Fig. 1
Frog leg radiograph demonstrating a severe acute SCFE slip
A second classification system developed for the presentation of SCFE was proposed by Loder et al. and has seen widespread acceptance and utilization. The Loder classification describes patients as having either stable SCFE, in which a child is willing to bear weight – with or without the presence of a limp – or unstable SCFE, in which there is refusal to bear weight. Importantly, the rates of avascular necrosis (AVN) of the hip have been clearly correlated with stability, with unstable SCFE having a 47 % rate of subsequent AVN, compared with no cases of AVN in stable SCFE in his study [5].
Pathoanatomy
Slipped capital femoral epiphysis accurately describes the disease process in which the structural integrity of the proximal femoral physis is compromised, leading to the epiphysis remaining reduced within the acetabulum, while the pull of the hip flexors displaces the proximal femoral metaphysis anteriorly. The resulting deformity leads to a loss of sphericity of the femoral head-neck junction, thereby decreasing the head-neck offset (Fig. 2). This is described by the alpha angle (Fig. 3a–b). A cam lesion forms at the anterosuperior head-neck junction of the proximal femur and impacts the acetabular rim in flexion and internal rotation. Alpha angles greater than 60° describe cam lesions that have been associated with a greater degree of labral and articular cartilage damage [6]. SCFE severity is generally described by the degree of slippage or the slip angle, described by Southwick [7]. The slip angle is formed by the long axis of the femoral neck and a line perpendicular to the physis and bisecting the epiphysis. Angles are measured on Dunn lateral, or frog leg lateral radiographs are categorized as mild (0–30°), moderate (30–60°), or severe (>60°) (image) [8]. Alternatively, the alpha angle may be measured on axial MRI or low-dose CT scan if hardware artifact impedes measurement on MRI. Rab et al. performed computer modeling of SCFE cases, demonstrating that even mild slips lead to impaction of the proximal femur against the acetabular rim, and patients walk with increasing degrees of external rotation with increasing slip angle to prevent impingement with ambulation alone [9]. Leunig’s intraoperative findings confirm that patients with even mild slips and less than 3 months of symptoms all had some degree of labral damage [10]. With SCFE, two types of impingement may occur. Minor slips, and those that have remodeled to smaller cam lesions, may lead to “inclusion” type impingement. This occurs when the prominent metaphyseal region enters the hip joint with range of motion, increasing shear forces across the articular cartilage. On the other hand, moderate and severe slips have greater metaphyseal prominence at the femoral head-neck junction that limits range of motion, and the lesion impacts the acetabular rim rather than entering the joint. This type of impingement is known as “impaction” impingement and leads to labral derangement and levering of the femoral head posteriorly in acetabulum resulting in countercoup impaction of the femoral head against the posterior acetabulum [8, 11–13]. The natural history of untreated SCFE or in situ pinning without addressing the underlying deformity may lead to the development of arthrosis in a proportion of patients. Some degree of arthrosis was reported in 92 % of patients at an 11-year follow-up in one study [14], with another report of approximately 5 % of patients requiring a total hip arthroplasty by 16 years of follow-up [15].
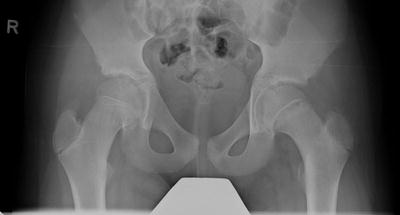
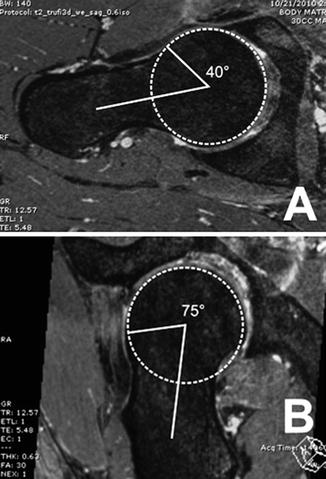
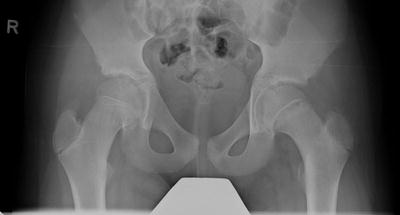
Fig. 2
AP radiograph illustrating a mild SCFE slip with CAM impingement
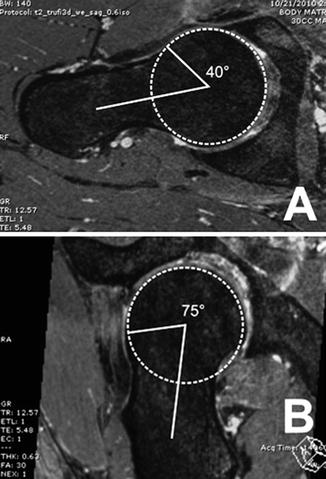
Fig. 3
Hip radiographs illustrating (a) normal and (b) abnormal alpha angles
Indications
Patients with symptomatic femoral acetabular impingement (FAI) from a chronic, stable SCFE may be amenable to treatment with arthroscopic proximal femoral osteoplasty to increase the proximal femoral head-neck offset. Surgical dislocation and open proximal femoral osteoplasty remains a viable and, often times, preferable approach for more significant deformity resulting from severe slips [10, 16, 17]. Femoral neck osteoplasty allows for greater range of motion without pathological abutment of the prominent metaphyseal deformity against the acetabular rim. Patients with chronic slips may simply complain of decreased range of motion as compared to the contralateral side, rather than joint pain [4]. Pain with activities or positions that place the hip in high flexion are common. Intra-articular derangement often presents with pain radiating to the groin or thigh, as well as referred pain to the knee. Patients may demonstrate the “C-sign,” as described by Byrd [18], when discussing their pain. Notably, some patients may be asymptomatic, but may have radiographic or MRI evidence of a labral tear or early acetabular cartilage delamination or degeneration. Given the natural history of this disease process, arthroscopy with the goal of joint preservation, removal of the offending bony lesion, and repair or debridement of damaged labral tissue is a reasonable surgical option.
Patients with mild chronic SCFE (slip angle <30°) may have alterations in joint biomechanics significant enough to create chondral and labral derangements due to inclusion impingement [10]. Joint space narrowing, signs, and symptoms of arthrosis may be evident clinically and radiographically. The earliest sign of arthrosis may currently be detected on delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC). This study utilizes indirect contrast enhancement of articular cartilage by intravenously administered gadolinium. Gadolinium is a negatively charged element that binds to positively charged glycosaminoglycans (GAG) that comprises the matrix of articular cartilage. Areas of early arthrosis will have a relatively lower concentration of GAG and, thus, less contrast enhancement. Zilkens et al. studied 32 hips with varying severity of SCFE (10 mild, 22 moderate) treated with in situ pinning, on average 11 years prior to dGEMRIC imaging [19]. The authors correlated postoperative alpha angles with dGEMRIC findings. Though 85 % of the hips were Tonnis grade 0, showing no signs of joint space narrowing, those with alpha angles >60° did have significantly decreased gadolinium uptake and therefore greater early cartilage degeneration than those with normal proximal femoral head-neck offset (alpha angle <50°). The subset of patients in this study with alpha angles >60°, meeting FAI criteria, had a mean Harris Hip Score greater than 95, yet had degenerative changes on dGEMRIC. While patients with chronic, stable SCFE or those post-pinning with residual decrease in head-neck offset may be asymptomatic, subtle degenerative changes in the articular cartilage may be occurring. This may set the cascade of degenerative joint disease in motion. The goal of hip arthroscopy after SCFE is to restore the head-neck offset (alpha angle <50°) to prevent, or slow, these changes (Fig. 4a–b).


Fig. 4
Radiographs demonstrating a CAM deformity after SCFE treatment. (a) AP radiograph and (b) lateral Dunn radiograph
Provided adequate healing of any acute or unstable SCFE lesion has occurred, hip arthroscopy need not be delayed until skeletal maturity, as the technique has been shown to be a relatively safe procedure and effective approach for skeletally immature patients. Cam lesions typically develop at the level of the proximal femoral physis in the skeletally immature patient and can been safely debrided [20, 21]. No cases of physeal separation, growth arrest, femoral neck fracture, or AVN have been described after hip arthroscopy in the skeletally immature patient [22–25].
In summary, the indications for hip arthroscopy in patients after in situ pinning or untreated residual SCFE with uncorrected deformity may include symptomatic FAI, decreased range of motion, pain with activities that place the hip in high flexion, early degenerative changes on plain films or dGEMRIC imaging, and/or evidence of intra-articular derangement including labral and articular cartilage lesions. Contraindications to hip arthroscopy for chronic SCFE include significant arthrosis (joint space <2 mm), concomitant hip dysplasia, patient who are incapable of complying with the postoperative rehabilitation regimen, and severe SCFE, which may be better treated with open intertrochanteric osteotomy.
Technique
Setup and Diagnostic Arthroscopy
Hip arthroscopy is most commonly performed in the supine position on a traction table. A well-padded, large circumference pudendal post is placed between the legs, and the patient’s feet are placed in well-padded boots at the end of the traction table. Typically 50–75 lbs of traction is applied, or enough to distract the hip 1 cm and observe a vacuum sign within the joint. Fluoroscopy is utilized to confirm joint distraction and the beginning of traction time is noted. The first portal is placed using anatomic landmarks and fluoroscopy assistance. A spinal needle is placed into the joint either from the anterolateral or posterolateral portal entry site. The negative pressure of the joint under traction will create an air arthrogram on fluoroscopy if the needle is within the joint. Other portals utilized include the accessory mid-anterior, direct anterior, and Dienst portals. The Dienst portal is located in the soft spot 1/3 of the way between the ASIS and the greater trochanter [26]. Typically, two to three portals are utilized. A flexible, blunt-tipped guide wire is inserted through the spinal needle, and its placement at the medial wall of the acetabulum is confirmed with fluoroscopy. The needle is removed over the guide wire, and a cannula with obturator is placed over the guide wire into the joint, taking care not to entrap the labrum. The position again is checked with fluoroscopy and the 70° arthroscope inserted in the scope cannula. The joint is insufflated with saline with the arthroscopic pump set at 45–60 mmHg, on average. The second portal is made under direct arthroscopic visualization within the central compartment, in a similar fashion to the first portal placement. Given the limitations in motion that often occur with SCFE, and postoperative changes after pinning, the joint capsules tend to be thick and stiff. Maneuverability within the joint is facilitated by establishing and extending an anterolateral capsulotomy with an arthroscopic beaver blade and shavers (Fig. 5a–c).
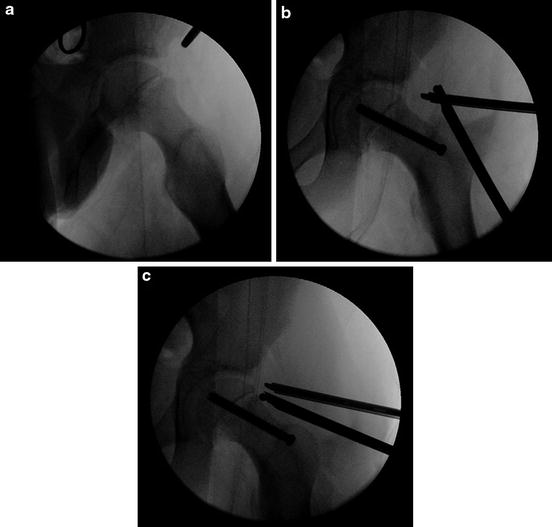
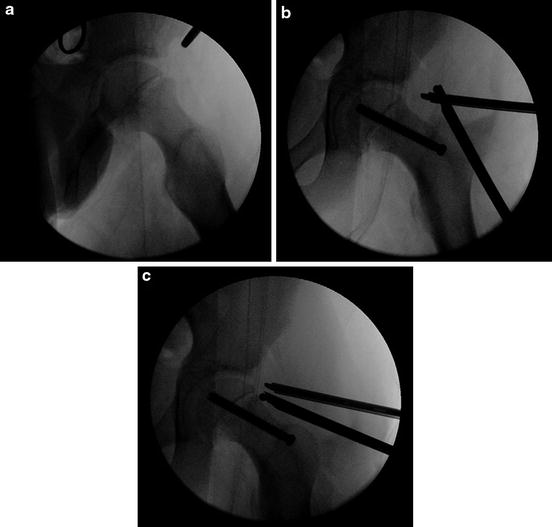
Fig. 5
Intraoperative fluoroscopy images illustrating a chronic SCFE slip with CAM lesion. (a) Frog leg images demonstrating a mild SCFE slip with CAM lesion prior to pinning and arthroplasty. (b) Pinned hip. (c) Pinned hip with femoroplasty
Central Compartment
A diagnostic arthroscopy of the central or articular compartment is performed. The second portal allows for probing of the labrum, acetabular and femoral articular cartilage, and ligamentum teres. Patients with large cam lesions secondary to chronic SCFE should have the integrity of the labrum and acetabular cartilage closely scrutinized. In the case of a labral tear, a third portal can be made if necessary as a distal accessory portal to facilitate an appropriate vector for anchor placement and suture passage. The labrum can be elevated from the acetabular rim sharply or recessed subperiosteally as described by Martin [27], theoretically preserving the blood supply to the labrum. If the structure of the labrum is preserved, yet it is separated from the chondrolabral junction, a repair is pursued rather than debridement. After preparing the acetabular rim creating a bleeding bony surface with an arthroscopic shaver or burr, enough anchors are placed to adequately reattach the torn portion. Nonabsorbable sutures from the anchors are passed either around the labrum encircling it or through the labrum in a mattress fashion and tied, reapproximating the labrum to the bleeding acetabular rim. Patients with post-SCFE impingement, whether resulting from untreated and healed slips or residual deformity after pinning, often develop articular cartilage changes. Acetabular cartilage delamination often accompanies labral damage at the anterosuperior acetabular articular margin and can be addressed with chondroplasty or microfracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








