly used classification system for odontoid fractures (Fig. 4.1). Type I fractures represent a fracture of the tip of the odontoid, cephalad to the transverse ligament. Type II fractures denote a fracture through the base of the dens but not involving the body of C2, while Type III fractures extend into the body of C2. It has been noted that there is relatively poor inter-observer agreement in differentiating Type II and Type III fractures.5 Grauer et al.6 suggested modifying the Anderson classification to consider fracture displacement, obliquity, and comminution. This modification also further distinguishes between Type II and III fractures, with Type III fractures defined as those involving the C2 superior articular facet. Fig. 4.1 Anderson and D’Alonzo classification system illustrating (A) Type I, (B) Type II, and (C) Type III odontoid fractures. Note the subset (D) IIA added by Haley, which denotes comminution. (From Stannard et al., Surgical Treatment of Orthopaedic Trauma. Thieme, NY. 2006. Reprinted with permission.) The incidence of odontoid fractures has a bimodal age distribution: younger patients have predominantly high-energy mechanisms, whereas older patients generally present with low-energy mechanisms, such as falls from standing. When evaluating an elderly patient with a history of repeated falls, one must consider the possibility of a chronic fracture. Anteroposterior (AP), lateral, and open-mouth odontoid views should be routinely obtained in the setting of a suspected fracture. If a fracture is identified or cannot be excluded, a computed tomography (CT) scan with sagittal and coronal reconstructions should be obtained to aid with fracture classification and treatment planning. Odontoid fractures are associated with other cervical fractures, such as C1 arch fractures, and the clinician must carefully evaluate the entire cervical spine on CT scan. If the fracture involves the foramen transversarium, magnetic resonance (MR) angiography should be considered to assess the vertebral artery. The presence of a neurological deficit is an absolute indication to obtain MR imaging (MRI). An MRI should also be considered if a ligamentous injury is suspected. The management of Type I and Type III odontoid fractures has little controversy. In the setting of a Type I fracture, upper cervical instability and occipitocervical (OC) dislocation must be excluded. In the absence of dislocation or instability, these injuries can be managed with a collar until symptoms subside. Type III fractures occur through the C2 body, which has a relatively robust blood supply and healing potential; following closed reduction, these injuries will usually heal with immobilization in a hard cervical orthosis or halo vest. However, Type III fractures with anterior displacement may be biomechanically unstable and are at risk for repeat displacement with closed management. In the setting of anterior displacement, management with internal fixation should be considered.7 Type II odontoid fractures present a management challenge because of the confluence of several factors. The blood supply of C2 is sparse at the base of the dens because of the presence of a true synovial joint. Coupled with a relative thinning of the trabeculae,8 the biological environment is not conducive to bony union. Fracture displacement and age > 50 years are the predominant risk factors for nonunion with closed management. Union rates for C2 fractures with closed management (cervical orthosis) have been reported to be as low as 15% in the elderly.9 With surgical intervention, union rates with direct osteosynthesis (anterior odontoid screw) range from 80 to 100%,7,10–13 and posterior fusion rates with modern instrumentation techniques exceed 90%.14 The outcome of a nonunion in the elderly is controversial. If there is minimal fracture displacement, some consider a stable fibrous nonunion to be an acceptable outcome.15 In the setting of an unstable nonunion, there is significant concern both for the risk of catastrophic neurological injury with a subsequent fall and for the potential development of late-onset myelopathy. Nonoperative management consists of immobilization in either a cervical orthosis or a halo vest. The success of immobilization is predicated, in large part, on the degree of fracture displacement. Studies that have documented high nonunion rates for Type II odontoid fractures have had fracture displacements that exceeded 2 mm. Therefore, particularly in the elderly, it is unlikely that a displaced fracture will achieve a stable union with immobilization. In the setting of a minimally displaced odontoid fracture, successful outcomes with non-operative management have been demonstrated to range from 74 to 90%,15,16 if one accepts a stable fibrous nonunion. Bony union with closed management, even in the setting of minimal displacement, is unlikely to exceed 50%.15 Nonoperative management necessitates close surveillance and consideration of C1–C2 stability. Particularly given the fall risk inherent to a subset of the elderly population, the relative merits of a fibrous nonunion and the relative risk of C1–C2 instability in the setting of a nonunion, compared with the risk of operative intervention, are patient-specific. The goal of operative intervention is to achieve either direct osteosynthesis of C2 (anterior procedure) or C1–C2 stability via a posterior C1–C2 fusion. Anterior screw fixation and direct osteosynthesis were first described by Bohler et al.11 Union rates have been reported to be between 70 and 96%,10,12,17–19 with higher rates of nonunion in the elderly.18 Fracture reduction prior to fixation is crucial, and an irreducible fracture is an absolute contraindication to anterior fixation. Similarly, an incompetent transverse ligament is also a contraindication, as there will be continued C1–C2 translational instability after fixation. A significant advantage of anterior direct osteosynthesis is the maintenance of axial rotation due to the avoidance of a posterior C1–C2 fusion.20,21 The fixation, achieved via a lag-screw technique and cortical screw purchase, is integral to achieving compression at the fracture site. Increased rates of instrumentation failure have been reported in the elderly population, and it is hypothesized that this is due to osteoporosis.17 A chronic fracture is a relative contraindication to anterior fixation because of the increased incidence of nonunion.10 Posterior management aims to fuse the posterior elements of C1 and C2. Historically, this was accomplished with Brooks fusion technique. With modern instrumentation the technique has evolved to C1–C2 transarticular instrumentation and fusion (Magerl) and C1 lateral mass/C2 pars instrumentation (popularized by Harms). Fusion rates generally exceed 90% with either technique. Harms technique is increasingly supplanting transarticular fixation,1 largely because of the perceived lower risk of injury to the vertebral artery. In addition to the higher rate of fusion, with the use of modern instrumentation, surgeons are increasingly opting for a cervical orthosis postoperatively in lieu of halo vest immobilization. Multiple studies indicate that Type II odontoid fractures are associated with significant morbidity in the elderly, with either surgical or nonsurgical management.22–25 There is increased recognition of the morbidity of halo vest immobilization in the elderly, with some observing acute mortality rates as high as 42% in patients managed with halo vest immobilization.26 Conversely, others have reported relatively few significant problems with the use of halo vests.15,27,28 As these studies are retrospective and of single-center cohorts, the divergence in results likely reflects that halo vest management necessitates specialized care, and the role of halo vest use is likely institution-specific. Postoperatively, the clinical team must be prepared for potential airway and swallowing complications, which, although observed with both anterior and posterior approaches, are more prevalent in the former.1 1. Smith HE, Vaccaro AR, Maltenfort M, et al. Trends in surgical management for type II odontoid fracture: 20 years of experience at a regional spinal cord injury center. Orthopedics 2008;31(7):650 PubMed 2. Panjabi MM, Crisco JJ, Vasavada A, et al. Mechanical properties of the human cervical spine as shown by three-dimensional load-displacement curves. Spine (Phila Pa 1976) 2001;26(24):2692–2700 PubMed 3. Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: clinical, radiological, and surgical features. J Neurosurg 1993;78(4):579–586 PubMed 4. Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am 1974;56(8):1663–1674 PubMed 5. Barker L, Anderson J, Chesnut R, Nesbit G, Tjauw T, Hart R. Reliability and reproducibility of dens fracture classification with use of plain radiography and reformatted computer-aided tomography. J Bone Joint Surg Am 2006;88(1):106–112 PubMed 6. Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J 2005;5(2):123–129 PubMed 7. Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 2006;31(11, Suppl):S53–S60, discussion S61 PubMed 8. Heggeness MH, Doherty BJ. The trabecular anatomy of the axis. Spine (Phila Pa 1976) 1993;18(14):1945–1949 PubMed 9. Ryan MD, Taylor TK. Odontoid fractures in the elderly. J Spinal Disord 1993;6(5):397–401 PubMed 10. Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg 2000;93(2, Suppl):227–236 PubMed 11. Böhler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am 1982;64(1):18–27 PubMed 12. Börm W, Kast E, Richter HP, Mohr K. Anterior screw fixation in type II odontoid fractures: is there a difference in outcome between age groups? Neurosurgery 2003;52(5):1089–1092, discussion 1092–1094 PubMed 13. ElSaghir H, Böhm H. Anderson type II fracture of the odontoid process: results of anterior screw fixation. J Spinal Disord 2000;13(6):527–530, discussion 531 PubMed 14. Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord 1992;5(4):464–475 PubMed 15. Koech F, Ackland HM, Varma DK, Williamson OD, Malham GM. Nonoperative management of type II odontoid fractures in the elderly. Spine (Phila Pa 1976) 2008;33(26): 2881–2886 PubMed 16. Müller EJ, Schwinnen I, Fischer K, Wick M, Muhr G. Non-rigid immobilisation of odontoid fractures. Eur Spine J 2003;12(5):522–525 PubMed 17. Harrop JS, Przybylski GJ, Vaccaro AR, Yalamanchili K. Efficacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus 2000;8(6):e6 PubMed 18. Platzer P, Thalhammer G, Ostermann R, Wieland T, Vécsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976) 2007;32(16):1714–1720 PubMed 19. Subach BR, Morone MA, Haid RW Jr, McLaughlin MR, Rodts GR, Comey CH. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery 1999;45(4): 812–819, discussion 819–820 PubMed 20. Platzer P, Thalhammer G, Oberleitner G, Schuster R, Vécsei V, Gaebler C. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am 2007;89(8):1716–1722 PubMed 21. Jeanneret B, Vernet O, Frei S, Magerl F. Atlantoaxial mobility after screw fixation of the odontoid: a computed tomographic study. J Spinal Disord 1991;4(2):203–211 PubMed 22. Smith HE, Kerr SM, Maltenfort M, et al. Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech 2008;21(8):535–539 PubMed 23. Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients; a prospective study of sequential cohorts with attention to survivorship. J Spinal Disord 1995;8(2):166–169 PubMed 24. Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in elderly patients. J Neurosurg 1993;78(1):32–35 PubMed 25. Müller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J 1999;8(5):360–365 PubMed 26. Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma 2006;60(1): 199–203 PubMed 27. Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: a success and survivorship analysis. Spine (Phila Pa 1976) 2009;34(15): 1561–1566 PubMed 28. Platzer P, Thalhammer G, Sarahrudi K, et al. Nonoperative management of odontoid fractures using a halothoracic vest. Neurosurgery 2007;61(3):522–529, discussion 529–530 PubMed Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: clinical, radiological, and surgical features. J Neurosurg 1993;78(4):579–586 PubMed Description of late-onset progressive myelopathy in a cohort of ondontoid fracture nonunions. Crockard et al. found that the transverse ligament was frequently interposed in the fracture. Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J 2005;5(2):123–129 PubMed Vaccaro et al. proposed a modified classification of odontoid fractures incorporating fracture obliquity, displacement, and comminution. These factors are important considerations for type of treatment and surgical technique (if operative treatment is utilized). Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 2006;31(11, Suppl):S53–S60, discussion S61 PubMed A thorough literature review of the treatment of odontoid fractures. Smith HE, Kerr SM, Fehlings MG, et al. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a Model System Spine Injury tertiary referral center. J Spinal Disord Tech 2010;23(8):501–505 PubMed A review of the historical trends in the epidemiology and management of odontoid fractures. There is a marked epidemiological trend of increased incidence of this injury in an aging population and an increasing probability of operative management. Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma 2006;60(1):199–203 PubMed Tashjian et al. identify a significant incidence of complications and a high relative risk of mortality in elderly patients with the use of halo vest immobilization. CT, computed tomography; MRI, magnetic resonance imaging
Odontoid Fractures
![]() Classification
Classification
![]() Workup
Workup
History
Imaging
![]() Treatment
Treatment
![]() Nonoperative Management
Nonoperative Management
![]() Operative Management
Operative Management
Anterior Odontoid Screw Fixation
Posterior Fusion
![]() Complications
Complications
References
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







