Fig. 1
MRI of the right hip. T1-weighted coronal (a) and sagittal (b) images demonstrating an osteochondral defect in the weight-bearing region of the right femoral head
Preoperative planning is paramount when OAT and OCA are considered options for hip preservation surgery. When OAT is indicated, consideration must be given to the planned donor site. Reported donor sites for treatment of articular defects of the hip include low-weight-bearing areas such as the inferior aspect of the femoral head and the femoral head and neck junction in instances where a concomitant cam lesion exists [5, 8, 14–16]. Alternatively, the lateral margin of the femoral trochlea in the knee may be used [8, 16, 17]. The advantage of harvesting osteochondral plugs from a local donor site in the hip are implicit in that there is no requirement for a separate incision, limiting donor site morbidity. When a large osteochondral lesion necessitates OCA, arrangements must be made for a fresh allograft that should ideally be stored at 4 ºC for no longer than 28 days, requiring some flexibility in scheduling surgery [18]. Allograft options reported in the literature for the acetabular defects include the medial tibial plateau and the acetabulum [19]; however, the availability of fresh acetabulum allograft can be particularly difficult. For defects of the femoral head, the use of allograft femoral head has been described in a number of studies [20–23].
Surgical Technique
Articular defects amenable to OCA or OAT require an open approach to the hip. Although various approaches have been described in the literature for restorative cartilage procedures, the surgical hip dislocation, as described by Ganz, offers full access to the femoral head and acetabulum while preserving blood flow to the femoral head and is therefore the preferred approach [24, 25]. After safely exposing the femoral head and acetabulum, the typical sequence of events is as follows: preparation of the recipient site, graft harvest from the donor site, and finally, placement of graft into the defect. Any one of the commercially available systems may be used to complete the steps as outlined below for OAT and OCA.
OAT and Mosaicplasty
Preparation of the recipient site initially involves debridement of the defect to stable margins of surrounding bone and cartilage . The defect is then sized to determine the appropriate dimensions and configuration of the donor plug, or plugs that may be required. When mosaicplasty is required, a 2–3 mm bone bridge should be preserved between donor plug areas whenever possible, to avoid graft instability and convergence (Fig. 2). Finalization of the recipient site by drilling to the appropriate size and depth is then completed. The recipient site may be under-drilled by 1 mm in some systems to allow for press-fit impaction of the graft. Donor plug harvest sites for the hip include local and remote options as previously outlined. When harvesting the graft, care should be taken to ensure the harvester remains perpendicular to the articular surface as this increases the likelihood of obtaining a congruent surface at the time of graft impaction. The harvester is advanced with gentle blows of a mallet to the appropriate depth, and the graft is then removed. Graft insertion is accomplished according to the system used. Typically there is a plunger that assists with the introduction of the graft into the defect, with a final impactor for fine-tuning. Throughout the introduction, care should be taken to avoid forcefully impacting the graft as this can lead to chondrocyte damage. Finally, back filling of the donor site can be considered at this time with either osteochondral allograft or a synthetic bone void filler [8]. When transferring multiple plugs, it is preferred to harvest and insert each plug fully before proceeding with the next plug.
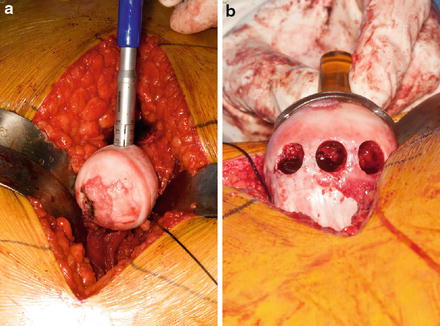
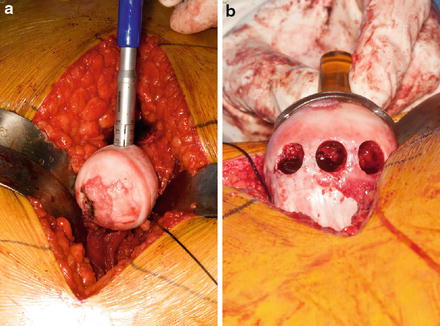
Fig. 2
Intraoperative photographs demonstrating the use of mosaicplasty for an osteochondral defect of the femoral head. (a) Osteochondral plug harvest from a non-weight-bearing region of the proximal femur. (b) Care should be taken to preserve a bone bridge of at least 2–3 mm between harvest sites
OCA
Preparation of the recipient site for OCA begins as outlined for OAT. Sizing for OCA is accomplished with a cannulated cylindrical sizer. A guide pin is placed into the bone through the sizer and the recipient site is reamed over the guide pin to the specified depth based on the system used. The recipient site should be marked with a reference point, and the depth of the defect after reaming should be measured in four quadrants. Harvest from the donor site begins with placement of the cylindrical sizer and guidewire into the portion of the allograft that will provide the best fit at the recipient site. When using allograft of the same bone (i.e., femoral head allograft for femoral head defect or acetabular allograft for the acetabulum), reference points may be used to match the location of donor and recipient sites. When alternative options are used (i.e., tibial plateau for acetabulum), the best fit should be sought based on surface characteristics The allograft is harvested with a cylindrical drill and the depth is fine-tuned based on the measurements of the four quadrants measured at the recipient site. The deep edges of the graft may be tapered with a rongeur prior to insertion. The allograft is then press fit, taking care to orient the graft ensuring the depth of the graft matches the depth of the recipient site in all four quadrants as measured (Figs. 3 and 4).
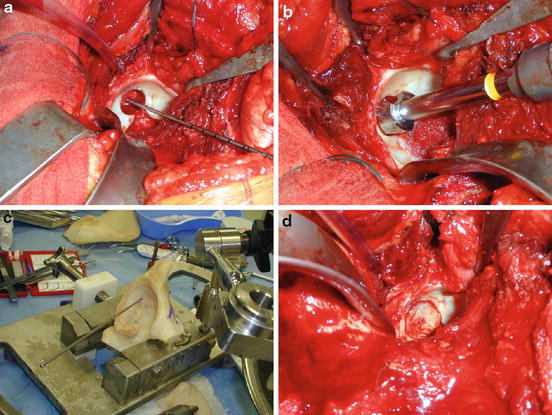
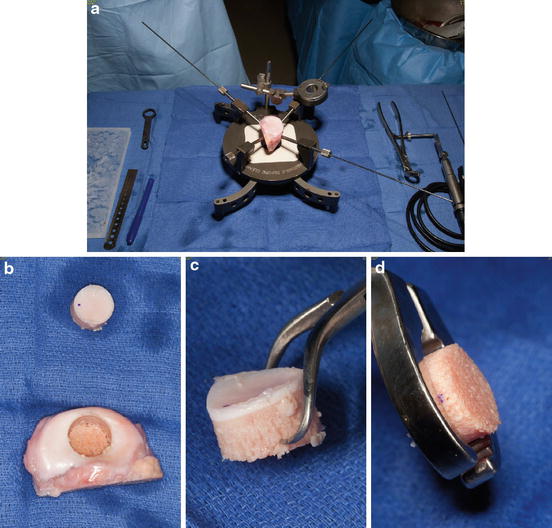
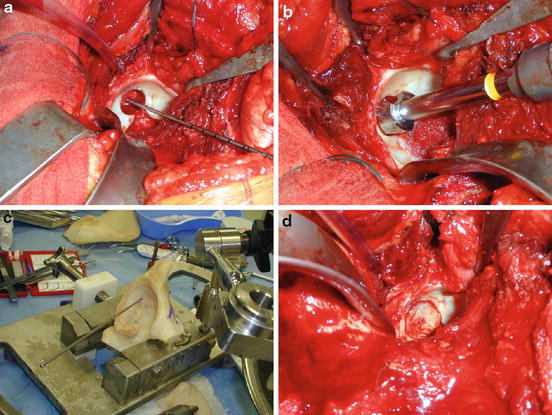
Fig. 3
Intraoperative photograph demonstrating the use of an acetabular osteochondral allograft for an acetabular articular surface defect. (a) A cylindrical drill is used over a guidewire to prepare the recipient site. (b) Recipient site after preparation. (c) Graft table setup shows donor acetabulum with guidewire in place. Note the reference points on the donor acetabulum used to match the location of the donor and recipient sites. (d) Press-fit graft placement, reconstituting the articular surface of the acetabulum (Reproduced from Krych AJ, Lorich DG, Kelly BT. Treatment of focal osteochondral defects of the acetabulum with osteochondral allograft transplantation. Orthopedics. 2011 Jul;34(7):e307–11., with permission from SLACK, Inc)
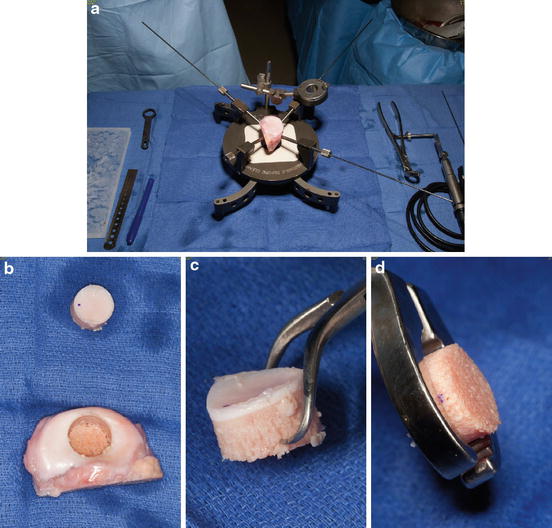
Fig. 4
Intraoperative photographs demonstrating the use of a medial tibial plateau to fill an osteochondral defect. (a) Graft table setup. (b) Osteochondral dowel after harvest. (c) Osteochondral dowel profile demonstrating best fit contour to match the recipient site. (d) Fine-tuning the depth of the osteochondral dowel to ensure the donor graft matches the recipient site
Postoperative Care
The postoperative course begins with the implementation of continuous passive motion (CPM) immediately after surgery. Throughout the first 8 weeks after surgery, CPM is advised for 8–10 h per day. Weight bearing is restricted to toe touch for the first 8 weeks postoperatively with a gradual advancement to weight bearing as tolerated allowed from that point onwards. After 6 months (OAT) to 12 months (OCA), MRI of the hip is obtained, and if graft incorporation is demonstrated, impact activities including running may be resumed.
Outcomes
Limited clinical data exists regarding the use of OAT and OCA in the treatment of chondral defects of the hip. These data are summarized in Table 1. While preliminary data is promising in some of the more recent series, further studies are needed to verify the long-term viability of these techniques for hip preservation surgery.
Table 1
Literature review
Authors/year | LOE | Defect location | Etiology | Patient characteristics | Procedure | Approach | Outcome measures | Follow-up | Results/conclusion |
|---|---|---|---|---|---|---|---|---|---|
Meyers et al. [22] | 4 | Femoral head | AVN | 21 hips in 20 patients | Fresh OCA | Gibson | d’Aubigne and Postel hip scores | Min.18 months | 71 % success rate overall (15/21)a |
Age: 18–44 years | Grafts composed of osteochondral shell with underlying iliac crest bone chips | 50 % success rate with steroid-induced AVN (4/8) | |||||||
Donor: allograft femoral head | 85 % success rate in nonsteroid group (11/13) | ||||||||
Meyers [23] | 4 | Femoral head | AVN, femoral head fracture | 25 hips in 21 patients | As above | Gibson | None reported | 9–63 months | Follow-up study |
Age: not reported | 68 % success rate overall (17/25)b | ||||||||
80 % success rate in nonsteroid group (12/15) | |||||||||
Meyers [26] | 4 | Femoral head | AVN, post-traumatic | 75 hips in 72 patients | As above | Gibson | None reported | Min. 1 year | Success not defined |
Age: 16–46 years | 80.5 % successful at 1 year | ||||||||
13 failed and had THA within 1 year | |||||||||
Hart et al. [17] | 4 | Femoral head | Intra-articular screw placement for acetabular fracture fixation | 1 patient | Mosaicplasty | Kocher-Langenbeck | HHS | 6 months | HHS |
Age: 28 years | Defect size: 14 mm diameter | Preoperative 69 | |||||||
Donor site: lateral condyle of femur | Postoperative 100 | ||||||||
Number of plugs: 4 | |||||||||
Rittmeister et al. [10] | 4 | Femoral head | AVN | 5 Patients | Mosaicplasty | Smith-Peterson | THA as endpoint | Mean 57 months | 4/5 cases failed with THA performed at a mean of 49 months |
Age: 34–51 | Defect size: 1.4–9.0 cm2 | 1/5 cases successful. 36-year-old with smallest defect: 1.2 × 1.2 cm | |||||||
Donor site: ipsilateral femoral head, ipsilateral knee | HHS | ||||||||
Number of plugs: 1–3 | Postoperatively 100 | ||||||||
Sotereanos et al. [14] | 4 | Femoral head
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





