Fig. 1
(a) In an anteverted acetabulum, the posterior rim (red line) is projected laterally to the anterior rim (blue line) and both converge towards the cranio-lateral edge of the acetabulum. (b) Acetabular retroversion is defined by a positive crossover [1, 4, 6], posterior wall [1], and ischial spine sign [7]. A crossover sign is considered positive if the anterior acetabular rim crosses the course of the posterior rim [1]. With increasing retroversion of the acetabulum, the crossover sign is projected more caudally. The retroversion index (ratio of distance “a” to “b”) quantifies the extent of acetabular retroversion. The posterior acetabular wall sign is positive if the deficient posterior acetabular wall runs medial to the femoral head center [1]. The ischial spine sign is considered positive if the ischial spine (arrow) is projected medially to the pelvic brim [7]. (c) Rarely total acetabular retroversion occurs with the entire acetabulum facing posteriorly. These cases can be missed because of the missing crossover sign. The entire anterior acetabular rim is projected laterally to the posterior wall on the AP pelvic radiograph. Typically, the anterior and posterior acetabular walls converge in the cranio-lateral edge and from an obtuse angle (arrows) instead of a sharp angle like in anteverted hips
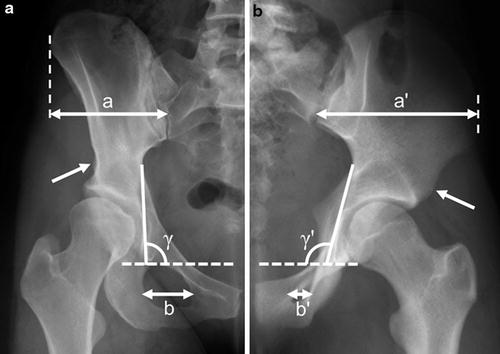
Fig. 2
Acetabular retroversion is the result of an externally rotated hemipelvis [7, 12–15] rather than an anterior wall prominence and/or a posterior rim hypoplasia as suggested previously [3]. Several extra-articular anatomical landmarks associated with acetabular retroversion exist. (a) Half an AP pelvic radiograph with a dysplastic hip in comparison with (b) half an AP pelvic radiograph with a retroverted hip. (a) The pelvis with an acetabular retroversion typically has a lateral protruding iliac wing (a′ > a), a narrow obturator foramen (b′ < b), a prominent anterior inferior iliac spine (arrows), and a less steep ilio-ischial line (γ′ > γ) [15] (Figure reprinted with permission)
Very rarely total acetabular retroversion occurs with the entire acetabulum facing posteriorly (Fig. 1). These cases can be missed because of an absent crossover sign. The entire anterior acetabular rim is projected laterally to the posterior wall on the AP pelvic radiograph (Fig. 1). Typically, the anterior and posterior acetabular walls converge in the cranio-lateral edge and from an obtuse angle instead of a sharp angle in anteverted hips (Fig. 1).
The axial view (e.g., cross-table axial) is used to evaluate the femoral head-neck offset. A cam-type deformity is often present in hips with acetabular retroversion [2]. An untreated cam-type deformity can adversely affect the long-term outcome following acetabular reorientation [17, 20].
Magnetic resonance (MR) arthrography of the hip with radial sequences, intra-articular contrast agent (gadolinium), and flexible surface coils is the current gold standard to detect chondrolabral pathologies in hips [21]. This imaging modality with radial sequences also allows exact location of additional cam-type deformities around the femoral neck. At the author’s institution some additional MR slices at the height of the distal femur are performed which allows evaluating femoral antetorsion [22]. MR arthrography is not performed routinely in patients with acetabular retroversion but might be indicated in older patients to quantify chondrolabral damage.
Although computed tomography (CT) imaging allows exact three-dimensional evaluation of acetabular orientation, it is not performed on regular basis for diagnosis of acetabular retroversion. It can be used to determine femoral antetorsion and to evaluate whether a concomitant intertrochanteric femoral osteotomy is indicated [23]. Recently, a CT-based method has been introduced for three-dimensional planning of PAO with simulation of postoperative range of motion and possible impingement conflicts [24]. Accurate realization of the planned acetabular reorientation is accomplished using CT-based navigation [24].
Indication for Reverse PAO
Indication for acetabular reorientation is based on a positive correlation of symptoms, physical findings, and radiographic findings. Typically, patients with acetabular retroversion present with groin pain and decreased flexion and internal rotation [17, 18]. The anterior impingement test, performed with the patient supine and internal rotation in 90° of flexion, results in reproducible hip pain [4]. In extreme forms of acetabular retroversion, the anterior impingement test might not be possible, and there is unavoidable passive external rotation in flexion (positive Drehmann’s sign [25]). Radiographically, indication is based on a combination of positive crossover [1, 4, 6], posterior wall [1], and ischial spine sign [7] with an acetabular retroversion index exceeding 30 % (Fig. 1). Typically, these patients are young with the majority aged less than 35 years [18]. A contraindication is advanced osteoarthritis Tönnis grade > 1 [26]. Ideally, the arthro-MRI shows no or minor chondrolabral damage.
Concomitant surgical procedures comprise the arthrotomy with offset correction or intertrochanteric osteotomies. Offset of the anterior femoral head-neck junction is judged on the axial view of the hip. An alpha angle exceeding 50° is considered insufficient offset [27]. However, intraoperative testing of range of motion following acetabular reorientation is crucial. Often a cam-type deformity limits internal rotation. If a minimum of 30° of internal rotation in 90° of flexion is not achieved, an arthrotomy with offset correction is indicated. A concomitant intertrochanteric osteotomy in hips with acetabular reorientation due to retroversion is rarely indicated. A high femoral antetorsion could potentially result in a posterior impingement following acetabular reorientation [28]. A derotational femoral osteotomy could be indicated in these hips.
PAO Versus Surgical Hip Dislocation
Trimming of the prominent anterior acetabular wall in retroverted hips can potentially decrease the size of the articular surface to a critical level resulting in a dysplastic hip. However, surgical hip dislocation with acetabular rim trimming can be an alternative in some selected hips with a lower degree of acetabular retroversion. Hips with a retroversion index of less than 30 % and a negative posterior wall sign are eligible for rim trimming [17, 18]. In these hips a sufficient size of the articular surface can be obtained following acetabular rim trimming [17, 18]. In contrast, a reverse PAO resulted in a too prominent posterior wall and a posterior impingement [17, 18].
Surgical Technique
In general, the approach and the sequence of osteotomies do not differ in a PAO performed for acetabular retroversion compared to a PAO for hip dysplasia [16]. The surgery is performed under general anesthesia with full muscle relaxation. The patient is positioned supine on a radiolucent table. Sterile draping of the leg should allow mobility of the leg during surgery. The entire iliac crest and femur should be accessible. A blood salvage device may be used to encounter excessive blood loss.
A modified Smith-Petersen approach [29] is used with an incision reaching from the anterior third of the iliac crest to the anterior superior iliac spine. The incision is then curved and extended caudally along the anterior boarder of the tensor muscle for approximately 10 cm (Fig. 3). Care must be taken not to injure the lateral femoral cutaneous nerve (Fig. 3). The fascia is incised at the anterior border of the tensor muscle. Staying within the fascial sheath of this muscle will protect the lateral femoral cutaneous nerve. The tensor fascia lata muscle is retracted laterally. Flexion of the leg decreases tension of the tensor muscle. A further deep fascia layer is incised longitudinally, and the reflected tendinous portion of the origin of the rectus femoris muscle is exposed. Distally, the ascending branch of the lateral femoral circumflex artery crosses the intermuscular interval of tensor and rectus muscles. This vessel should be preserved and it usually represents the distal end of the exposure.
Fig. 3
The periacetabular osteotomy (PAO) is performed through a modified Smith-Petersen approach. The incision includes the anterior third of the iliac crest, is curved at the anterior superior iliac spine (ASIS), and runs distally along the anterior boarder of the tensor muscle. Care must be taken not to injure the lateral femoral cutaneous nerve, which pierces the fascia of the thigh close to the intermuscular interval of tensor and sartorius muscles
At this point the aponeurosis of the abdominal muscles is detached from the anterior third of the iliac crest sharply with a knife like it is done for exposure of the first window in an ilioinguinal approach. With the hip in flexion and adduction, the iliacus muscle is bluntly mobilized from the iliac bone. The inguinal ligament and the sartorius muscle are detached subperiosteally from its origin at the anterior superior iliac spine (ASIS; Fig. 4). This step has replaced the osteotomy of the ASIS, which was performed routinely in earlier years [16]. Dissecting the inguinal ligament and the sartorius muscle of the ASIS connects the first ilioinguinal window with the previously performed exposure of the anterior aspect of the hip joint area. Medial retraction of the rectus muscle with a blunt retractor exposes the iliocapsularis muscle which is attached to the anterior aspect of the capsule. Sharp dissection of its lateral border from the capsule allows medial mobilization. In order to preserve the rectus muscle attachment, the proximal aspect of this muscle is now retracted laterally in order to continue complete sharp dissection of the iliocapsularis muscle from the capsule (Fig. 5). Additional medial retraction of the iliopsoas muscle is facilitated by adduction and flexion of the hip joint. The psoas tendon is retracted medially with a Hohmann retractor which is placed into the superior pubic ramus medially to the eminentia iliopubica (Fig. 5). This protects the femoral nerve and vessels that are located medially to the psoas tendon. This will lead to exposure of the anterior inferior iliac spine and of the corpus pubis and the psoas tendon surrounded by the iliopectineal bursa.
Fig. 4
The inguinal ligament and the sartorius muscle are detached from its origin at the anterior superior iliac spine (ASIS) and retracted medially. By retracting the tensor fascia lata muscle laterally, the joint capsule and the origin of the rectus muscle with its direct and reflected portions are exposed
Fig. 5
The iliocapsularis muscle is dissected sharply from the anterior joint capsule, but its origin at the anterior inferior iliac spine (AIIS) is left intact. The iliocapsularis muscle is retracted medially. The psoas tendon is retracted medially with a Hohmann retractor which is brought into the superior pubic ramus medially to the eminentia iliopubica. The infra-articular space between the psoas tendon and the capsule is dissected bluntly with a pair of scissors until the tip of the instrument touches the base with the medial aspect of the ischial bone lateral to the obturator foramen
Finally, blunt dissection of the infra-articular space between the psoas tendon and the capsule with a pair of scissors is performed until the tip of the instrument touches the base with the medial aspect of the ischial bone lateral to the obturator foramen (Fig. 5).
For preparation of the outer aspect of the pelvis, subperiosteal dissection is performed starting between the superior and inferior anterior iliac spine. Only limited dissection of the outer part of the pelvis is necessary to place a blunt pelvic retractor in the sciatic notch, thereby protecting the musculature and the sciatic nerve during supra-acetabular und retroacetabular osteotomy. In addition, limited dissection allows to preserve the proximal remaining fibers of the origin of the tensor fascia muscle and the origin of the gluteus minimus containing the inferior branch of the superior gluteal artery providing blood supply to the supra-acetabular bone.
In total, four periacetabular osteotomies and a controlled retroacetabular fracture are performed to mobilize the acetabular fragment. The ischial osteotomy is done first (Fig. 6). It is performed with a special osteotome (Ganz osteotome) with a notched 15 mm blade that is 30° angulated towards the shaft. The osteotome is placed into the space between the distal joint capsule and the psoas tendon with the hip flexed and abducted to lateralize the position of the sciatic nerve (Fig. 6). The infracotyloid groove at the level of the inferior border of the acetabulum is palpated with the osteotome (Fig. 6). The correct position of the blade can be verified with an image intensifier. While the shaft of the osteotome points towards the patient’s contralateral shoulder, the blade is hammered into the ischium to a depth of 2.5 cm. The shape of the ischial body is triangular with its base posterior. A complete osteotomy of the medial cortex is more important than of the thinner lateral cortex as the lateral cortex eventually breaks while the acetabular fragment is mobilized. The osteotome is carefully retrieved. Palpation with the osteotome assures whether the medial and lateral aspects of the ischial body are osteotomized correctly. The ischial osteotomy is incomplete to maintain the posterior column and the continuity of the pelvic ring (Fig. 6).
Fig. 6
The ischial osteotomy is performed with the Ganz osteotome which is placed in the infracotyloid groove. The hip is flexed and abducted to lateralize the position of the sciatic nerve. The shaft of the Ganz osteotome is pointed towards the patient’s contralateral shoulder. The ischial osteotomy is incomplete to maintain the posterior column
The second osteotomy is done through the medial aspect of the superior pubic ramus just medial to the eminentia pubica (Fig. 7). A Hohmann retractor is placed medially into the superior pubic ramus to retract the soft tissue medially and to protect the neurovascular structures (Fig. 7). The hip is flexed and adducted in order to relax the soft tissues. Subperiosteal placement of two blunt retractors around the origin of the superior pubic ramus helps to avoid damage to the adjacent obturator nerve and vessels. A complete, transverse osteotomy of the pubic ramus medially to the pubic eminentia is performed with 15 mm Lexer chisel (Fig. 7).