Technique
Intraoperative Setup and Assessment
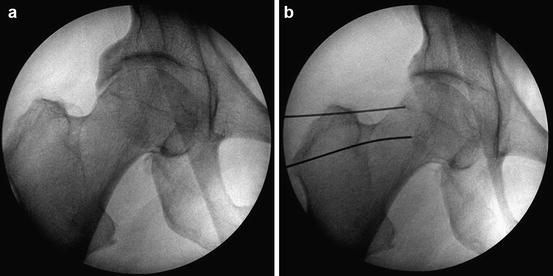
While both the supine and lateral position have been described, this chapter will discuss the supine position. Either a commercially available table attachments or a standard fracture table can be utilized to provide the distraction forces required to perform this procedure safely. Once anesthetized, an examination under anesthesia is performed to assess for hypermobility and to document preoperative range of motion with particular emphasis placed on the internal and external hip rotation at 90° and in extension. Well-padded boots and a well-padded offset perineal post are utilized to decrease the risk of neurologic injury [9]. The operative limb is placed into a position of slight hip flexion and roughly 15° of internal rotation to account for normal femoral anteversion and is placed in neutral abduction/adduction. Depending on the orientation of the pelvis after positioning, the operative bed may need to be tilted or “airplaned” with variable Trendelenburg/reverse Trendelenburg to achieve neutral pelvic tilt in order to create a fluoroscopic recreation of a well-centered preoperative AP pelvic radiograph. Once the patient is appropriately positioned and oriented, several fluoroscopic views of the hip are performed, a technique that has been described as an “around the world” assessment (Fig. 3). The hip is evaluated in neutral rotation and maximal internal and external rotation while both flexed and extended for a total of six views. This allows for an assessment of the medial and lateral femoral head-neck junction (hip extension) and anterior and posterior femoral head-neck junction (hip flexion).
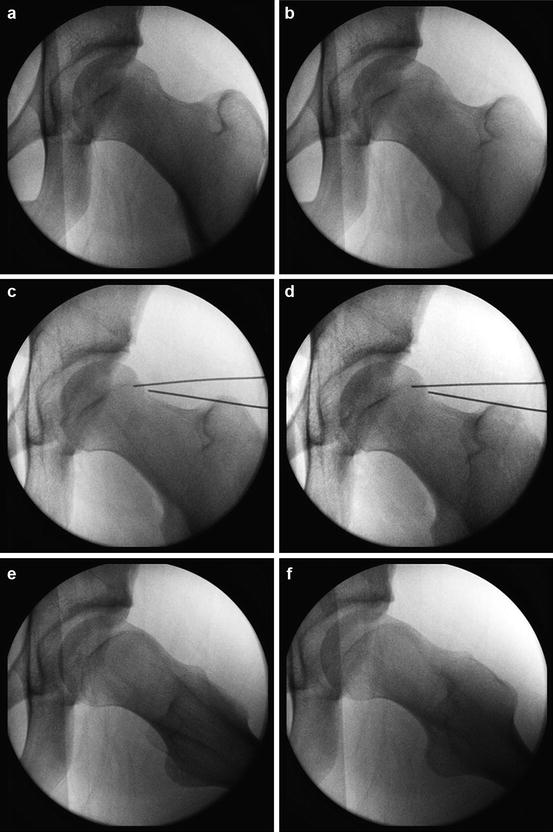
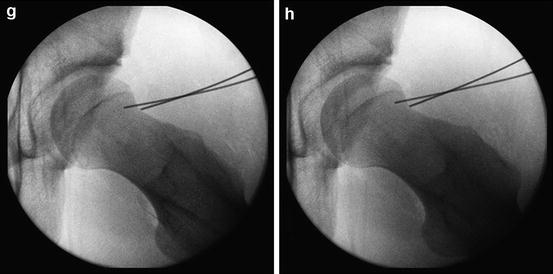
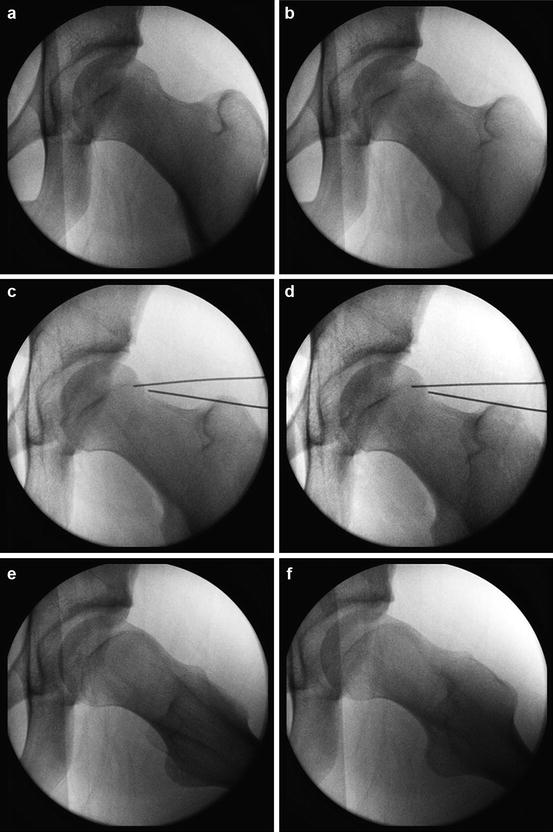
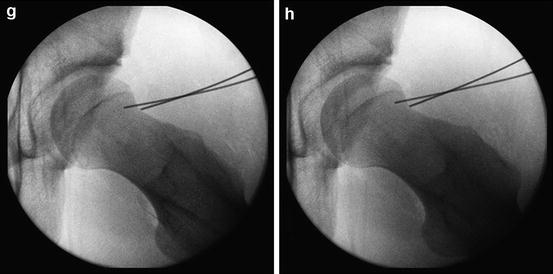
Fig. 3
Intraoperative pre-resection (a, b, e, f) and post-resection (c, d, g, h) AP and lateral fluoroscopic images demonstrate cam decompression
Surgical Technique
The hip is gradually distracted under fluoroscopy with care to avoid over-distraction and a goal of 8–10 mm of joint space opening. With excessively deep sockets or in the presence of large anterior/lateral acetabular fragments/overcoverage, it may be necessary to consider beginning in the peripheral compartment or outside the capsule and entering from an “outside-in” approach after a rim recession is performed. More commonly, a standard anterolateral (AL) portal is created beginning with a 16 gauge spinal needle and introduction of a cannula over a nitinol guidewire. A modified mid-anterior portal (MMA) is then created under direct visualization [10, 11]. Rarely a posterolateral (PL) portal will need to be created if a significant posterior rim recession is planned. During the diagnostic portion of the procedure, the clinical diagnosis of a pincer-type FAI is confirmed by the presence of labral ecchymosis, degeneration, ossification, posterior acetabular wear consistent with a contrecoup lesion, and an acetabular rim that extends well beyond the chondrolabral junction.
Labral preservation is preferred if possible and has been shown to have superior results to labral resection [2, 10]. If possible, the chondrolabral junction can be left intact as it can help to stabilize the labrum in a more anatomic position and more predictably results in a repair with maintenance of the labral seal (Fig. 4). When this technique is utilized, the leading edge of the acetabular rim is resected behind the labrum to achieve the desired level of resection. This technique is quite effective for focal anterior-based overcoverage. Alternatively a formal labral takedown can be performed sharply and the rim recessed and is more often used in the setting of greater degrees of overcoverage in order to resect excess acetabular articular cartilage allowing for better advancement of the labrum to the acetabular rim (Fig. 5) [6]. Using preoperative information including a 3D CT scan and the information gathered at the time of the diagnostic arthroscopy, the length and depth of the rim resection can be determined and can vary significantly between patients. Typically the amount of resection for focal overcoverage is between 3 and 6 mm in depth. When a deeper resection is necessary, it is helpful to occasionally release traction to assess for proper acetabular coverage as over-resection can lead to edge loading of the acetabular articular surface and the potential for iatrogenic dysplasia/instability.



Fig. 4
Rim recession depicted with chondrolabral junction left intact

Fig. 5
Rim recession with a formal labral takedown
For both techniques, the rim recession is performed with a motorized high-speed burr and the starting point for the resection is confirmed with fluoroscopy. Work is initiated through the modified mid-anterior portal and viewing through the AL portal and begins with the recession just inferior to the area of acetabular overcoverage seen on the fluoroscopic image. For more posterior resections the burr can be introduced though the PL portal and AL portal while viewing from the MMA and anterolateral portal. As the recession continues it is continually assessed with fluoroscopy to confirm the regions of the acetabulum being resected. A combination of direct visualization and intraoperative fluoroscopy allows for a more accurate resection in the current authors experience.
If a labral takedown has been performed, or if the amount of rim resected has led to a destabilization of the labrum, labral refixation is then performed at this point of the procedure. The number of anchors utilized will depend on the length of rim resected and is determined by the anatomy of the pincer lesion. Placement of the first anchor is at the more superior aspect of the labral takedown when more lateral rim resection is performed. This can be accomplished by drilling through the AL portal or alternatively a distal anterolateral portal (DALA) can be created to improve the angle for drilling allowing the surgeon to place the anchor as close to the acetabular rim as possible while not penetrating the articular surface. The DALA portal is localized in line with the standard AL portal and is between 2 and 3 cm distal to it. Otherwise, the anchors are placed from anteromedial to superolateral with anchors placed through the MMA portal and arthroscopic visualization via the AL portal. It is critical to place the anchor on the bony rim 1–2 mm off the articular margin in order to avoid eversion of the labrum, which will enable the surgeon to more accurately recreate the suction seal effect of the labrum (Fig. 6). With the anchor placed and tested for pullout, a tissue-penetrating device is used to place one limb of the suture between the acetabular rim and the labrum. When possible it is beneficial to then re-pierce the labrum and retrieve this suture creating a mattress-type or base refixation configuration for the repair. Some surgeons prefer to loop the suture around the labrum and currently there is no clear agreement about which technique is superior. Typically anchors are placed roughly 1 cm apart and will typically use 3 anchors for refixation, though for more extensive lesions between 5 and 8 anchors may be required. If there is associated AIIS/subspine impingement, the AIIS can be decompressed through the MMA portal and occasionally may be helpful to make an additional window through the direct head of the rectus femoral and capsular in order to preserve the capsular anteriorly (Fig. 7a, b). Rim fractures and/or os acetabula can typically be resected. In cases of fragments contributing to hip stability, however, arthroscopic-assisted cannulated screw fixation can be considered if the fragment is unstable (Fig. 8a, b).










