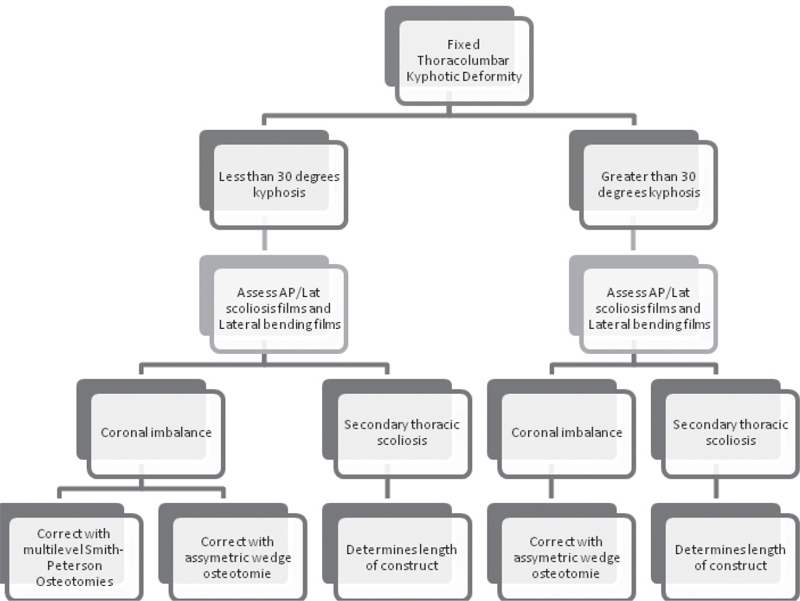
43 Trauma to the spinal column, with or without injury to the spinal cord, has life-changing and potentially devastating consequences for patients. With advances in the use of imaging modalities, including radiography, computed tomography (CT), and magnetic resonance imaging (MRI), unstable fractures are often treated with immobilization or surgical stabilization acutely. Despite the advances in the diagnosis and treatment of unstable spinal fractures, delayed complications, including post-traumatic thoracolumbar kyphosis, can develop. One likely source for the development of thoracolumbar kyphotic deformities is unrecognized or occult instability with thoracolumbar trauma. Post-traumatic kyphosis typically results from injury to the anterior and posterior columns of the spine. As has been noted in recent classification systems, such as the Thoracolumbar Injury Classification and Severity Score (TLICS), the posterior ligamentous structures play an important role in spinal stability, and disruption of posterior ligaments is likely a key factor in the development of post-traumatic kyphosis. The center of axis for body weight is carried ventral to the spine, and the posterior musculature and ligaments act to hold the spine in an erect posture. Disruption of the posterior tension band allows the body weight to pull the spine ventrally into a kyphotic posture. The posterior ligaments can be evaluated by multiple techniques, including physical examination findings and radiographic studies, but the sensitivity and specificity for detecting ligamentous injuries are questioned with all of these techniques. Clinical studies of the TLICS classification and other classification systems have found a very poor inter-observer reliability in classifying spinal injuries and, especially, in determining the integrity of the posterior spinal ligaments. As a result, spinal injuries are not treated uniformly, and it can be expected that some unstable fractures do not receive sufficient treatment, resulting in the development of post-traumatic kyphotic deformities. Aside from underestimating the extent of injury and potential for instability, other causes include pseudarthrosis, instrumentation failure, infections, and inadequate surgical stabilization. Fracture nonunion, with or without evidence of instrumentation fatigue, has been implicated. In cases of suspected nonunion, extensive workup for deep wound infection should be performed, as infections may clinically mimic or even cause chronic nonunions. Implant and instrumentation failure has been reported in as many as 16% of patients requiring reoperation. Causes of implant failure may be related to excessive force on the implants, surgical technical errors, poor implant selection, insufficient number of levels fused, infection, osteoporotic bone, or patient noncompliance with bracing or immobilization devices. Surgical risk factors for delayed formation or progression of kyphotic deformity include laminectomy alone in the setting of an unstable injury or including too few segments in a thoracolumbar fusion procedure. Instrumentation and fusion of five or more spinal segments (two above the injured level and two below) is less likely to result in postoperative deformity. Charcot spine has also been associated with delayed development of thoracolumbar kyphosis. The most common presenting symptom of post-traumatic kyphosis is pain. The pain is usually constant and aching, centered at the apex of the deformity. The pain is typically increased with prolonged standing or activity. The sagittal balance of the kyphotic spine is shifted ventrally with standing, creating a biomechanical disadvantage for the posterior musculature. As a result, the muscles fatigue and pain is produced. The more caudal in the spine the kyphotic deformity, the greater the effect of the deformity on the sagittal balance, and the deformity is subsequently less well tolerated by the patient. Additional factors associated with intolerable pain include the severity of the deformity, disk degeneration, canal compromise, angular deformity, pseudarthrosis/non-union, and focal instability. There is up to a 27% incidence of progressive neurologic deficit in spinal cord injury patients with post-traumatic deformity. Potential causes of neurologic deterioration include spinal cord compression associated with the progressive kyphotic deformity, development of post-traumatic syringomyelia, and possible cystic myelopathy related to arachnoid adhesions at the site of injury. With progressive kyphotic deformity, the spinal cord can become draped over anterior compressive pathology, such as residual bone fragments associated with a burst fracture compromising the ventral spinal canal, and with normal body movements the cord is further damaged as it slides over the anterior pathology. Patients with less than 15 degrees of kyphosis and less than 25% canal stenosis are less likely to develop hydromelia than are patients with greater deformity. Given the complexity involved in the radiographic evaluation of post-traumatic spinal deformity, multiple imaging modalities are typically necessary. Plain radiographs are crucial in the evaluation of suspected kyphotic deformities. Standing or upright AP and lateral scoliosis films with flexion, extension, and lateral bending are necessary to understand fully the degree of kyphotic deformity and to provide an evaluation of spinal mobility during physiologic range of motion. Likewise, serial plain radiographs are a useful tool for following and documenting changes in the post-traumatic deformity longitudinally. CT scanning of the affected levels using thin cuts and multiple-planar reconstruction is useful in obtaining detailed bony anatomy as part of preoperative planning. In some instances, such as presence of spinal instrumentation or in the evaluation of intradural pathology like arachnoid adhesions, CT combined with myelography can provide valuable information about neural pathology. MRI can be helpful in the acute trauma evaluation for ligamentous injury, which may lead to progressive instability in the future. In the setting of a chronic deformity, MRI provides soft-tissue resolution for assessing the spinal cord for compression, myelomalacia, syringomyelia, or arachnoid adhesions. The decision to proceed with surgery is best made after careful discussion with the patient and his or her family about the patient’s symptoms and the goals and expectations following surgery to correct the kyphotic deformity. As a general rule of thumb, surgery is indicated when significant pain is combined with altered function in a patient with a sagittal index greater than 20 degrees. The location of the pain is variable and can be associated with the apex of the deformity or in any exaggerations of the normal lordosis or kyphosis of the spine. If the patient has not developed a hyperlordosis of the lumbar spine, there will be a forward listing posture that can be severe enough to limit the patient’s line of sight. Additional strong factors in favor of surgical management include pseudarthrosis, disk degeneration, and neurologic deficit caused by neural compression associated with the kyphotic deformity. Cosmetic concerns must also be taken into consideration and must be discussed with the patient. Surgery should be approached with extreme caution in patients with mild deformity and severe pain. There is a percentage of patients who will have persistent pain after spinal trauma, and in some instances this pain is not amenable to surgical intervention. Successful surgical intervention for the treatment of post-traumatic thoracolumbar kyphosis is highly dependent upon the surgeon’s skill in patient selection, education, and operative techniques. The goal of surgery is always to give reproducible results with low rates of complications. With aggressive surgical correction of deformity, morphological changes in the presenting deformity of greater than 50–70% can be achieved. In assessing patients with pain relief as the primary outcome measure, success rates as high as 60–70% may be achievable. More severe deformities can give the surgeon an increasing confidence in the ability of the surgery to improve pain. Greater patient age, work-related injury, and psychosocial problems are generally regarded to be negative prognosticators for pain relief following surgery. The goals of the surgery must be carefully considered by both the operating surgeon and patient prior to surgery. Typically the goals of surgery are threefold: (1) Restore sagittal balance of the spine to allow for a normal straight posture. (2) Perform decompression of any neural elements compromised by the deformed level. (3) Cure pain related to pathologic curves by restoring a normal spinal alignment and repairing any spinal instability. The ultimate decision about the correct and appropriate surgery for a given patient is best made in collaboration with the patient, combining patient symptoms, radiographic studies, and surgeon experience to tailor the treatment plan to each individual case. Thoracolumbar kyphosis can be addressed from either the posterior, anterior, or combined anterior/posterior approach (refer to algorithm at beginning of chapter). There are studies showing efficacy of each approach, but for severe deformities the posterior approach with an osteotomy allows for more radical correction of post-traumatic kyphotic deformities. It is also important to consider the coronal plane balance, and in patients with scoliosis in conjunction with kyphotic deformity, consider asymmetric wedge osteotomies to correct the balance of both the coronal and sagittal planes (Fig. 43.1). In situations of progressive neurological deficits, a thorough decompression of the spinal canal is needed in addition to correction of the deformity. For patients with osteopenia or osteoporosis, cement augmentation of the vertebral bodies at the cephalad and caudal extent of the spinal instrumentation may be considered to prevent hardware loosening. There may also be a benefit with the use of cobalt chromium rods over titanium rods for improved strength to reduce the risk of rod breakage in these extensive deformity corrections. Fig. 43.1 Algorithm for fixed thoracolumbar kyphotic deformity.
Post-Traumatic Thoracolumbar Kyphosis
![]() Classification
Classification
Presenting Symptoms
Pain
Neurologic Deficit
![]() Evaluation
Evaluation
Radiographic Evaluation
![]() Treatment
Treatment
Indications for Surgery
Surgical Prognosticators
Surgical Goals
Surgical Procedures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






