Fig. 1
Typical appearance of the dislocated hip with adduction contracture in a spastic patient

Fig. 2
X-ray showing the dislocated left hip
The untreated hip dislocation in the spastic patient population has a poor natural history [1] and the results of all procedures have poor outcomes in the growing child vs. the young adult.
The goals of surgery for the spastic dislocated hip are fourfold [2]: (1) relieve adduction contractures to facilitate perineal hygiene and nursing care, (2) restore hip mobility enough so as not to interfere with positioning in bed or chair, (3) simple procedure so as to minimize complicated postop care and prolonged hospitalization, and (4) one-stage operation.
The majority of these patients are nonambulatory, so the procedure is one to improve the quality of life, with its inherent economic and humanitarian implications.
Prevention is obviously the preferred treatment for the patient with spastic hip subluxation/dislocation , with early surgical intervention and the appropriate soft tissue releases and femoral and/or pelvic osteotomies. However, for long-standing cases with significant acetabular dysplasia as well as a deformed and eroded femoral head, measures other than containment are necessary. Options include simple soft tissue release, valgus osteotomy, Girdlestone procedure of femoral head and neck resection , proximal femoral resection with interposition arthroplasty, arthrodesis, and total hip arthroplasty.
Soft tissue release alone is insufficient to relieve pain and deformity, and valgus/abduction osteotomies often result in a stiff hip with skin breakdown over the prominent femoral head and difficulty with positioning [2–4]. The Girdlestone procedure is complicated by heterotopic ossification and proximal femoral migration with recurrent pain and deformity [2, 5–7]. These procedures are no longer recommended.
Proximal femoral resection with interposition arthroplasty [2, 5] has generally provided good pain relief and positioning ability, but still has problems with heterotopic ossification and requires traction postoperatively, requiring additional time in recumbency or rigging of the wheelchair. Hip arthrodesis [7] is only for patients with a normal contralateral hip and spine, often requires a concomitant proximal femoral osteotomy for positioning, and may develop heterotopic ossification and pseudarthrosis and maybe a hard sell to the patient and family. Total hip arthroplasty [7] often requires a custom stem and difficulty with positioning the acetabular component at its true level, requires a spica cast or brace for immobilization postoperatively, and has the inherent problems of dislocation, loosening, and wear.
Our preferred treatment is the McHale osteotomy , which combines a femoral head and neck resection with adductor release and a proximal femoral valgus osteotomy with internal fixation [4]. This is a one-stage operation that fulfills all the goals of surgery.
Technique
The patient is positioned supine under general anesthesia on the operating table with a bump or roll under the hip. Additional caudal or epidural block is at the discretion of the surgeon and the anesthesiologist. An adductor release of the longus and brevis is performed through a longitudinal incision in the groin over the adductor longus tendon, and dissection carried through to release the adductor longus and brevis. Obturator neurectomy is not routinely performed. The incision is closed in a standard fashion and attention is then turned laterally to the hip joint itself.
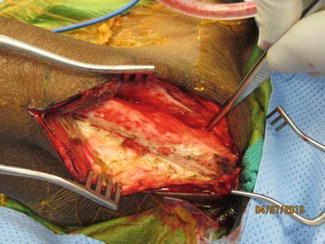
A straight lateral incision is made from approximately level with the anterior superior iliac spine, across the greater trochanter, and down the femoral shaft. An anterolateral approach to the hip, i.e., Watson-Jones, is used (Fig. 3). The fascia is exposed in line with the skin incision and split longitudinally, taking care to remain posterior to the posterior border of the tensor fascia lata proximally. Cutting too far anteriorly in the muscle belly of the tensor may make it difficult to discern the plane between the gluteus medius and tensor fascia lata.