Fig. 1
Shows a left femoral head fracture with displaced suprafoveal weight-bearing osteochondral fragment (With permission from Orthopedics Today)
Preoperative Planning
Experience
Arthroscopic osteosynthesis of femoral head and acetabular fractures is technically challenging. One should assess his/her personal and surgical team’s experience and ability to perform these procedures in a safe manner.
Game Plan/Contingencies
Fixate critical fragments that contribute to weight-bearing articular congruency (Fig. 2) and/or structural integrity but consider removal of others. If one decides to perform arthroscopic osteosynthesis, a contingency plan is recommended in case the procedure does not proceed as planned. It is better to convert to an open osteosynthesis than perform an inadequate arthroscopic reduction and/or fixation. Keep in mind the general principle of anatomic reduction with secure internal fixation permitting early joint motion. Resection, even arthroscopic, of a critical weight-bearing or structural fracture fragment is the last option if all reasonable attempts at arthroscopic or open osteosynthesis fail.
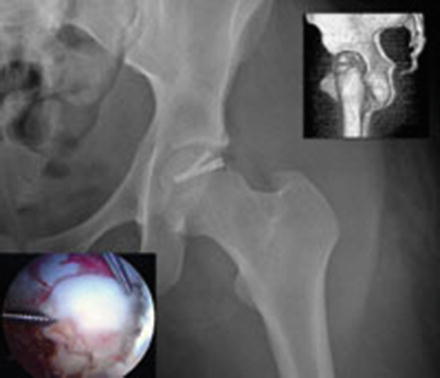
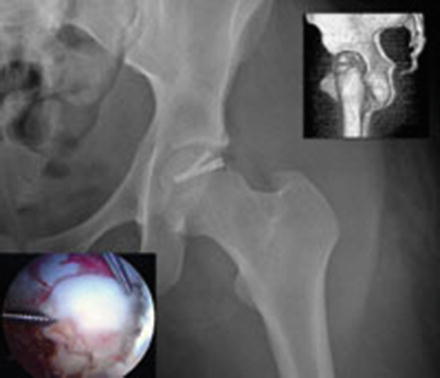
Fig. 2
Shows the same fracture during arthroscopic reduction using the chopstick maneuver (lower left) and postoperative imaging (With permission from Orthopedics Today)
FAI Considerations
Acetabular overcoverage from pincer FAI may prevent an acceptable angle of approach for screw fixation of the fracture fragment(s). In such instances, adjunctive arthroscopic acetabuloplasty of the overcovered femoral head may enable successful arthroscopic fixation with headless screws [7] (Fig. 3, 4, 5, and 6). Note that one must not cause iatrogenic dysplasia by overzealous rim trimming and the labrum should be preserved, typically with refixation. Cam FAI, even if previously asymptomatic, may be addressed with arthroscopic femoroplasty without traction as a potentially prophylactic measure. Finally, if a fracture fragment involves a region of cam morphology, resection of that fragment may improve structural offset in that region.
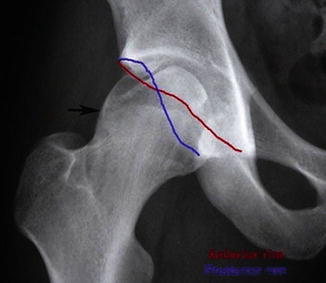
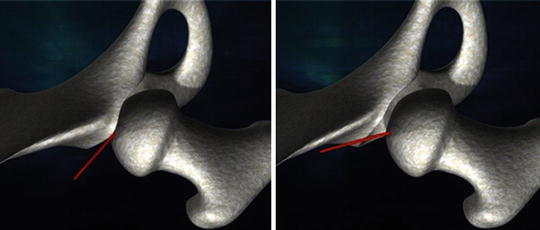
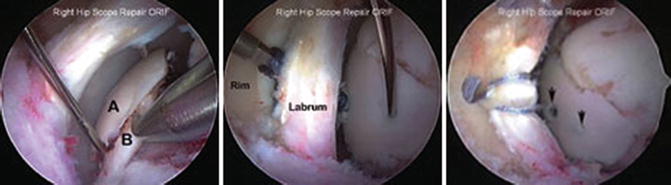

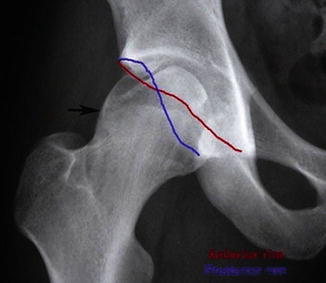
Fig. 3
Is a detail of a preoperative AP pelvis radiograph showing a double-density shadow of a clamshell suprafoveal femoral head fracture seen after emergent closed reduction of anterior dislocation (Brumback type 4B). Note cam (arrow) and pincer FAI with focal acetabular overcoverage and crossover sign (With permission from Elsevier Arthroscopy Journal)
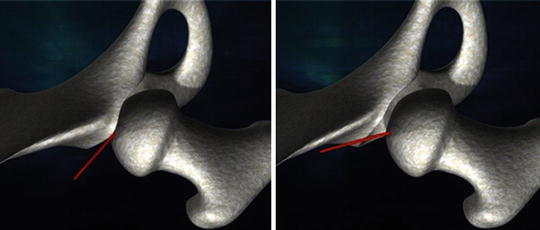
Fig. 4
Depicts screw path (red line) before (left) and after (right) arthroscopic acetabuloplasty. A more perpendicular trajectory for screw fixation is achieved (With permission from Elsevier Arthroscopy Journal)
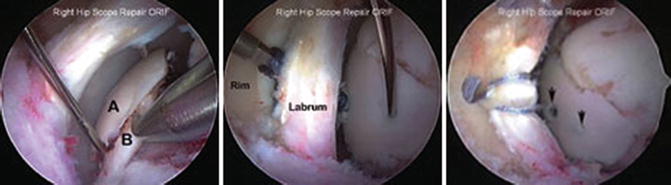
Fig. 5
Shows the clamshell fracture with folded osteochondral fragment with superior (a) and inferior (b) fragments being pried apart with microfracture awl (left). The reduced fracture is being fixated with cannulated headless compression screws (middle). The acetabular rim has been trimmed and the labrum preserved with a screw being inserted between the structures to optimize screw fixation path. Arthroscopic labral refixation is then completed (right). Arrows indicate buried screw heads below chondral surface (With permission from Orthopedics Today)

Fig. 6
Shows postoperative healed femoral head fracture. Arrow indicates superolateral acetabuloplasty (With permission from Elsevier Arthroscopy Journal)
Consent
Consent should include arthroscopic and open osteosynthesis plus possible resection of fracture fragment(s). Arthroscopic acetabuloplasty, femoroplasty, and chondrolabral surgery with possible labral debridement, refixation, and reconstruction should be included as appropriate.
Equipment
Ensure that the fracture table and/or portable hip distractor provides sufficient freedom of hip motion for hip positioning and dynamic testing and does not obstruct fluoroscopic visualization of the operative hip on anterior–posterior and lateral projections. Even if one does not routinely use fluoroscopic guidance for hip arthroscopy, a C-arm image intensifier is strongly recommended and is very helpful, especially when using metallic (radiopaque) screws (see below). A cannulated headless screw system is needed. These systems vary in their specific instructions so it behooves one to become familiar with the chosen system.
Setup
Although lateral position hip arthroscopy is an option, supine hip arthroscopy will be described. Position the image intensifier between the abducted legs enabling AP, lateral, and dynamic fluoroscopy. The operative hip is positioned in 10° flexion, 20° abduction, and 30+ degrees of internal rotation.
Consider using the fluoroscopic templating technique [9] especially in cases where one anticipates possible acetabular rim trimming. Moreover, pelvic positioning is standardized by aligning the pelvis to the vertical beam of the C-arm in frontal and sagittal planes prior to commencement of surgery.
Traction
A detailed preoperative assessment of sciatic function is important as there is a relatively high incidence of sciatic injury associated with trauma from hip dislocations.
Remain vigilant of traction time AND force [10]. Limit the amount of hip distraction to 10 mm of actual space between the acetabular and femoral head chondral surfaces during central compartment arthroscopy. Rather than over-distract, consider hip adduction along with adjustments in hip rotation to permit acceptable screw trajectory. The use of a traction “time-out” for every hour of applied traction is prudent. Concurrent procedures requiring no traction (e.g., femoroplasty) may be performed during this time.
Portals
The anterolateral portal (ALP) and the modified midanterior portal (mMAP) [21] are used. The latter is typically 3 cm anterior and 4–5 cm distal to the ALP and is made in the aforementioned internal rotated hip position. Typically, a 70° arthroscope permits sufficient visualization from the ALP and the mMAP is the working portal, although occasionally interportal exchange is needed.
A vertical line passing through the anterior superior iliac spine (ASIS) along the operative thigh is a landmark beyond which one should not stray medial to minimize risk of inadvertent neurovascular damage. Percutaneous passage of guide pins and cannulated screws should remain lateral to this landmark whenever possible.
Fluid Pressure
Minimizing arthroscopic fluid pressure minimizes the risk of inadvertent abdominal compartment syndrome. With hypotensive anesthesia, fluid pressure of 50 mmHg is often sufficient for adequate arthroscopic visualization. In some cases, even “dry” arthroscopy may be considered. Intermittent palpation of the draped abdomen, monitoring of hemodynamics and core body temperature, and, if indicated, iliopsoas release at the conclusion of surgery are prudent precautionary measures [11]. Intentional removal of intra-articular debris should be performed in hopes of minimizing third body wear; a suction-shaver and high-flow (but low pressure) arthroscopic irrigation may expedite this step and should be repeated at the conclusion of the surgery.
Arthroscopic Reduction
Although closed reduction techniques can be used by manipulating operative hip position for minimally displaced fractures, significantly displaced fractures typically require arthroscopic reduction. A switching stick or probe may enable gross translation of the osteochondral fragment to the fracture site. If fragment derotation is necessary, one may use a toggle stick method; however, this violates the articular surface. The chopstick technique [6] (Fig. 2) uses two percutaneous guide pins with two points of chondral contact to aid in fragment derotation for arthroscopic reduction.
Arthroscopic Internal Fixation
Once fracture reduction is achieved, the guide pins used to enable arthroscopic reduction can then be used to provide transient fracture fixation. The percutaneous entry sites for these guide pins should enable an acceptable trajectory for cannulated headless screw fixation. Hip adduction in traction may facilitate arthroscopic screw fixation by exposing some femoral head fractures out from under the obstructive coverage of the acetabulum. Perfectly perpendicular screw fixation is not mandatory for successful fracture union; however, a relatively perpendicular position is desirable as it permits optimal engagement of the subchondral bone while seating the headless screw below the chondral surface. Current headless compression screw design compresses the fracture site with antegrade advancement. Typically two or three screws (Acutrak mini, Acumed, Hillsboro, Oregon) are required although this will vary with the size and thickness of the osteochondral fragment. Avoid overzealous antegrade screw advancement as this may lose subchondral purchase and compromise compression if one then decides to partially back the screw out in a retrograde manner.
Although radiolucent bioabsorbable implants may be used, an advantage of metallic headless screws is that their position may be monitored to detect even subtle joint encroachment via intraoperative fluoroscopy and postoperative radiographs [6]. If detected, one may perform arthroscopic screw removal or antegrade screw advancement. A relative disadvantage of metallic implants is unwanted scatter from computed tomographic and magnetic resonance imaging, although some scanners have metal-subtraction technology.
Dynamic Arthroscopic and Fluoroscopic Testing
Dynamic arthroscopic and fluoroscopic examinations confirm safe positioning of headless screws and also confirm absence or eradication of coexistent FAI. Static biplane fluoroscopy may not detect a proud screw violating the joint. Rotating the C-arm around the femoral head and moving the hip within the static C-arm are both acceptable methods, although the latter may permit more range of motion including internal and external rotation and may be quicker with less radiation exposure.
Postoperative Considerations
Early range of hip motion while protecting against excessive weight-bearing stress is desired. Typically 6–8 weeks of protected weight bearing of the operative hip with two crutches or a walker is sufficient. Exercise bicycling is permitted after 1 week and swimming (freestyle stroke) and jogging in a pool begin when portals are healed. Return to impact activity is individualized to the patient and his/her fracture, but even in the best case scenario, running is not begun until 3 months. Key pearls and pitfalls of arthroscopic femoral head osteosynthesis are provided in Table 1.
Table 1
Pearls for arthroscopic reduction and internal fixation of femoral head fractures
Perform accurate preoperative fracture assessment |
Perform accurate preoperative self-assessment of surgical experience and arthroscopic skills |
Be willing to perform possible open reduction–internal fixation (rather than arthroscopic fragment removal) if arthroscopic method fails |
Consider fluoroscopic templating technique to standardize pelvic position under hip distraction |
Hip adduction may improve path for screw fixation |
If pincer FAI, acetabuloplasty of overcoverage may improve path of screw fixation |
N.B. Do not cause iatrogenic dysplasia |
Pay careful attention to safe portal placement (may require several accessory portals), capsulotomies, intra-articular fluid pressure, and distraction amount and time
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





