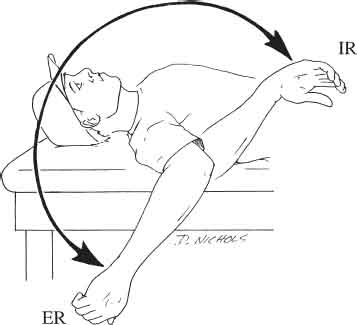
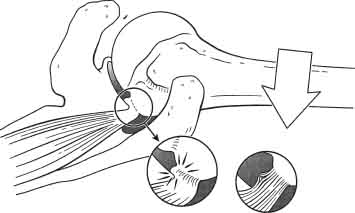
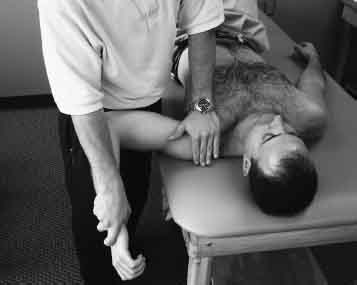
2 Michael M. Reinold, Leonard C. Macrina, Kevin E. Wilk, and James R. Andrews The overhead athlete, however, is unique and typically presents with a certain degree of acquired laxity from the inherent stresses observed during competition. Although necessary to perform at a competitive level, this acquired laxity may progress to excessive micro-instability and lead to pathologies such as rotator cuff and labral degeneration, fraying, or lesions. In this chapter, our purpose is to overview the classification and mechanism of acquired laxity in overhead athletes, to review common examination techniques used to determine the extent of pathology in these patients, and to discuss the specific rehabilitation principles and guidelines used to treat patients with pathological acquired micro-instability. Functional stability of the shoulder is achieved through the precise interaction of the static and dynamic stabilizing systems of the glenohumeral joint. Static stability is accomplished via the joint geometry, capsule, glenohumeral ligaments, and labrum. Because of the required amount of motion of the shoulder, particularly in the overhead athlete, static stability is often compromised, demanding a greater amount of dynamic stability to remain asymptomatic. Dynamic stability is achieved through the precise neuromuscular interaction of the force couples of the rotator cuff and the shoulder musculature.34,36 The need for excessive motion in the shoulder of overhead athletes requires the dynamic stabilizers to perform efficiently, particularly near end range of motion (ROM) when static stability is most compromised. Most overhead athletes exhibit significant laxity of the glenohumeral joint. This allows them to accomplish the necessary motions required to perform their sport. One significant difference between overhead athletes and nonoverhead athletes is shoulder ROM. The typical overhead athlete exhibits excessive external rotation (ER) and decreased internal rotation (IR) at 90 degrees abduction in the throwing shoulder.4,5,13,35 Brown et al5 reported that the mean ROM in 41 professional baseball pitchers was 141 degrees ± 15 degrees of shoulder ER at 90 degrees abduction and 83 degrees ± 14 degrees of IR. External rotation was 9 degrees greater in the throwing shoulder than in the nonthrowing shoulder, whereas IR was 15 degrees less than in the nonthrowing shoulder. Furthermore, ER of the throwing shoulder was 9 degrees greater in pitchers than in positional players. Similarly, Bigliani et al4 evaluated the ROM characteristics in 148 professional baseball players. The authors reported a mean of 118 degrees ER at 90 degrees abduction (range 95 to 145 degrees) in the throwing shoulder of pitchers and a mean of 108 degrees ER in positional players. A statistically significant increase in ER and decrease in IR was observed between the dominant and nondominant shoulder. Wilk et al36 reported the shoulder ROM characteristics in 372 professional baseball players. The authors reported a mean of 129 degrees ± 10 degrees of ER and 61 degrees ± 9 degrees of IRin the throwing shoulder at 90 degrees abduction. The authors noted that ER was 7 degrees greater and IR was 7 degrees less in the dominant arm when compared with the nondominant arm. Wilk et al36 introduced the concept of “total motion,” and defined it as the sum of ER and IR at 90 degrees abduction (Fig. 2–1). The authors noted that total motion is equal bilaterally in most throwers, usually within 7 degrees. These findings were similar to those reported by Ellenbecker et al9 in a group of tennis players. There are several theories explaining why the overhead athlete presents with these unique ROM characteristics. The repetitive microtraumatic stresses placed on the athlete’s shoulder joint complex during the throwing motion challenges the physiologic limits of the surrounding tissues. During the overhead throwing motion, the athlete places excessive stresses at the end ROM while generating tremendous angular velocities. Fleisig et al10 have reported the angular velocity of the arm during the overhead throw to reach 7265 deg/s, which is the fastest human movement. Furthermore, these forces are generated when the shoulder joint is at end range ER, often at 145 to 165 degrees of ER. This results in high forces generated and dissipated at the joint and the supporting structures (i.e., capsule and/or musculature).39 Fleisig et al10 reported anterior forces up to 1½ times body weight during ER (late cocking) and up to one and one-half times body weight distracting the joint during the follow-through phase. Consequently, the overhead athlete often presents with acquired anterior laxity due to the stresses placed on the joint throughout the throwing motion. Thus, the shoulder complex greatly relies on the dynamic stabilizers because of the compromised static stability often present. Figure 2–1 Total motion concept in the overhead athlete. (From Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med 2002;30:137 Figure 1. Reprinted with permission.) Previous authors have hypothesized that the loss of IR ROM can be attributed to posterior capsular contraction.6 However, this has been disputed by evidence of osseous retroversion of the humerus8,19,21 as well as excessive posterior laxity even in patients with marked loss of IR. Furthermore, Reinold et al24 recently noted that ROM is affected by overhead throwing. The authors evaluated shoulder ROM in 31 professional baseball pitchers before and immediately after baseball pitching. External rotation before throwing (133 degrees ± 11 degrees) did not significantly change after throwing (131 degrees ± 10 degrees). However, there was a statistically significant decrease in IR ROM after pitching (73 degrees ± 16 degrees before, 65 degrees ± 11 degrees after) and a subsequent decrease of 9 degrees of total motion. The authors hypothesized that this decrease in IR ROM was due to the large eccentric forces observed in the external rotators during the follow-through phase of throwing. Figure 2–2 Internal impingement leading to degeneration of the under surface of the rotator cuff. (From Walch G, Boileau P, Noel E, et al. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg 1992;1:243, Figure 5A. Reprinted with permission.) Thus, it appears that the ROM characteristics of the overhead athlete are due to a combination of factors, including acquired laxity of the anterior capsule, soft tissue adaptations of the posterior rotator cuff, and osseous adaptations of the humerus. Because of the delicate balance between acquired laxity and pathological micro-instability, the overhead athlete is continuously challenged to perform efficiently and remain asymptomatic. When the overhead athlete develops excessive laxity in the shoulder, it is most often a pathological micro-instability rather than gross macro-instability. The excessive amounts of translation observed in the athlete with acquired laxity may lead to several pathological conditions such as SLAP (superior labrum anteroposterior) lesions2 and impingement of the undersurface of the infraspinatus on the posterosuperior labrum.28 This is referred to as internal impingement and may lead to degeneration of the undersurface of the rotator cuff and labrum (Fig. 2–2). The phenomenon of internal impingement is one of the most common diagnoses observed in the overhead athlete. A thorough evaluation of the shoulder, including clearing examinations of the proximal and distal segments, is required to appreciate the nature and extent of the pathology. Examination techniques are performed to assess active and passive ROM, laxity, and muscle strength. The examiner may also perform several special tests to assess the integrity of the rotator cuff, labrum, and capsule. Although necessary to perform a complete and thorough evaluation, this is beyond our scope here; other authors review these tests and techniques in later chapters. We will briefly review a few tests that we feel are specific to the patient with micro-instability. The focus of the examination of these patients is the ROM characteristics and the capsular tissue laxity to determine the extent of instability. As discussed previously, total motion should be equal bilaterally. Total motion is routinely assessed clinically by simply adding ER and IR ROM using standard goniometric measurements. Athletes with symptomatic complaints of micro-instability will often present with a decrease in total motion when compared bilaterally. This overall loss of total motion is often attributed to loss of IR rather than ER. Theoretically, we believe that the loss of IR in the symptomatic athlete can be attributed to pathology of the posterior rotator cuff (rather than posterior capsule), resulting in fibrosis and loss of IR motion. Several tests may be performed to assess laxity of the capsular tissue. We commonly perform the sulcus sign, anterior and posterior drawers, and the anterior fulcrum tests. A simple technique used to determine generalized laxity of the glenohumeral joint is the sulcus maneuver.17,26 The sulcus sign is designed to assess inferior laxity and may be performed at various degrees of abduction. We routinely perform the test in the seated position at 0 degrees of abduction, which assesses the coracohumeral ligament and superior glenohumeral ligament.29 The test is performed by providing long-axis distraction of the humerus while grasping the bicondylar axis of the humerus and palpating the lateral subacromial space (Fig. 2–3). Normal motion varies between 5 and 15 mm depending on the patient population being assessed.12,14 We feel that a positive sulcus sign is present when there is greater than 10 mm of inferior humeral translation. This represents a degree of congenital laxity that may be present; we use it to determine the progress rate of our rehabilitation program. Individuals with significant congenital laxity (as indicated by a positive sulcus sign) may be progressed more slowly with specific emphasis on enhancing dynamic stability. The examiner performs specific techniques to assess anterior3 and posterior laxity.11 The anterior and posterior drawer tests are performed with the patient supine. The examiner grasps the arm at the bicondylar axis of the distal humerus. The patient’s arm is held in the scapular plane with neutral rotation. The proximal hand grasps the humeral head, which is gently compressed, then translated anteriorly or posteriorly. The tests can be performed at various degrees of shoulder abduction to assess the integrity of specific capsular ligaments (Fig. 2–4). Figure 2–3 Sulcus maneuver to assess inferior glenohumeral laxity. Another test commonly performed for overhead athletes with micro-instability is the anterior fulcrum test. This test is performed with the patient positioned supine at the edge of the examination table and the arm abducted to 90 degrees. The arm is placed in maximal ER. In this position, the anterior band of the inferior glenohumeral ligament complex wraps around the anteroinferior aspect of the humeral head and acts as a hammock to prevent anterior humeral head displacement.18 The examiner places the proximal hand on the posterior aspect of the glenohumeral joint to act as a fulcrum, while the other hand grasps the bicondylar axis of the elbow. The test is performed by simultaneously providing an anterior translation force as the humerus is brought into extension, acting as a fulcrum (Fig. 2–5). The examiner should feel minimal displacement and a firm end feel in the normal shoulder. In the patient with anterior micro-instability, there will be excessive anterior displacement and a softer end feel. Figure 2–4 Anterior drawer test As discussed previously, overhead athletes with micro-instability often have internal impingement. Meister et al15 originally described the internal impingement sign in which the patient is supine with the humerus at 90 degrees of abduction. The examiner passively rotates the shoulder into maximal ER until the patient experiences symptoms. Rather than feeling symptoms in the anterior aspect of the shoulder, which is common in patients with anterior macro-instability, the patient with internal impingement will have symptoms located specifically over the posterosu-perior aspect of the shoulder. A relocation maneuver is then performed while the patient is in maximal ER. The examiner provides a posterior force to relocate the humeral head within the glenoid and effectively alleviate symptoms, signifying that the symptoms were related to anterior translation (Fig. 2–6). Figure 2–5 Anterior fulcrum test. Figure 2–6 Relocation maneuver performed during the internal impingement sign. The rehabilitation process for overhead athletes with micro-instability must restore ROM, muscular strength, and endurance as well as gradually restore proprioception, dynamic stability, and neuromuscular control. As the athlete advances, sport-specific drills are emphasized to prepare for a gradual return to competition through an interval sport program. Neuromuscular control drills are performed throughout; they are advanced as the athlete progresses to provide continuous challenges to the dynamic stabilizers and neuromuscular system. In the following section, we provide an overview of a functional rehabilitation progression for overhead athletes with micro-instability, while incorporating the previously discussed principles and guidelines. The program is divided into four separate phases with specific goals and criteria to advance to the next phase. The use of a criteria-based rehabilitation program allows for the individualization of each patient and his or her specific pathology. It is imperative to modify each program based on the extent of each patient’s pathology. Alterations in exercise activities, positioning, and rate of progression are based on the type of injury, healing constraints, and the tissues that are being stressed during rehabilitation. The acute phase of rehabilitation begins either immediately following the injury or when symptoms arise. The duration of the acute phase is dependent on the healing constraints of the involved pathological tissues and the degree of the injury. The initial goals of the acute phase are to diminish pain and inflammation, normalize motion and muscular balance, and restore baseline proprioception and kinesthetic awareness. One of the primary goals during the acute phase is to normalize total motion bilaterally. This often requires the addition of ROM and flexibility exercises for IR and ER in a restricted ROM based on the theory that motion assists in the enhancement and organization of collagen tissue, the stimulation of joint mechanoreceptors, and possibly the neuromodulation of pain. The rehabilitation program should allow for progressive applied loads, beginning with gentle passive ROM. Active-assisted range of motion (AAROM) exercises are performed by the patient, which include a cane or L-Bar (Breg Corp., Vista, CA) for flexion, ER, and IR. As the patient advances, flexion progresses as tolerated and shoulder rotation ROM is progressed from 0 degrees of abduction to 30, 45, and 90 degrees of abduction. In addition, pendulum, rope, and pulley exercises may be used as needed to facilitate additional motion. We believe that one of the underlying causes of symptomatic internal impingement is excessive anterior shoulder laxity. One of the primary goals of the rehabilitation program is to enhance the athlete’s dynamic stabilization abilities, thus, controlling anterior humeral head translation. In addition, another essential goal is to restore flexibility to the posterior rotator cuff muscles of the glenohumeral joint. We strongly suggest caution against aggressive stretching of the anterior and inferior glenohumeral structures. This may result in increased anterior humeral translation. As previously mentioned, the soft tissue of the posterior shoulder is subjected to extreme repetitive, eccentric contractions during the throwing motion. This may result in soft tissue adaptations and loss of IR ROM.24 Common stretches performed include horizontal adduction stretching across the body with slight IR stretching at 90 degrees of shoulder abduction. The cross-body horizontal adduction stretch may be performed in a straight plane adduction motion as well as being integrated with a component of IR at the shoulder (Fig. 2–7). Strengthening begins with submaximal, pain-free isometrics for shoulder flexion, extension, abduction, ER, IR, and elbow flexion. Isometrics are used to hinder muscular atrophy and restore voluntary muscular control while avoiding detrimental shoulder forces. Isometrics should be performed at multiple angles throughout the available ROM, with particular emphasis on contraction at the end of the currently available ROM.
Rehabilitation of Micro-Instability
Common Examination Techniques
Acute Phase
Intermediate Phase
Advanced Phase
Return to Activity Phase
 Presentation and Mechanism of Acquired Laxity
Presentation and Mechanism of Acquired Laxity
Common Examination Techniques



 Rehabilitation Program for Overhead Athletes with Micro-Instability
Rehabilitation Program for Overhead Athletes with Micro-Instability
Acute Phase

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


