66 Failure of spinal arthrodesis or fusion leads to a condition called pseudarthrosis. Though the term literally means“false joint,” it is commonly used in clinical practice to refer to nonunion at greater than 1 year following the index surgery.2 Pseudarthrosis incidence rates following spinal arthrodesis reported in the literature range from 0% to 56%, varying with site, approach, fusion material, instrumentation, and year of the study.3,4 The true incidence, however, is likely underestimated by the literature, as many patients with pseudarthrosis remain asymptomatic. More importantly, the diagnosis of pseudarthrosis in the absence of symptoms is not necessarily an indication for surgical revision. Although many imaging techniques are available for evaluation of pseudarthrosis, none is perfect, and no universally agreed-upon imaging criterion exists. Open surgical exploration remains the “gold standard” for the diagnosis of pseudarthrosis. Heggeness and Esses5 classified patients with spinal pseudarthrosis according to the appearance of the fusion on imaging studies into four categories: atrophic, transverse, shingle, and complex (Table 66.1). Pain is the most common complaint associated with pseudarthrosis. Pain may be persistent from before the procedure, but most commonly pain is noted to recur after a period of temporary relief around the time of surgery. This temporary period of improvement (often referred to as a honeymoon period) is believed to be associated with the temporary stability associated with instrumentation, and pain can recur with implant loosening. Table 66.1 Heggeness and Esses Classification of Lumbar Pseudarthroses
Spinal Imaging for Pseudarthrosis
![]() Classification
Classification
![]() Workup
Workup
History
Morphologic category | Description |
Atrophic | Most severe case: Involves gross atrophy and resorption of the bone graft. |
Transverse | Most common: Substantial mass of viable remodeled bone, continuous with the fusion mass of adjacent levels, that possesses a horizontal or transverse discontinuity. |
Shingle | Substantial mass of matured bone graft is present, but a defect is present in the fusion mass, which passes obliquely through the sagittal plane. Creates the impression of an onion-skin construction of the fusion mass. |
Complex | Least common: Unique for the presence of more than one adjacent defect in the fusion mass. |
In working up a patient with suspected pseudarthrosis, it is important to screen for local or systemic signs of infection and new neurologic symptoms, as they can suggest alternative or concomitant pathology. However, asymptomatic pseudarthrosis has been reported in as many as 50% of patients, making it difficult to diagnose based solely on clinical information.6
Physical Examination
Physical exam is often nonspecific, but can occasionally identify gross motion, surgical site infection, loss of alignment, or new neurologic symptoms. Positive exam findings and/or persistent complaints of discomfort should warrant further investigations, including imaging studies. Symptoms and exam findings confirmed by imaging may encourage a more aggressive treatment approach.
Spinal Imaging
Plain films are routinely used to follow patients after a spinal fusion to evaluate fusion and instrumentation status. If fusion is occurring, progressive consolidation and bridging of trabecular bone will be observed at the margins following a brief period of resorption in the early stages of healing (Fig. 66.1). Conversely, the presence of a radiolucent line within the fusion mass has been considered diagnostic of nonunion.7–9 Other clues to suggest pseudarthrosis include progressive settling or deformity. Loosening may be suggested by radiolucency around implants (Fig. 66.2). Delayed failure of implants is suggestive of continued implant loading and pseudarthrosis (Fig. 66.3A,B). However, plain films have been shown to correlate with surgical exploration only 68–82% of the time, with a high rate of false-negative studies, making plain film insensitive in diagnosing pseudarthrosis.9–12
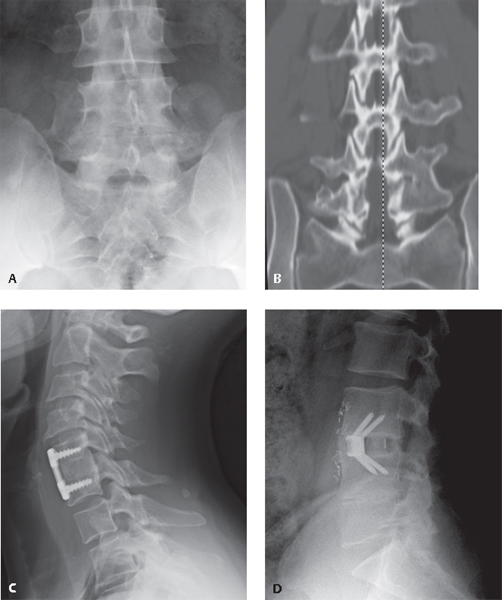
Fig. 66.1 Noninstrumented posterolateral lumbar fusion with new bone formation between adjacent transverse processes shown on (A) AP radiograph and (B) coronal CT. Instrumented (C) anterior cervical discectomy and fusion (ACDF) and (D) anterior lumbar interbody fusion (ALIF) demonstrating bridging bone (the sentinel sign).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






