CHAPTER 16 Rotator Interval Pathology
The term rotator interval was first attributed to Neer in 1970,1 when describing the capsular structures in the anterior shoulder found between the supraspinatus and subscapularis tendons. Although originally identified as a safe zone from which to access the glenohumeral joint, the role of the rotator interval in shoulder pathology and disease has become more defined as greater knowledge of shoulder kinematics and function has accumulated.
ANATOMY
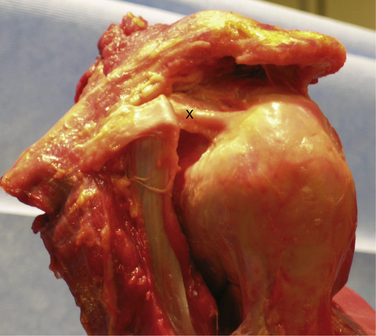
Knowledge of the complex anatomy of the rotator interval is essential to an understanding of the pathologic processes that may lead to shoulder pain and dysfunction. The rotator interval is triangular in shape and consists of the fibers that span the area between the supraspinatus and subscapularis tendons, medially from the coracoid to their insertions onto the greater and lesser tuberosities. The base of the triangle is made up of the base of the coracoid process and its apex is formed by the convergence of the lesser and greater tuberosities and bicipital groove laterally. The superior margin of the subscapularis tendon and inferior margin of the supraspinatus tendon make up the remaining respective sides of the interval. The interval contains the fibers of the coracohumeral ligament (CHL), superior glenohumeral ligament (SGHL), and biceps tendon, with their interdigitations with the supraspinatus, subscapularis, and glenohumeral joint capsule (Fig. 16-1). Distinct structures have been identified within the rotator interval, but histologic analysis has shown poorly organized collagen fibers, and a thinner, less distinct capsular structure in comparison to the well-defined inferior glenohumeral ligaments and capsule.2
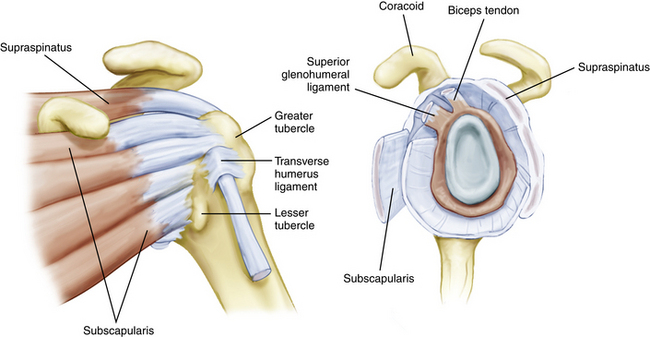
FIGURE 16-1 The rotator interval as viewed extra-articularly and intra-articularly.
(From Harryman DT 2nd, Sidles JA, Harris SL, Matsen FA 3rd. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53-66.)
The most recent detailed description of the anatomy of the interval was performed by Jost and colleagues.3 In their description, the rotator interval (RI) began as a two-layered structure medially and transitioned to a four-layered structure laterally near the insertions on the tuberosities. Medially, the two layers consisted of the coracohumeral ligament superficially and the superior glenohumeral ligament and glenohumeral joint capsule deeply. As the tissue fans out toward the humerus, two further layers form between the superficial CHL and SGHL. The more superficial layer consists of fibers of the supraspinatus and subscapularis, which interdigitate with those of the superficial CHL, and a deeper layer consisting of fibers of the deep coracohumeral ligament.
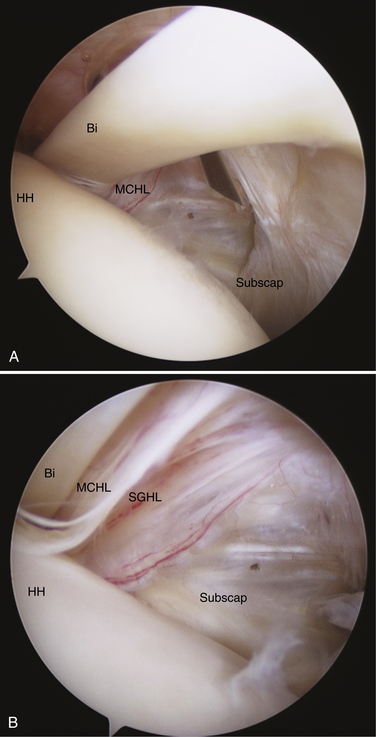
The CHL origin is about 2 cm wide and begins at the base of the lateral side of the coracoid process.4 The more superficial fibers cross over the interval and insert onto the medial portion of the greater tuberosity, blending with the fibers of the anterior supraspinatus and forming the lateral portion of the biceps sling (Fig. 16-2). The deeper fibers of the CHL blend with those of the SGHL and the upper subscapularis tendon to form the medial portion of the biceps sling.
The ligamentous structure of the CHL has been debated, and many authors5–7 have described it as an extra-articular fibrous structure that is a thickening or fold of the glenohumeral capsule. Others, such as Neer and associates,8 have recognized it as a distinct identifiable structure starting laterally at the coracoid base, but acknowledged that laterally there are slips that blend into the tendons of the rotator cuff. Microscopic examination has shown that it blends with the glenohumeral capsule with bundles and sheets of collagenous tissue without a discrete orientation, which is not consistent with a true ligamentous structure.9
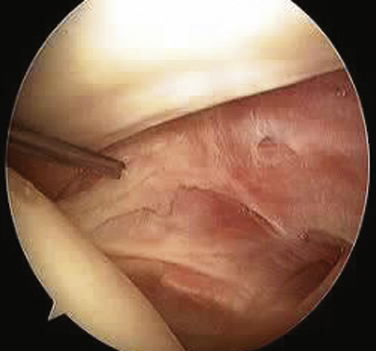
The SGHL originates from the glenoid labrum at roughly the 12 o’clock position.7,9 It crosses the floor of the rotator interval deep to the CHL, blending with the fibers of the glenohumeral capsule. Laterally, it joins the fibers of the deep CHL to form a reflection pulley for the biceps tendon. Similar to the CHL, the SGHL may be recognized as only a capsular thickening.2 Unlike the CHL, which can be seen extra-articularly, the deeper fibers of the SGHL are best seen within the joint as they cross across the RI and insert on the lesser tuberosity (Fig. 16-3).
BIOMECHANICS
Glenohumeral Joint Stability and Motion
Many studies have attempted to clarify the role of the rotator interval structures in passive motion and stability of the glenohumeral joint. Most studies agree that in concert, the RI works to provide resistance to posteroinferior translation of the humeral head and that imbrication or tightening of the RI will lead to restrictions in external rotation. However, disagreement exists about which of the structures may play the more predominant role. Ovesen and Nielsen10 originally identified the CHL as the more important inferior stabilizer, but did not specifically address the SGHL as separate from the CHL or anterior glenohumeral capsule. Boardman and coworkers11 have determined that the CHL can withstand higher tensile loads than the SGHL. Warner and colleagues12 were able to test the SGHL and CHL separately and determined that only the SGHL plays a significant role in preventing inferior translation. Cooper and associates9 have suggested that because the CHL does not consist of a truly ligamentous structure, it is unlikely to play a significant suspensory role as a soft tissue restraint in the shoulder.
Many cadaveric studies have noted that isolated release of the RI structures will affect both passive glenohumeral motion and humeral head translation. Ferrari and coworkers13 have confirmed through visual inspection that the anterior and proximal glenohumeral capsule became taut with external rotation in the adducted position. Similar findings have been noted by others in observational cadaveric studies.6,14
In an oft-cited paper, Harryman and colleagues7 performed sequential sectioning and successive repair of the RI capsule on cadaveric specimens to determine their effect on stability and motion. They found increases in flexion, extension, and external rotation with sectioning of the CHL and rotator interval capsular fibers. Furthermore, obligate translations of the humeral head were coupled with certain motions as a result of the sectioning. RI sectioning increased anterior translation in the abduction–external rotation position and inferior sulcus. However, the most striking finding was that a posteriorly directed force in slight abduction–external rotation resulted in posteroinferior dislocation in 50% of specimens. The authors concluded that the interval capsule acts as a checkrein to flexion and external rotation, and secondarily functions to provide additional posterior stability in the position of abduction–external rotation. In agreement with their findings, most cadaveric studies examining release of the RI and CHL have noted increases in passive external rotation of the shoulder. Neer and associates8 noted an increase of 32 degrees of passive external rotation with CHL sectioning. Tetro and coworkers15 more recently confirmed an increase of external rotation (in adduction) of 36 degrees and increased external rotation of 12 degrees in abduction after arthroscopic release of the rotator interval.
Biceps Stability
The structures of the RI play a key role in stabilization of the long head of the biceps tendon as it enters the bicipital groove. Werner and colleagues16 have examined the biceps sling anatomically and found the superior glenohumeral ligament and fasciculus obliquus as the primary stabilizers of the tendon at the entrance to the groove. Slatis and Aalto17 have determined through anatomic dissection that the medial coracohumeral ligament is the primary restraint to medial subluxation. Taken together, these and other studies have emphasized the role of the rotator interval capsular structures in biceps stability. Walch and associates18 have described hidden lesions of the anterosuperior cuff and interval capsule that can lead to medial subluxation and instability of the biceps tendon. In their group’s experience, subluxation of the biceps was always associated with subscapularis tendon tears and often with associated tears of the anterior supraspinatus. Gleason and coworkers19 performed an anatomic dissection of cadavers and were unable to find a distinct transverse humeral ligament; they found that the roof of the bicipital groove is made up of continuing fibers from the subscapularis tendon and coracohumeral ligament. Alternatively, Bennett20 has described two separate lateral divisions of the coracohumeral ligament, a lateral and medial division. The medial CHL and SGHL combined with the subscapularis tendon insertion form the medial stabilizers of the biceps sling, and it was noted that involvement of one structure, and not necessarily both, could result in biceps instability. In addition, the lateral CHL and anterior supraspinatus provide stabilization of the biceps tendon on the lateral side of the bicipital groove, and anterosuperior cuff tears involving these structures could also result in subluxation of the biceps tendon (Fig. 16-4).
PATHOPHYSIOLOGY
For the purposes of this chapter, pathology of the rotator interval will be divided into three groups. Taking from the original classification of rotator interval lesions by Nobuhara and Ikeda,21 two classifications of RI pathology will be reviewed: (1) contracture of the rotator interval, resulting in loss of glenohumeral motion; and (2) deficiency of the rotator interval, resulting in loss of normal glenohumeral stability. The third aspect is biceps tendon pathology as it relates to stability in the bicipital groove; this will also be discussed.
Rotator Interval Contracture and Adhesive Capsulitis
Many authors have cited contracture of the rotator interval as the primary involvement in adhesive capsulitis (frozen shoulder) and have focused on the RI (coracohumeral ligament and superior glenohumeral ligament) as the primary reason for loss of external rotation associated with the disorder.6,22,23 Bunker and coworkers22 have performed coracohumeral release for primary frozen shoulder and examined the specimens histologically for changes. They found an active fibroblast population, which was similar to the myofibroblast cell described in Dupuytren disease. Later work confirmed that Dupuytren disease is much more common in patients with idiopathic frozen shoulder, and that similar underlying pathologic processes may be involved.24 These results have been confirmed by others,25 suggesting that an unchecked fibroblast proliferation, combined with inflammation of the anterior interval capsule, leads to contracture of the RI and loss of active and passive motion. Although the underlying biochemical pathways leading to frozen shoulder have not been identified, clear risk factors have been identified, including female gender, diabetes mellitus, and hypothyroidism.
Rotator Interval Laxity and Instability
Glenohumeral instability is known to be a multifactorial process in which alterations in normal rotator cuff function, capsuloligamentous structures, and bony anatomy can lead to altered kinematics, with resultant instability. In their original report, Harryman and colleagues7 found that with sectioning of the RI capsule, posterior-inferior dislocation of the humeral head was possible in the abducted, externally rotated position. Although some have described rotator interval lesions in the settings of open surgery for instability, in the arthroscopic setting it becomes difficult to assess the tissue quality of anterior capsule. Usually, a layer of synovium and capsule will be present anteriorly, without the presence of a clear defect.21,26,27 We believe that with open reconstructive surgery for shoulder instability, friable tissue may be present in the rotator interval, which is easily disrupted and seen as a defect in the capsule. This is especially true with taking down the subscapularis when doing a capsular procedure.
The biomechanical effects of arthroscopic rotator interval closure have been examined in cadaveric models, but published data vary. Harryman and associates7 originally performed imbrication of the rotator interval capsule after cadaveric sectioning and found improved restraint to inferior and posterior translation. The procedure described was essentially a medial to lateral pants over vest imbrication of the coracohumeral ligament of approximately 1 cm. This was thought to be valuable in the setting of multidirectional instabilities, but the open procedure for rotator interval tightening described is very different from current arthroscopic procedures. Most descriptions of RI closure both arthroscopically and open used an inferior to superior closure, leaving limited applicability of this early data. The dramatic losses of external rotation (approximately 35 degrees) seen in their group are not noted in more recent arthroscopic cadaveric studies.
As noted, current arthroscopic techniques use an inferior to superior closure, which does not shorten the anterior capsule as described in the original paper by Harryman and coworkers.7 Using two superior-inferior sutures closing the anterior edge of the SGHL to the upper margin of the subscapularis or the MGHL, Yamamoto and colleagues28 have found decreased anterior translation in the abduction–external rotation (ER) position and decreased posterior translation in the adducted position. At the same time, passive ER and abduction were diminished. Plausinis and associates29
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree