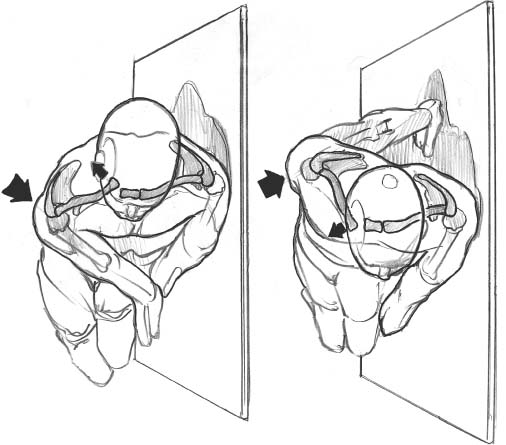
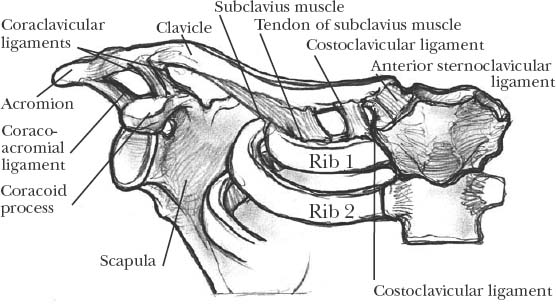
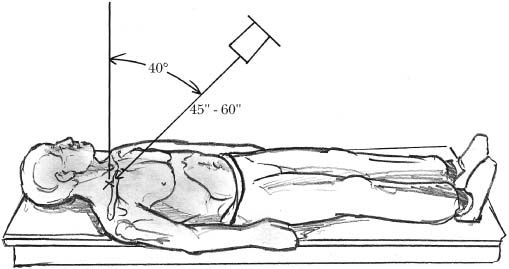
10 Sternoclavicular injuries are infrequent but often devastating.1–4 Because of its medial location and strong ligamentous supports, this joint, the only major connection between the upper extremity and the axial skeleton, is rarely injured.1–3,5,6 When injuries do occur, they can be difficult to diagnose because of the problems in imaging this joint. Delay in diagnosis can be disastrous in the event of a posterior or retrosternal injury. Diagnostic delay has been attributed to radiologic limitations as well as the paucity of sternoclavicular disorders and therefore the unfamiliarity that orthopedic surgeons may have with them.1,2,7 Retrosternal dislocations and physeal fractures can potentially be life threatening because of the close proximity of the sternoclavicular joint to the lungs, great vessels, esophagus, and trachea. Fortunately, the vast majority of sternoclavicular joint injuries are anterior from an indirect blow to the antero-lateral shoulder. Anterior sternoclavicular joint injuries, in contrast to posterior injuries, are associated with a more benign course. The anatomy of the sternoclavicular articulation is somewhat unusual. The sternoclavicular joint itself is the only true articulation between the axial and appendicular skeleton6 and accounts for the majority of scapulothoracic motion.8 It is a diarthroidal joint that has the least amount of bony stability of any joint of the body.1,5,6,9 The sternoclavicular joint is formed by the large, bulbous sternal end of the clavicle, the upper and lateral portion of the manubrium sterni, and the cartilage of the first rib (Figure 10-1).4,5,10–12 The articular surface of the medial clavicle is much larger than the opposite surface of the manubrium, which, according to Grant, makes for an “ill fit.” Less than 50% of the clavicle articulates with its sternal counterpart.5,9,11,13 Consequently, the ligamentous supports play the predominant role in stability of this articulation. The costoclavicular (also referred to as rhomboid) ligament is the strongest contributing ligament to the articulation and is thick, short, and flat.11 It runs obliquely from the costal tuberosity on the undersurface of the clavicle to the upper and medial portion of the first rib cartilage near the synchondrosis with the sternum. There are both anterior and posterior fasiculi of the costoclavicular ligament.4,14–16 The anterior fasiculus is directed upward and laterally from its origin on the first rib, and the posterior fasiculus has fibers that are directed upward and medially.5,6,11 Functionally these two bundles cross and confer considerable stability during rotation and elevation of the medial end of the clavicle.5,6,11,14,15 The interclavicular ligament runs along the top portion of the sternoclavicular joint and connects the two superomedial ends of the clavicle while also sending a portion to the top part of the manubrium. According to Gray, this ligament can vary considerably in size and form in different individuals.11 The anterosuperior and posterior sternoclavicular ligaments represent joint capsular thickenings and confer a large part of sternoclavicular stability as well. The articular capsule surrounds the articulation and varies in thickness and strength, with the strongest portion anterior followed by posterior, and thins superiorly and inferiorly.11 The attachment of the ligament onto the clavicle occurs largely in the epiphyseal region with some extension into the metaphysis.4–6,12 Bearn14 has shown experimentally the capsular ligament to be the primary restraint to superior translation of the medial clavicle that might occur from a downward blow to the superolateral aspect of the shoulder. The weaker anterior portion of the joint capsule allows more disruption than does the posterior portion, accounting for the much more common occurrence of anterior sternoclavicular dislocation as opposed to posterior or retrosternal.17 FIGURE 10-1. The anatomy of the sternoclavicular joint. The intra-articular disk ligament is a true fibrocartilagenous disk that is flat and circular and sits interposed between the medial clavicle and sternum.11 Superiorly it attaches to the posterior portion of the articular surface of the clavicle; inferiorly it attaches to the synchondrosis near the sternum. It is thickest along its circumference and thinnest at its center portion. The disk divides the articulation into two separate synovial compartments. Anteriorly and posteriorly the disk ligament interfaces with the anterior and posterior capsular ligaments, respectively.11 Its main function is to prevent medial displacement of the clavicle.4 Major structures exist behind the sternoclavicular joint that must be considered when surgery is being considered or when a patient presents with a retrosternal injury. Mediastinal and hilar structures include the innominate artery and vein, vagus and phrenic nerves, aortic arch, internal jugular vein, trachea, and esophagus. Rockwood and Wirth4 point out that there is a sleeve of muscles posterior to the sternoclavicular joint and medial clavicle (sternohyoid, sternothyroid, scalenes) that completely obscures the great structures from direct visualization. The relationship of the great structures to the sternoclavicular joint and the muscular sleeve must be considered in both surgical and nonsurgical evaluation of patients. The clavicle is the first long bone to ossify (occurs during the fifth intrauterine week), and its medial physis is the last to fuse in the body.4,16 The medial clavicular epiphysis appears at age 18 to 20 and does not fuse with the shaft of the remaining clavicle until age 23 to 25 and in some cases even later.4,5,9,18 This becomes clinically important in evaluating younger patients with sternoclavicular joint injuries, as an apparent dislocation may actually be a physeal fracture. Most commonly these are Salter I or II injuries that the meta-physeal portion of the clavicle displaces through a periosteal sleeve.3 The sternoclavicular ligaments, capsule, epiphysis, and joint all remain in their correct anatomical location.3,19–21 Medial clavicular dislocations are uncommon in the skeletally immature.1,7,17,19 Differentiating between sternoclavicular dislocation and physeal injury may be impossible. According to Rock-wood and Wirth,4,5 the majority of physeal injuries heal with expectant management. Closed reduction of all posterior physeal injuries should be attempted within 10 days of the injury. Remodeling will occur, and most deformity and displacement will be eliminated. If, however, there are symptoms of mediastinal injury, an open procedure should be carried out regardless of time since injury.4,5 Rockwood and Wirth point out that at the time of surgery for a physeal disruption, the epiphysis remains with the sternum, not with the clavicle. This must be appreciated to prevent inadvertent excision of the unossified medial end of the clavicle during open reduction.5,22 The sternoclavicular joint is an extremely important articulation, as scapulothoracic and sternoclavicular motion go hand in hand. Scapulothoracic motion is dependent on motion at the sternoclavicular joint.6,10,12 Therefore, fusion of this joint would greatly limit scapulothoracic motion.4,6,9,10,18 The long lever arm of the scapulothoracic articulation often dooms attempts at fusion and fixation.10 Motion occurs in nearly every direction: anterior, posterior, medial, lateral, and circumduction. Clavicular protraction and retraction occur between the sternum and the disk ligament. Clavicular elevation and depression occur between the clavicle and disk ligament.11,12 Relative contributions of each specific anatomical part are dependent on the position of the arm as well as the applied load.13,23 Motion at the sternoclavicular joint is reciprocal with motion at the acromioclavicular joint except in rotation.4,12 With full forward flexion the lateral clavicle elevates 35 degrees and rotates up to 45 degrees along its long axis. With extension and adduction the clavicle protracts and retracts 35 degrees.4 Clavicular rotation occurs in the same direction at the acromioclavicular and sternoclavicular joints.12 Motion at the sternoclavicular joint is complex and has yet to be completely elucidated with regard to differential loads and various shoulder positions. Sternoclavicular dislocations are extremely uncommon and account for only less than 1% of all joint dislocations.1,24 Cave, in 1958, published a series of 1603 injuries to the shoulder girdle and reported that only 3% were sternoclavicular dislocations.3,25 Of these, only one was a retrosternal dislocation. Nettles and Linscheid24 reported their experience with 60 sternoclavicular dislocations. From their series only three had retrosternal dislocations. Rockwood and Wirth9 reported a series of 185 traumatic sternoclavicular joint injuries. They had 135 anterior and 50 retrosternal dislocations. In the past 65 years 102 cases of sternoclavicular disruptions have been reported in the English literature.26 Thirty percent of these (31 cases) had complications relating to the retrosternal displacement of the medial clavicle from injury to the trachea, esophagus, and great vessels.26 Three of the patients in that series died as a result of mediastinal injury and ensuing complications. The diagnosis of sternoclavicular injury is frequently missed. Thomas et al8 described three missed cases of retrosternal dislocations, all of which had significant injuries to their shoulders and had plain films read as normal by junior and senior medical staff. Hence, a high index of suspicion must exist in the patient with shoulder trauma and medial clavicular pain despite the presence of normal-appearing routine plain x-rays. In general, a large force is necessary to disrupt the stern-oclavicular joint. Forces can be either direct or indirect (Figure 10-2). Indirect mechanisms are the most common.4 Patients will usually give a history of a motor vehicle accident or a fall onto the affected shoulder.17 A force directed at the medial third of the clavicle from the anterior position can produce a retrosternal dislocation.4,6,9 Direct blows cause only posterior, not anterior, dislocations.6 Because both ends of the clavicle move in reciprocal directions,6 indirect forces at the point of the shoulder can produce both presternal and retrosternal dislocations. Presternal dislocations are due to forces that retract and depress the clavicle. Retrosternal dislocations occur as a result of forces that protract the clavicle, either direct or indirect. Dislocations occur commonly as rollover events. If the shoulder is compressed and rolled forward, a retrosternal dislocation results. If the shoulder is compressed and rolled backward, however, a presternal dislocation results.4 A blow to the posterolateral corner of the shoulder can cause medial clavicular retraction, yielding a reciprocal retrosternal dislocation of the sternoclavicular joint. Conversely, a blow to the anterolateral shoulder (posteriorly directed force) can cause a medial clavicular protraction, effecting a pre-sternal sternoclavicular dislocation. As the anterior load is applied to the lateral clavicle, the anterior sternoclavicular ligament becomes taut. The posterior manubrium and clavicle contact, acting as a further fulcrum in tearing the ligament anteriorly and allowing subluxation or frank dislocation of the joint. Depending on the severity of the trauma, patients will generally present with their injured arm supported across their chest and complain of severe pain localized to the sternoclavicular area exacerbated by any movement of the extremity.4,5 They may give a history of a direct blow or fall to the clavicle or shoulder. If the joint is dislocated, the shoulder girdle appears shortened, and the head may be tilted and rotated due to sternocleido-mastoid muscular spasm.6 Pain can be elicited with palpation of the area as well as with compression of the shoulders toward the midline. If the medial clavicular head is dislocated anteriorly, it can be seen and palpated as a prominence on the chest wall. It may be fixed or mobile.5 FIGURE 10-2. The mechanism of injury can be direct or indirect. In contrast, a posterior dislocation may be more subtle and difficult to diagnose. There may be no apparent deformity at all, or there may be soft tissue swelling that masks the absence of the clavicular head in the sternal notch. Palpation of the joint may reveal a step-off posteriorly or a prominent manubrium at the sternal notch. Patients may present with respiratory difficulties, dysphagia, weaker or absent peripheral pulses, or numbness and tingling in the involved upper extremity. There may also be venous congestion in the neck and arm from compression on vascular elements in the chest. These potentially life-threatening injuries must be noticed early, and appropriate consulting services must be notified emergently (general surgery, cardiothoracic surgery, vascular surgery). Imaging of the sternoclavicular joint can present a significant challenge to the examining physician. Stern-oclavicular dislocations are frequently missed on routine plain x-rays of the shoulder and chest.4,5,6,8,27 The sternum is relatively hypodense and therefore difficult to see with the overlying vertebrae and ribs. A true lateral is extremely difficult to interpret because of the medial clavicular overlap with the sternum and first rib.27,28 Additionally, the obliquity of the joint itself makes plain orthogonal radiographs of little use. Several specialized plain x-ray views have been described. The value of early diagnosis, especially of a posterior dislocation, cannot be overemphasized. The risk of a major complication from a posterior dislocation remains until reduction has been effected.7,17,27 Therefore, rapid diagnosis with plain radiographs can be extremely valuable. Rockwood and Wirth described the “serendipity view,” or 40-degree cephalic tilt view4,9 (Figure 10-3). This view resembles a lordotic chest x-ray. The patient lies supine on the x-ray table, and a large cassette is placed behind the patient’s head. The cassette must be large enough to capture both medial clavicular halves for comparison of the injured to the uninjured side. The x-ray tube is angled at 40 degrees to the head and is centered on the manubrium. In adults, a tube-to-film difference of 60 inches is employed. In this projection, if the sternoclavicular joint is dislocated anteriorly, the clavicle will appear superior to the uninjured contralateral clavicle. Conversely, if the joint is posteriorly dislocated, the clavicle will appear inferior. This view should not be difficult to obtain by trained technologists and should not take any longer than a chest radiograph.27
Sternoclavicular Injuries
Anatomy
Applied Surgical Anatomy
Medial Clavicular Physis
Biomechanics
Incidence
Mechanism of Injury
Assessment
Clinical Presentation
Imaging
Sternoclavicular Injuries
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree