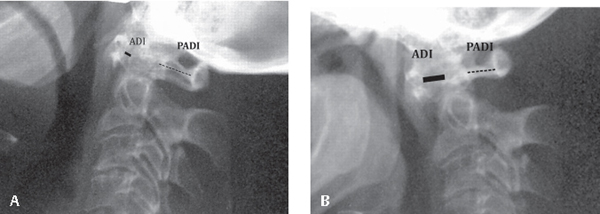
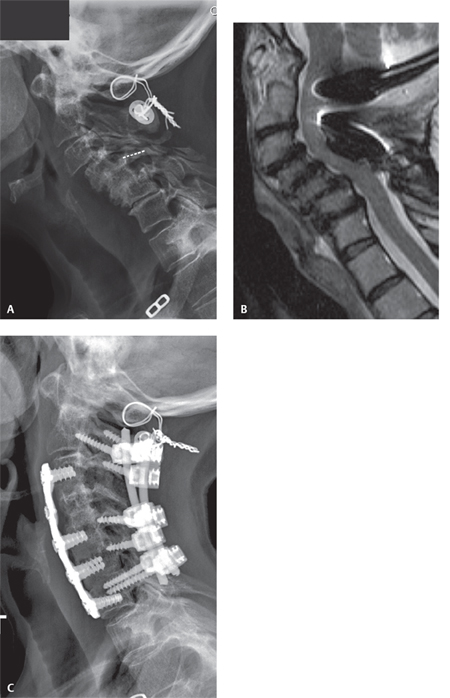
51 Rheumatoid arthritis (RA) is a chronic, systemic autoimmune disorder that affects many soft tissues and organs but primarily attacks synovial joints. It is the most common inflammatory disorder of the spine and has a predilection for the cervical spine.1 It is estimated that 1% of the population is afflicted by RA, with females having a threefold greater chance of having the disease. This disabling and painful condition is diagnosed primarily by symptoms, but also by blood tests and radiographic findings.2 The diagnosis carries with it a reduced life expectancy and a 50% risk of disability within 10 years of diagnosis.3 Despite its prevalence, the etiology of the disease is unknown but is likely multifactorial, with a strong genetic component. Medical treatment includes the early use of disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, and biologic agents, such as tumor necrosis factor (TNF) antagonists. Recent studies have suggested that these agents may preserve joint function and slow the progression of the disease.4 Cervical spine manifestations occur in 25–80% of individuals diagnosed with RA, with the severity of the cervical spine involvement mirroring the severity of peripheral joint involvement.5 The complex joints of the upper cervical spine appear to be uniquely susceptible to the ligamentous and bony damage of RA. Chronic synovial inflammation can lead to pain, deformity, instability, and neurologic deficits. Three common patterns of cervical spine instability have been described and include: atlanto-axial subluxation (AAS), atlanto-axial impaction (AAI), and subaxial subluxation (SAS). Atlanto-axial instability or AAS is the most common deformity of the rheumatoid spine, occurring in 20–84% of patients.6–8 Inflammation and subsequent pannus formation cause damage to the transverse, alar, and apical ligaments as well as to the odontoid itself. The majority of C1–C2 subluxations are anterior, with rates of lateral and posterior cases estimated at 20% and 7%, respectively. Severe C1–C2 instability may place the upper cervical spinal cord at risk for neurologic injury. Atlanto-axial impaction (AAI) is (also known as basilar invagination or cranial settling) and is the second most common cervical spine deformity in patients with RA. Persistent inflammation causes damage to the atlantooccipital joints and surrounding ligaments, allowing cranial migration of the odontoid. Pannus formation on the odontoid can lead to further impaction into the foramen magnum and brainstem compression.9 Atlanto-axial impaction is thought to occur later in the course of the disease and carry with it a poor prognosis.10 Subaxial subluxation (SAS) is the least common deformity of the rheumatoid cervical spine. Inflammation of the facet joints is thought to lead to destabilization and subsequent subluxation. Known as the “staircase phenomenon,” sub-axial disease is most common at the C2–C3 level and often progresses caudally. Although important in the differential diagnosis of any patient, SASs are especially important to rule out in the case of previous upper cervical spine fusion.11 The incidence of neck pain in RA has been reported to be between 40% and 80% with radiologic changes in 43–86% of patients.6 However, neurologic deficits have been reported in only 7–36% of patients.12,13 Approximately 10% of patients have been shown on postmortem exam to have died of unrecognized spinal cord or brainstem compression.14 Risk of neurologic deficit has been shown to be higher in males, patients with severe involvement of peripheral joints, and patients who use corticosteroids.15 Boden et al. reported on the radiographic and clinical progression of 73 patients followed for over 7 years. They found that 42 patients (58%) developed paralysis. All paralyzed patients treated nonoperatively died within 4 years, while 71% of patients treated operatively improved at least one neurologic class.12 Although radiographic changes are often used in the classification of cervical spine involvement of RA, a careful history and physical examination are needed to identify subtle neurologic findings. Patients commonly report pain at the occipitocervical junction, and compression of the C2 sensory fibers can cause migraine headaches, ear pain, mastoid pain, or facial pain. Spinal cord compression can also lead to myelopathic symptoms, including weakness, loss of dexterity, and gait distubance. AAI may also lead to vertebrobasilar insufficiency, with resulting tinnitus, vertigo, visual changes, and dysphagia.1 The Ranawat classification of rheumatoid cervical myelopathy, although limited in specificity, provides a means of grouping patients for planning treatment and evaluating outcomes. Class I patients are neurologically intact, Class II patients have hyperreflexia and subjective weakness, and Class III patients have long-tract signs and objective weakness. Class III is further divided into ambulatory (IIIa) and nonambulatory (IIIb). Initial evaluation of the cervical spine includes anteroposterior (AP), lateral, and dynamic flexion and extension views. These provide a baseline to follow for radiographic progression and should be performed every 2–3 years. Radiographs should also be obtained within one year of any required intubation and in any patient with new neurologic symptoms. AAS is most commonly defined by three radiographic measurements (see Fig. 51.1). The anterior atlanto–dens interval (ADI) is measured on a lateral radiograph from the posterior aspect of the anterior ring of C1 to the anterior border of the dens. An ADI less than 10 mm was the earliest measurement shown to be prognostic of neurologic injury and was used as a relative indication for surgical stabilization.15 More recently, attention has been focused on the posterior atlanto–dens interval (PADI), the distance between the posterior border of the dens and the anterior aspect of the C1 lamina. This distance has also been defined as the space available for the cord (SAC). Boden et al. have shown that a PADI less than 14 mm is much more sensitive in identifying patients at risk for neurologic injury than ADI measurements are. Dynamic instability has been defined as greater than 3.5 mm of motion on flexion/extension films and is also considered a relative indication for surgical stabilization (Fig. 51.1A,B). AAI has many radiographic definitions based upon the location of the odontoid in relation to the skull base. Common definitions include protrusion of the tip of the odontoid past the line formed between the basion and opisthion (McRae’s line) and protrusion more than 4.5 mm past the line between the hard palate and opisthion (McGregor’s line). Such measurements are inherently susceptible to inaccuracy in the case of odontoid erosion. Several indices have been developed specifically to overcome this weakness, including the Clark station, Ranawat measurement, and Redlund-Johnell values (see Fig. 51.2). A recent review showed that only by the combination of all three of these values was a sensitivity greater than 90% achieved.16 The increasing availability of computed tomography (CT) with two-dimensional reconstructions enables direct visualization of the occipitocervical junction, eliminating the difficulties associated with plain radiographs. Fig. 51.1 52-year-old woman with neck pain and intermittent numbness, tingling, and weakness in both arms. (A) Lateral extension and (B) flexion radiographs of the cervical spine. ADI (solid line) and PADI (dashed line) are demonstrated. With flexion, PADI decreases to 11 mm, suggesting significant loss of space in the spinal canal. SAS is commonly measured by the translation of one vertebral body upon another, with a significant listhesis defined as a slip greater than 20% or 4 mm.1 As with the other forms of rheumatoid cervical spine disease, a more critical radiographic measurement is the space available for the cord (SAC). Boden et al. demonstrated that a sagittal diameter of the spinal canal less than 13 mm more closely relates to neurologic deficits than other radiographic measurements do12 (Fig. 51.2A–C). Advances in the availability and quality of magnetic resonance imaging (MRI) have allowed for more thorough radiographic evaluations of the cervical spine in RA patients. MRI provides more detail regarding the presence of rheumatoid pannus, odontoid erosion, compression of the spinal cord, and signal change within the substance of the spinal cord. While controversial, increased signal within the cord on T2-weighted images has been associated with poor postoperative neurologic recovery.17 This has been suggested to be an indication for surgical management. With AAI, direct visualization of the spinal cord and brainstem can be made. The angle subtended by a line along the anterior aspect of the cervical spinal cord and the medulla is known as the cervicomedullary angle. It is normally between 135 and 175 degrees; an angle less than 135 degrees has been strongly correlated with neurologic findings.18 When considering surgical treatment of a patient with RA, it is important to consider the systemic effects of the disease and properly manage the patient’s medications. Both cardiovascular and pulmonary disease are more common in the rheumatoid population. A thorough evaluation of the patient’s cardiac and pulmonary status is required prior to surgical management. Patients often require multiple medications to control their RA, including anti-inflammatory medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids, methotrexate, hydroxychloroquine, sulfasalazine, and TNF antagonists. These medications can increase the rate of postoperative infections and other complications but also are important in preventing a rheumatoid flare in the perioperative period that can slow the rehabilitation process. Corticosteroid management remains controversial, with the need for perioperative dosing dependent upon the amount of surgical stress. Cervical spine surgery for RA likely requires a moderate dose of supplemental hydrocortisone (50–75 mg hydrocortisone with tapering over 1–2 days or 10–15 mg of prednisone).19 Current recommendations state that aspirin should be discontinued ~ 7–10 days prior to surgery, and the cyclooxygenase-2 (COX-2) inhibitors should be discontinued 5 half lives before surgical intervention, with a reported range between 9 hours and 1 week.9 Fig. 51.2 64-year-old woman with progressive loss of strength and numbness in the upper extremities as well as gait imbalance. (A) Lateral radiograph reveals multiple SASs, creating a “staircase” deformity of the cervical spine. Space available for the cord (SAC) is demonstrated (dashed line) and measured to be 9 mm. Prior C1–C2 stabilization for atlanto-axial instability is also seen. (B) Sagittal T2-weighted MRI confirms multilevel spinal cord compression consistent with clinical symptoms and signs. (C) Postoperative lateral radiograph after multilevel anterior decompression and fusion combined with posterior instrumentation and fusion.
Rheumatoid Arthritis of the Cervical Spine
![]() Classification
Classification
![]() Workup
Workup
Physical Examination
Radiographs
![]() Treatment
Treatment
Perioperative Care of the RA Patient
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






