Fig. 1
Coronal MRI of a 45-year-old female with acute proximal hamstring avulsion (solid arrow) and 6 cm of distal retraction from the ischial tuberosity (dashed arrow) (Taken from Larson [10])
Operative Indications
Indications for repair of chronic proximal hamstring avulsions include two- or three-tendon complete avulsions from the ischial tuberosity or incomplete avulsion that fails conservative treatment with associated poor leg control, recurrent spasm and cramping, and sciatic nerve symptoms [10]. In the chronic setting, the hamstring muscles are retracted distally, scarred in place, and often cannot be mobilized sufficiently to obtain a primary repair. If this is the case, three options remain including tenodesis to the adjacent hamstring musculature, distal fractional lengthening and primary repair, and allograft reconstruction. Tenodesis is reported to result in unsatisfactory results [3]. Distal fractional lengthening produces better results but requires an additional incision and is technically demanding [6]. Reconstruction using Achilles tendon allograft has thus become the author’s preferred method as this allows for restoration of hamstring complex, crossing two joints, avoids the need for additional distal incisions and dissection without placing undue tension on the adjacent sciatic nerve.
Intraoperative Setup
The patient is positioned prone on the operating table. The use of a laminectomy frame eases positioning although it can be accomplished safely and conveniently with the use of large rolls, one under the chest and a second under the pelvis. Pillows or stacked blankets are placed under the patient’s tibiae and feet with the goal of approximately 20–30° of hip flexion and 50° of knee flexion. The operative leg should be prepped and draped free from the posterior pelvis to the foot. Keeping the foot uncovered will allow more accurate assessment of sciatic nerve function intraoperatively with the use of a nerve stimulator.
Surgical Technique
While acute ruptures can be performed through transverse incisions, for chronic ruptures, a longitudinal incision is preferred and allows for more predictable access to the retracted hamstring stump (Fig. 2). The degree of retraction is assessed by MRI and with resisted knee flexion in the holding area and marked prior to the procedure. An incision is made from the gluteal crease to the level of the retracted hamstring tendons. The length of the incision will vary depending on retraction of the hamstring tendons. Sharp dissection is carried through the skin, subcutaneous tissue, and to the level of the hamstring fascia. The gluteus maximus is not incised but retracted proximally in order to identify and expose the ischial tuberosity. The sciatic nerve is identified and lies deep and lateral to the hamstring tendons followed by a formal neurolysis (Fig. 3). Locating the nerve distally in an area of more normal anatomy and/or the use of a nerve stimulator to differentiate from surrounding scar tissue is recommended. The retracted hamstring tendon stump is then dissected free and mobilized. The ischial tuberosity is then identified and exposed to a bleeding bony bed (Fig. 4). It is important to recognize the anatomic origin of the proximal hamstring complex as it is fairly proximal on the ischial tuberosity.

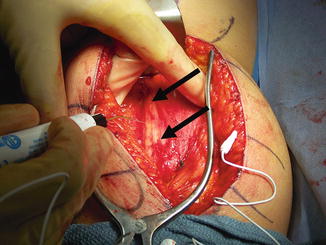
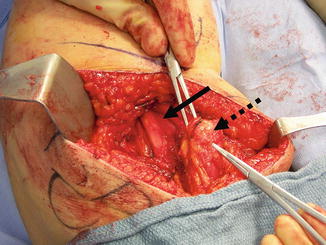

Fig. 2
The patient’s left leg has been draped for surgery. The planned longitudinal incision has been drawn down the posterior thigh from the center of the ischial tuberosity, starting at the gluteal crease (Taken from Larson [10])
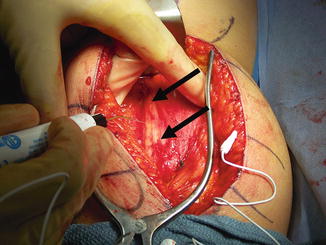
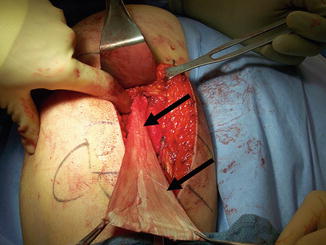
Fig. 3
After dissection is taken though the skin and subcutaneous tissue, a nerve stimulator is used in the sciatic nerve (identified by arrows) neurolysis (Taken from Larson [10])
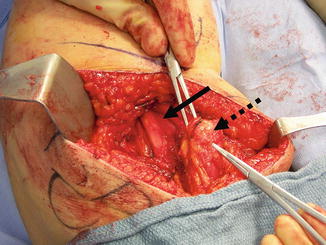
Fig. 4
The hamstring tendon (dashed arrow) is mobilized after the sciatic nerve identified (solid arrow) and neurolysis performed (Taken from Larson [10])
Next, the method of proximal fixation must be made. If the patient is a small female with an ischial tuberosity that is not of sufficient size to accommodate a bone plug or if the patient has a large gluteus maximus muscle that limits proximal exposure, two to three large suture anchors can be used for tendon reattachment. The anchors are placed in the anatomic footprint of the proximal hamstrings, lateral on the ischial tuberosity. The graft is then prepared and the Achilles bone block excised from the tendon (Fig. 5). One limb of each suture is placed in locking fashion through the graft. The second limb is used to secure the allograft to the ischial tuberosity.


Fig. 5
The Achilles allograft prepared with bone plug for fixation with interference screw (Taken from Larson [10])
If there is adequate bone and proximal exposure, an 8 × 20 mm bone plug is fashioned from the calcaneal allograft and fixed to the ischium with an interference screw. If this method is selected, a guidewire for an 8 mm reamer is drilled into the center of the hamstring footprint (Fig. 6). It is critical to verify that at least 20 mm of the wire is within the bone to ensure the entire bone plug and interference screw will seat and not be prominent. Ream over the guide pin to the appropriate depth, insert the bone plug, and secure it into the tuberosity with a 7 or 8 × 20 mm interference screw depending on bone density.
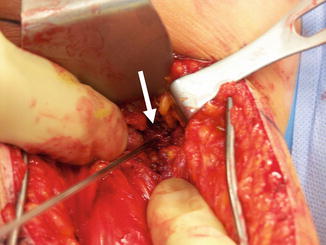
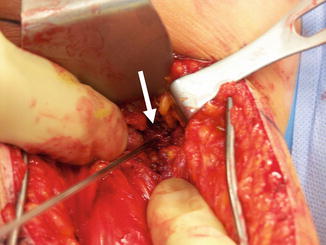
Fig. 6
Insertion of the guidewire into the prepared ischial tuberosity (white arrow) in preparation for reaming and graft insertion (Taken from Larson [10])
While ensuring the hips are flexed 20–30° and the knees at least 45°, the graft is pulled distally and the hamstrings proximally. Under tension, the two are provisionally secured together with heavy absorbable suture. The tension is then evaluated. The newly reattached hamstrings should be taut in 45° of knee flexion but allow for knee extension to within 10° of full extension. If too much or too little tension is noted, simply repeat the previous step until appropriate tension is achieved. Finally, secure the graft to the tendon in a locking fashion with nonabsorbable sutures (Fig. 7). Check the sciatic nerve to be sure there has been an adequate neurolysis and there is minimal tension on the nerve with knee motion. The wound is then irrigated, hemostasis obtained, and the wound is closed in standard fashion (Fig. 8a, b).