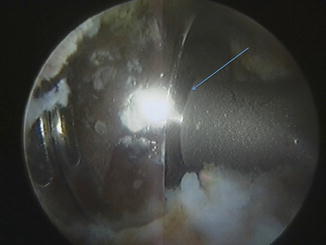
Fig. 1
An image intensifier picture of right hip joint showing the air shadow (blue arrows) along iliopsoas tendon course during iliopsoas air bursography (Arthroscopic image Courtesy Mr. Ali Bajwa)
The cross section of the iliopsoas at different levels delineates a higher tendon to muscle fiber ratio closer to its insertion [8]. The iliopsoas tendon-muscle complex at the level of the labrum, transcapsular iliopsoas release site in the peripheral compartment, and the level of the lesser trochanter is composed of 40 % tendon/60 % muscle belly, 53 % tendon/47 % muscle belly, and 60 % tendon/40 % muscle belly, respectively [9]. This has an implication on the site of iliopsoas tendon release or lengthening when it is planned arthroscopically.
Total Hip Arthroplasty and Iliopsoas Impingement
Iliopsoas impingement can occur in the native hip, the internal snapping of the hip. It has been well described as a cause of clunking and pain in the native hip joint. The presence of THA can predispose a patient to iliopsoas problems. These can result from dynamic or static issues [10]. As a result the implant position merits careful evaluation.
Static Issues
The implanted acetabular component may be relatively retroverted compared the native acetabulum. Likewise, the abduction angle may be more closed or reduced than the anatomical position. Both of the above factors bring into play the anterior and anterosuperior walls of the acetabular component, which may rub on the undersurface of the iliopsoas tendon as it glides across the hip joint [11]. Acetabular component malposition is particularly problematic in the uncemented hips, which have a metal edge on the acetabular implant and even more critical in hip resurfacing [12]. Likewise, the version of the femoral component has an impact on the position of the lesser trochanter in relation to the acetabulum, which in turn affects the mechanics of the iliopsoas tendon. The problem, as expected, is worse when position of both the components is compromised. In addition to version, the over sizing of the acetabular component or a large femoral head may increase the risk of iliopsoas impingement especially in hip extension phase of the gait [10].
Dynamic Issues
The dynamic problem of iliopsoas in association is poorly understood. Iliopsoas muscle group has predominantly red muscle fibers (slow twitch), thereby making it suitable for maintaining spinal posture [13] and controlled hip flexion [14]. Hence, if there is a deficit in the other muscle groups that contribute to posture, then iliopsoas pathology may result from overuse.
Clinical Assessment
Prior to undertaking arthroscopic surgery for iliopsoas pathology in the presence of THA, a full clinical evaluation is mandatory. It is ascertained that whether the onset of symptoms is following THA or lingering on from the preoperative period. Clinical examination typically reveals hip flexor irritability against resisted flexion but relatively pain-free passive range of motion. Occasionally, clunking or snapping can be elicited. Investigations are performed with two aims: Firstly, as a diagnostic tool to rule out implant loosening, infection, metal ion-related reaction, or referred pain and secondly, to confirm the iliopsoas pathology [11, 15]. The standard work-up will include full blood count (FBC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), cobalt and chromium ion levels in case of metal-on-metal articulation, dynamic ultrasound scan, metal artifact reduction sequence magnetic resonance imaging (MARS MRI), and plain radiographs in anteroposterior and cross-table lateral views. If iliopsoas pathology is visualized on imaging studies, a trial of ultrasound-guided steroid and local anesthetic is undertaken. This serves not only as a diagnostic test but occasionally is therapeutic when combined with a structured physical therapy rehabilitation program [16]. In selected cases where other causes of groin discomfort have been excluded and the diagnostic injection is positive but without sustained pain relief, an arthroscopic iliopsoas release is undertaken [15].
Arthroscopic Intervention
Arthroscopic intervention is planned under general anesthesia, intravenous antibiotic cover, and deep venous thrombosis (DVT) prophylaxis; however, the evidence for the latter is inconclusive. Based on the surgeon’s experience and preference, a lateral or supine position is used [11]. The patient is placed on Maquet table with a dedicated hip arthroscopy positioning system. The use of the hip arthroscopy distractor system enables superior patient positioning and protection of the pressure areas; however, no distraction is required for this procedure. The hip to be operated upon is on top in the lateral position. The knee joint is flexed to 40° and the hip joint flexed to 35° with 15° of abduction to relax the anterior hip capsule. After careful prep and drape, per-operative image intensifier views are obtained. A spinal needle (24G) is used to access the hip from the direct lateral side, an aspirate is attempted in case of an effusion; otherwise insufflation of the hip is carried out with 20–40 ml of normal saline. Next the access portals are established. The superior portal is 3 cm superior and 2 cm anterior to the tip of the greater trochanter (GT). The needle tip is directed to the neck of the femoral component to avoid scratching of the prosthetic articulating surfaces. In the case of a resurfacing hip arthroplasty, the needle is aimed at the implant-neck junction anteriorly. After confirmation of the access needle position under radiographic control, a guide wire is inserted followed by a 4.5 mm trocar and cannula system using Seldinger technique [17]. It requires careful visualization under image intensifier to avoid breakage of the guide wire since it may get trapped against the metal prosthesis or pushed against the scar tissue. The superior portal is used as the viewing portal. Anterolateral portal is next established 5 cm anterior and 2 cm distal to the tip of the greater trochanter. This portal is established under direct vision and 5.0 mm trocar-cannula system is used. This portal can be substituted for a distal anterolateral portal as required. An imaginary line is drawn perpendicularly distal to the anterior superior iliac spine (ASIS) and the anterolateral portal should not cross anterior to this line to avoid neurological damage [18]. Following access, the joint aspirate is collected for microscopy, culture, and sensitivity. This may be sent in aerobic and anaerobic culture bottles to decrease the risk of a false-negative result.
A radiofrequency probe is inserted from the working portal (AL) and a capsulotomy is performed. At this stage, further tissue samples are taken for histology and microbiology examination. The femoral prosthesis is examined at the head-neck (Fig. 2) interface as well as femoral stem-bone interface (Fig. 3). Acetabular component is assessed at the implant-bone interface (Fig. 4). Acetabular liner assessment is carried out at the periphery, but no attempt is made to distract the hip or examine the central part of the acetabular liner (Fig. 5). Both femoral and acetabular components can be stressed with a blunt and rigid instrument such as a Trethowan bone lever to assess for loosening. Dynamic testing is carried out to rule out any macro- or micromotion at the implant-bone interface and impingement of soft tissues on implant. In a case of typical iliopsoas impingement, the anterior capsule in the vicinity of the iliopsoas tendon shows fraying (Fig. 6) and synovitis. Occasionally the iliopsoas can be seen impinging on the hip prosthesis. The impingement may be at the rim of the acetabular component (Fig. 7), femoral head, or a combination. The iliopsoas course is identified both arthroscopically and with the aid of an image intensifier. If the hip arthroplasty was undertaken using a posterior approach, then a clear visualization of zona orbicularis is possible; however, medial synovial fold is often difficult to view. A window is made in the anterior capsule with a radiofrequency probe and iliopsoas tendon is identified (Fig. 8). This is carried out either at the acetabular margin or further distal depending on the site of impingement and scarring. The iliopsoas tendon is identified and carefully dissected from the often-adherent capsule. Histology samples are routinely taken (Fig. 9) and assessed for aseptic lymphocyte-dominated vasculitis-associated lesion (ALVAL) [10]. If there is a large iliopsoas bursa or significant metal debris in cases of MoM hip arthroplasty, it is cleared away (Fig. 10). Once the iliopsoas tendon is isolated, the lengthening is undertaken by releasing the tendinous part of the iliopsoas only (Fig. 11). The muscle fibers are preserved, which avoids total transection of the iliopsoas tendon-muscle complex as well as safeguards against damage to the neurovascular structures. The iliopsoas tendon release is undertaken using radiofrequency probe. Depending on the site and angle required, a 90° RF probe (Fig. 8) or a hooked RF probe can be used. The fibers are released from deep to superficial under direct vision and the extent of lengthening is noted, which ranges from 2 to 3 cm (Fig. 12). Care is taken to avoid cutting the muscle fibers in the iliopsoas muscle-tendon complex (Fig. 13). This is followed by dynamic assessment, checking the extent of clearance achieved. The opportunity is taken to document any prosthetic overhang either due to oversizing the components or malposition. This is important for further surgical planning should the arthroscopic surgery fail to resolve the whole problem.