Fig. 1
Synovial chondromatosis, a condition of synovial metaplasia with four or more osteochondral loose bodies
These loose bodies, which are either ossified or non-ossified, can become trapped in the acetabular fossa and gutter and cause pain (Fig. 2). The number within each joint may range from a handful to hundreds, and their removal may consequently be a challenge. Nevertheless, an organized and efficient approach that optimizes access, visualization, adequate joint distraction, and appropriate instrumentation for addressing central and peripheral compartment lesions will minimize potential difficulties. Recent improvements in technique and instrumentation have made hip arthroscopy an effective way to diagnose and treat synovial chondromatosis [9] and a variety of other intra-articular problems. Many hip disorders that are now managed arthroscopically previously were undetected and therefore untreated.


Fig. 2
Radiographic and magnetic resonance imaging showing loose bodies in the hip joint
Technical Pearls
Arthroscopy can be done supine or lateral; and the latter is preferred by the senior author. With the patient in the lateral decubitus position, a dedicated hip distractor (Innomed Corp, Savannah, GA) is applied to the well-padded leg and ankle (Fig. 3). A regular fluoroscopic table is necessary. The patient must be carefully padded at the perineum to avoid neuropraxic injury.


Fig. 3
A dedicated hip distractor with the patient in the lateral decubitus position (Innomed, Savannah, GA)
Position and Joint Distraction
The femur is placed in slight flexion (approximately 10–20°), with the foot in neutral or slight external rotation. Positioning the hip greater than 20° can translate the sciatic nerve anteriorly, bringing it into danger with the inserting trocar. Excessive external rotation of the femur will also move the greater trochanter posteriorly, making it more likely to deflect the inserting trocar toward the sciatic nerve. The well-padded perineal post is perpendicular to the long axis of the thigh, 10–15 cm distal to the ischial tuberosity. This distal placement of the post avoids pressure on the pudendal nerve and allows a cantilever effect on the proximal femur when traction is applied to lift the femoral head up from the medial wall of the acetabulum and over the transverse acetabular ligament [10]. After skeletal muscle relaxation but prior to skin preparation, fluoroscopy is used to determine the degree of distraction required. Axial distraction is applied with the leg abducted, usually between 0° and 20°, depending on the patient’s neck-shaft angle and the depth of the acetabulum. Adequate visualization and cannula insertion require the femoral head to be distracted at least 7–10 mm between the articular surfaces. If distraction is suboptimal, visualizing and maneuvering of instruments within the joint will be challenging, and unexpected loss of traction can further lead to articular damage and instrument breakage. Traction should be less than 1 h at a time for the central compartment. Peripheral compartment surgery is performed without distraction. The distractor is subsequently relaxed after adequate distraction has been confirmed via fluoroscopy. Standard skin preparation and draping would follow.
Once the spinal needles are inserted into the joint, and joint fluid is aspirated to confirm proper location. A blunt, conically tipped trocar is then inserted for controlled penetration of the hip capsule to create an arthroscopic portal. Portal placement requires palpation, identification, and marking of the anatomic landmarks, especially the femoral neurovascular bundle. The procedure may require two or more portals: direct anterior, anterior paratrochanteric or anterolateral, proximal trochanteric, superior paratrochanteric or posterolateral, and direct posterior have all been well described [11]. The superior paratrochanteric portals pass through fewer muscle planes and minimize chance of injury to the lateral femoral cutaneous nerve; these portals also allow the trocars to puncture the superior hip capsule which is thinner. The senior author prefers the anterior and superior paratrochanteric portals initially [12], as they allow visualization of the entire articular portion of the joint in 95 % of cases (Figs. 4 and 5). After the portals are established, the hip is distended with normal saline to overcome the joint’s native intra-articular negative pressure. Pressure-sensitive high-volume lavage is required for optimal visualization.

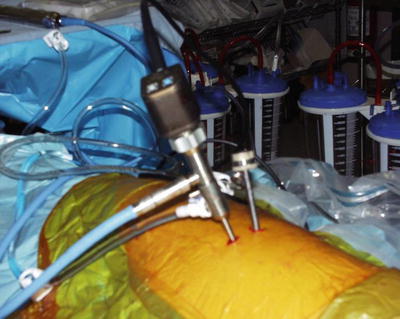

Fig. 4
The senior author’s (JCM) preferred arthroscopic portals: anterior superior paratrochanteric portal, which gives excellent visualization of the femoral head, anterior neck, anterior labrum, and synovial tissues beneath the zona orbicularis, and the posterior superior paratrochanteric portal, used for viewing the posterior capsule, posterior labrum, and posterior femoral head
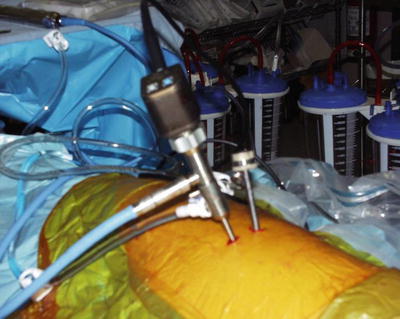
Fig. 5
The senior author’s (JCM) preferred arthroscopic portal sites with the patient in the lateral decubitus position
The Hip Joint
The hip joint has both intra-articular (or central) and peripheral compartments. Hip pathology is often found within the intra-articular region. The peripheral compartment, which is intracapsular but extra-articular, may also contain lesions which are overlooked with traction alone because synovial disease frequently involves the capsule, and loose bodies may therefore sequester in the peripheral recesses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








