Rupture of the Patellar Tendon
Mechanism of Injury
Direct
- Most commonly seen in patients less than 40 years of age during athletic activity
- Eccentric and forceful contraction of the quadriceps muscle resisted by the flexed knee (tripping while ascending stairs, landing after a rebound in basketball)
Indirect
- End-stage chronic tendon degeneration due to longstanding repetitive microtrauma
- Tendon weakened by systemic disorders such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), insulin-dependent diabetes mellitus (IDDM), chronic renal failure (CRF), or long-term systemic corticosteroid therapy or the local injection of corticosteroid into or around the tendon as a treatment for chronic patellar tendonitis
Patient Presentation and Symptoms
- History of trauma during athletic competition
- Sudden pain with an associated tearing or popping sensation
- Unable to continue with activity, and an assistive device required for bearing weight
Indications
- Complete ruptures
- Partial ruptures
- Chronic ruptures
Contraindication
Functional extensor mechanism (no extensor “lag”)
Physical Examination
- Tense hemarthrosis
- Unable to bear weight on the involved extremity
- Lack of active knee extension
- Unable to maintain the passively extended knee against gravity
- Passive knee flexion is diminished because of pain
- Palpable gap in tendon at the level of the rupture
- Proximal migration of the patella up to 5 cm
Diagnostic Tests
- Plain radiography, anteroposterior (AP) and lateral views. On the lateral view, patella alta is identified on the basis of the location of the inferior pole of the patella above Blumensaat’s line with the knee flexed 45 degrees. Insall-Salvati index greater than the con-tralateral knee. Bone avulsion from inferior pole of patella resembling Sinding-Larsen-Johansson disease.
- High-resolution ultrasonography: sagittal images obtained with linear-array transducers at center frequencies of 7 to 10 mHz
- Acute ruptures are identified by a confluent area of hypoechogenicity traversing the entire thickness of the tendon.
- In a chronic tear, thickening of the tendon at the site of rupture with disruption of the normal echo pattern
- Acute ruptures are identified by a confluent area of hypoechogenicity traversing the entire thickness of the tendon.
- Magnetic resonance imaging (MRI)
- Discontinuity of the tendon fibers, waviness of the ends of the tendon, and an increase in signal intensity on sagittal T2-weighted images.
- Hemorrhage and edema may also be seen to extend posteriorly to the infrapatellar fat pad.
- MRI is not recommended in the routine evaluation of most suspected patellar tendon ruptures.
- It is useful in the evaluation of a patient where the diagnosis is in question, in differentiating between a partial and complete tear, when associated intraarticular injury is suspected, or in the case of a neglected tear.
- Discontinuity of the tendon fibers, waviness of the ends of the tendon, and an increase in signal intensity on sagittal T2-weighted images.
Special Considerations
- If the rupture extends completely through the tendon and retinaculum, there will be total loss of active extension.
- Less commonly, if the rupture involves only the tendon and most of the fibers of the retinaculum remain intact, some active extension may still be possible, although an extension lag will often be evident.
- If there is any question, an ultrasound and/or MRI should be obtained to confirm the diagnosis.
- Partial tears of the patellar tendon are rare but do occur. Clinically active full extension of the knee, albeit painful and weak, can ensure that any disruption is incomplete.
- MRI is useful in delineating a partial from complete tear when the diagnosis is in question.
- A partial tear of the patellar tendon can be treated nonoperatively with immobilization for 3 to 6 weeks in full extension.
- In those patients with a history of systemic illness such as RA, SLE, CRF, and IDDM, or in those who have received long-term systemic corticosteroid therapy or repeated local injections of corticosteroid near the tendon as treatment for chronic patellar tendonitis or jumper’s knee, the tendon may be weaker due to long-standing compromise of intrinsic collagen structures. As the tissue may not be sufficient for primary repair alone, the surgeon must be prepared to augment the repair with Mersilene tape, cerclage wire, semitendinosus and/or gracilis free tendon graft, or in the extreme case, Achilles allograft.
Preoperative Planning and Timing of Surgery
- A lateral radiograph of the contralateral knee is obtained and patellar height is assessed so that intraoperative comparison can be made with the injured knee during the course of the reconstruction to ensure that the normal length of the patellar tendon is reestablished.
- An MRI may be necessary to identify associated intraarticular pathology, and if present, should be addressed accordingly.
- The most reliable indicator of prognosis is the interval between the injury and reconstruction. Surgical intervention should be performed as soon as possible (within 7 days). The timing is not for vascular considerations but to prevent any contractures that might make the procedure more difficult. Delayed repair (longer than 2 weeks) puts the patient at increased risk for loss of flexion, persistent quadriceps atrophy, and diminished quadriceps strength.
Special Instruments
- Intravenous antibiotics
- Standard instrument set
- Drill
- Pneumatic burr
- Rongeur
- Tendon stripper
- No. 5 nonabsorbable suture
- Keith needle (straight), Hughston suture passer, or Beath needle
- 5-mm Mersilene tape
- Cerclage wire No. 18 gauge
- Intraoperative fluoroscopy or x-ray
Anesthesia
Options are spinal anesthesia, epidural anesthesia with intravenous sedation as needed, or general anesthesia.
Patient and Equipment Positions
- Supine on a regular operating table
- If extremity tends to externally rotate, place a “bump” under the ipsilateral hip.
Surgical Procedure
Acute Ruptures of Patellar Tendon (Osteotendinous Junction)1,2
- Anterior, midline skin incision beginning 2 cm proximal to the superior pole of the patella and carried distally just medial to the medial edge of the tibial tubercle
- With careful dissection, the peritenon is opened longitudinally and preserved if possible.
- Irrigate the knee joint, evacuate hematoma, and debride back to healthy tendon.
- Create a horizontal trough along the inferior pole of the patella.
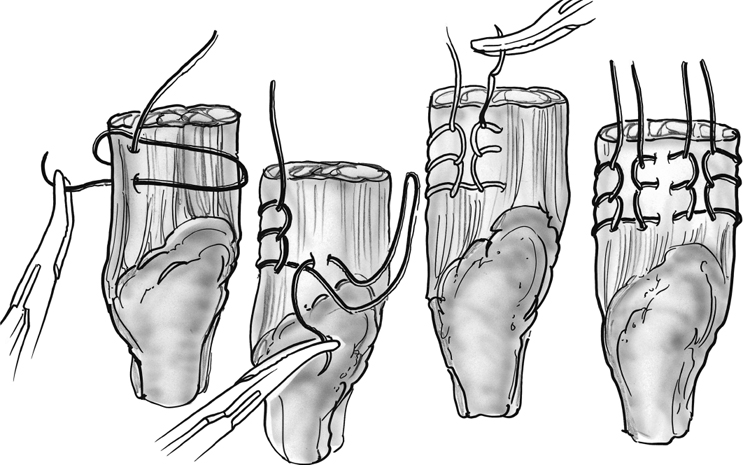
- Using No. 2 or No. 5 nonabsorbable suture, several parallel interlocking (Krackow) sutures are placed in the patellar tendon (Fig. 33–1).
- Four longitudinal drill holes are placed at the base of the trough, exiting at the superior pole of the patella.
- Pass the lateral suture through the lateral tunnel, the two central sutures through the central tunnel, and the medial suture through the medial tunnel (Fig. 33–2A).
- Traditionally, the suture is passed using either a (straight) Keith needle or a Hughston suture passer. Alternatively, the tunnels may be drilled using a Beath needle. The Beath needle has an eye so that the sutures can be passed using the same needle that was used to drill the tunnels.
- Tension is applied to the sutures, allowing the proximal stump to be seated within the bony trough. Use a smooth clamp to provisionally hold the sutures at the proximal pole of the patella, and move the knee through a range of motion to assess tension through the tendon along with tracking and rotation of the patella.
- If the patella is maltracking, perform a lateral release.
- Avoid overtightening the patellar tendon repair (this will create patella infera). Check intraoperative fluoroscopy or lateral knee radiograph at 45 degrees of flexion. The inferior pole of the patella should be superior to the roof of the intercondylar notch.
- Once patellar position is confirmed, the sutures are tied over an osteotendinous bridge at the proximal pole of the patella (Fig. 33–2B).
- Repair the medial and lateral retinacula with No. 0 absorbable suture.
- If the repair is tenuous, reinforce it with Mersilene tape or cerclage wire (Fig. 33–2C).
- Pass the reinforcing wire or tape through a transverse drill hole in the patella and a transverse drill hole in the tibial tubercle. It is prudent to place the transverse drill hole in the patella at a different level than the longitudinal tunnels to avoid compromise of the sutures. Ideally, create both tunnels prior to passing the sutures (requires early assessment of the patellar tendon). If a secure repair of the patellar tendon cannot be obtained with either of the repairs described above, augmentation with a semitendinosus/gracilis autograft is recommended (see below). 16. If the peritenon is present, it is closed over the graft with 2-0 absorbable sutures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








