Grade
Amount of fat within muscle
0
Normal muscle
1
Some fatty streaks
2
More muscle than fat
3
Equal amounts of muscle and fat
4
More fat than muscle
Grade | Percent fat in muscle |
|---|---|
0 | Normal muscle |
1 | <25 % |
2 | 25–50 % |
3 | 50–75 % |
4 | 75–100 % |
In patients with abductor deficiency in the absence of radiographic or imaging findings, SGN palsy can be diagnosed and followed with electromyography (EMG). Close observation is encouraged as 95 % of patients are expected to spontaneously recover by 24 months post-THA. Serial EMG is a useful tool for the assessment of patient recovery during this time [33].
Surgical Management
Depending on the type and degree of abductor deficiency, different abductor repair or transfer techniques are warranted. The main indication for anterior gluteus maximus transfer is abductor deficiency secondary to loss of gluteus medius and minimus in the presence of a normal functioning gluteus maximus [13]. The current author’s indication for gluteus maximus transfer is massive gluteus medius and minimus tears with greater than 50 % fatty infiltration or failed primary repair of gluteus medius and minimus tendons with a normal gluteus maximus muscle. Fortunately, gluteus maximus function is spared in most cases of abductor deficiency. Though large studies have yet to be conducted, anterior gluteus maximus transfer is believed to be particularly useful in patients with severe destruction of the abductor mechanism. This is often seen in patients with abductor avulsion, as well as osteolytic and inflammatory damage secondary to THA and THA revisions [9, 13]. Surgical reattachment of avulsed abductors is often difficult, and inflammatory destruction secondary to THA metal-on-metal hypersensitivity often results in complete loss of abductors and capsular instability. In these cases, anterior gluteus maximus transfer can restore stability and abductor function.
The anterior gluteus maximus originates at the anterior half of the iliac crest, and in hip extension, its fibers are positioned parallel to the femoral shaft. Since its SGN innervation enters the muscle proximally and posteriorly, the anterior detachment from the fascia lata during flap creation limits iatrogenic nerve damage [13, 34]. In the technique described by Whiteside [13], the anterior half of the gluteus maximus is transferred to the proximal femur and attached underneath the vastus lateralis. In cases of more severe deficiency of gluteus minimus and posterior capsule, a second triangular flap from the posterior gluteus maximus can be transferred under both the greater trochanter and the primary flap to the anterior capsule. This partially compensates for absence of short external rotators and posterior instability and is the subject of the surgical technique section.
In cases where the greater trochanter is displaced from the remaining bone stock but still has abductor attachments, a posterior gluteus maximus transfer technique can be used. Whiteside et al. [13] note that in most cases of tendon or greater trochanter avulsion associated with THA, surgeons cannot reattach the gluteus medius and minimus to the femur. Moreover, the abductor muscles and hip capsule may be completely absent in cases of destructive inflammation associated with failed THA [13]. In this technique, a triangular muscle flap from the middle posterior gluteus maximus is created, without disrupting the tendon insertion, and used to span the gap between the displaced greater trochanter and the remaining bone stock [20]. When indicated, this procedure can increase abduction and pelvic stability but often coincides with decreased range of motion. However, this posterior transfer technique cannot be used in cases of severe abductor deficiency or absence secondary to osteolytic degradation or prolonged displacement of the greater trochanter [13, 20]. Without gluteus medius or minimus attachment to the greater trochanter or proximal femur, complete abductor substitution is necessary [13]. In these cases, anterior gluteus maximus transfer would be more useful.
Other surgical options for less severe abductor deficiency include direct transosseous repair with or without incorporation of fascia lata and Achilles tendon allograft. These procedures have been met with mixed results [1, 7–10]. The authors’ preferred technique includes a gluteus maximus transfer using a docking technique with double-row fixation with suture bridge.
Surgical Technique
The patient is placed in the lateral decubitus position. The greater trochanter is outlined with an incision that begins 3 cm proximal to the tip of the greater trochanter and extends 3 cm distally (Fig. 1). Sharp dissection is performed down to the fascial layer of the iliotibial band, which is then incised just distal to the iliac crest to the level of the greater trochanter. A flap is created in the posterior aspect of the gluteus maximus and mobilized (Fig. 2). A second flap is made just distal to the first to recreate the short external rotators. After adequately mobilizing these flaps (Fig. 3), two sets of Krackow stitches (No. 2 FiberWire, Arthrex, Naples, FL) are placed in each flap. If the gluteus medius tendon appears to be torn and retracted, a primary repair of the tendon can also be performed in addition to the gluteus maximus transfer. The greater trochanter is decorticated with a 4.0 mm oval burr (Stryker, Kalamazoo, MI) that is then used to create a trough within the greater trochanter (Fig. 4). The burr is placed on the tip of the greater trochanter over the superoposterior and lateral facets and directed approximately 45° away from the lateral cortex. Two drill holes are created to communicate with the posterior aspect of the trough and allow the sutures from the gluteus maximus flap to dock into the bone trough. Two additional drill holes are placed on the anterior aspect of the trough so that there are a total of four drill holes. Passing sutures are placed through the drill holes, and a suture loop will exit through the trough entry. Once this is completed, the hip is placed in an abducted position. Two suture anchors (4.5 Bio-Corkscrew, Arthrex, Naples, FL) are placed on the medial border of the gluteus medius footprint to primarily repair the gluteus medius and, in some cases, the gluteus minimus tendons. The Krackow sutures are passed into the trough via the passing sutures, and the initial gluteus maximus flap is docked into the bone trough and subsequently tied over a bone bridge (Fig. 5). Stitches from the suture anchors are passed through the flap, and these sutures with those tied over the bone bridge are subsequently incorporated into a lateral row suture anchor (4.5 SwiveLock, Arthrex, Naples, FL).

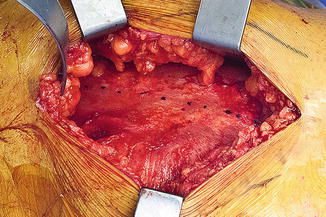

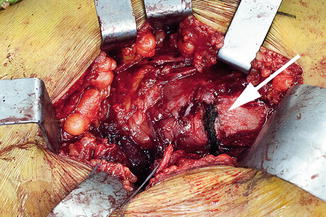

Fig. 1
The greater trochanter is outlined with a 6–8-cm incision centered at the tip of the greater trochanter
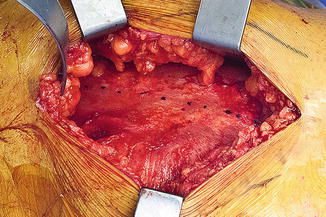
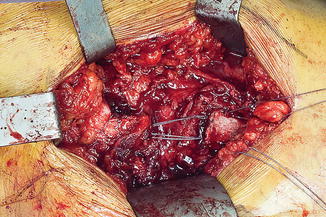
Fig. 2
The gluteus maximus is visualized. The incisions are marked for the posterior flap (dotted line) as well as the flap for the short external rotators (solid line)

Fig. 3
The flaps are fashioned and mobilized. Once this is completed, two sets running Krackow sutures are placed in each flap
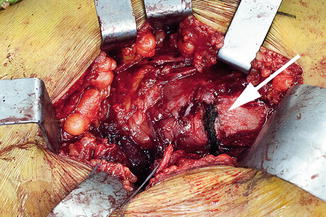
Fig. 4
A bone trough (arrow) is developed in the greater trochanter so that the gluteus maximus flap can be docked into the bone trough and tied over a bone bridge