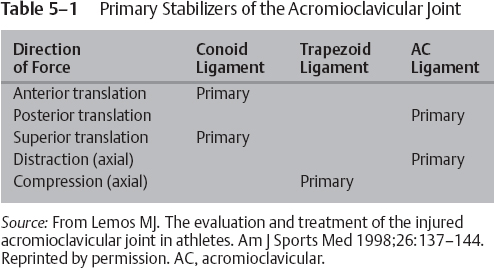
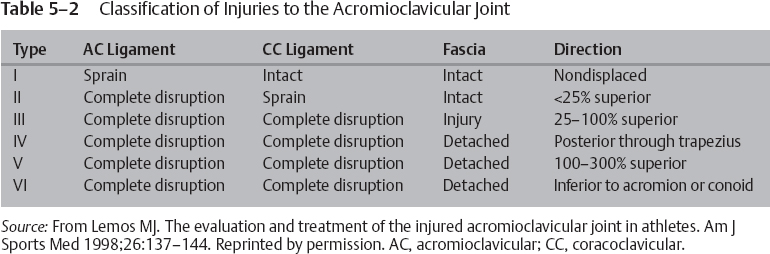
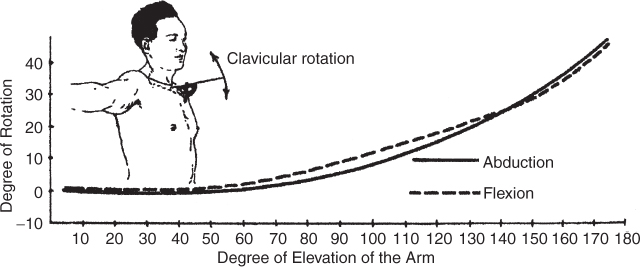
5 Timothy F. Tyler and Michael J. Mullaney The AC joint is a diarthrodial joint that joins the clavicle to the upper extremity via the scapula; it is a plane synovial joint with 3 degrees of freedom. The clavicle has ~50 degrees of rotation about its longitudinal axis, most of which is contributed by the mobile sternoclavicular (SC) joint.1 The inclination of the joint can vary from vertical to 50 degrees of medial inclination with the clavicle overriding the acromion.1 Although the clavicle rotates upward to 50 degrees during full overhead elevation (Fig. 5–1), only 5 to 8 degrees of the motion is detected at the AC joint.2 This difference is due to synchronous scapuloclavicular motion: As the clavicle rotates upward, the scapula rotates downward and the AC joint motion is minimized.3 Interposed in the joint is a fibrocartilaginous disk that aids in distributing the forces from the upper extremity to the axial skeleton. Studies have shown that this disk has variable morphology in size, shape, and existence.4 The ligamentous complex and support of the AC joint stability is composed of intracapsular and extracapsular ligaments. The AC joint capsule is reinforced with an encompassing ligamentous complex (Fig. 5–2). Ligaments surround this joint on the anterior, posterior, superior, and inferior side. This complex acts as the primary restraint to posterior translation and axial distraction.5 Fukuda et al5 determined that during small displacements, the AC ligament complex is the primary restraint to posterior and superior displacements. As the displacement increases, however, the conoid ligament of the CC ligamentous complex becomes the primary stabilizer with superior clavicle translation, and the AC joint ligament complex remains the primary stabilizer to posterior translation (Table 5–1). The CC ligament consists of the lateral trapezoid ligament and the more-medial conoid ligament (Fig. 5–2). The fibers of this ligament travel from the inferior aspect of the clavicle to the base of the coracoid process and posteriorly to the pectoralis minor tendon attachment.2 These two ligaments function differently with respect to the direction of the loads applied. The conoid ligament functions as a restraint to anterior superior loading, whereas the trapezoid ligament functions as a restraint to posterior loading.6 The CC ligament, though anatomically related to the AC joint and implicated in grade I and II AC joint separations, is the least important ligament to stability.2 It primarily prevents anterosuperior translation of the humeral head when a rotator cuff pathology is present.2 Figure 5–1 The clavicle rotates to allow the arm to elevate overhead. (From Rockwood Jr, CA, Matsen F III. The Shoulder. Philadelphia, PA: WB Saunders; 1990: 213, Figure 6–7. Reprinted by permission. Figure originally from Inman VT, Saunders M, and Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg 26, 1–30, 1944) Figure 5–2 Acromioclavicular (AC) joint stability is maintained by the AC ligament, coracoacromial ligament, and the two coracoclavicular ligaments. (From Agur AMR. Grant’s Atlas of Anatomy. 9th ed. Baltimore, MD: Williams & Wilkins; 1991: 392, Figure 6.46. Reprinted by permission.) As discussed, each of the ligaments associated with the AC joint are responsible for maintaining a level of stability that promotes shoulder function. Each of the ligaments is responsible for maintaining joint stability in a specific plane of motion. AC joint separations have been divided into six types (Fig. 5–3); each separation type typically correlates well with the constellation of the involved structures and the severity of the injury.7–9 The continuum of injury starts with the AC ligaments and capsular complex, progresses to involve the CC ligaments, and continues with injury to the deltoid and trapezius muscles. These patterns of injury generally result in predictable positions of the clavicle.1 Figure 5–3 Acromioclavicular injury types. Descriptions of each injury are given in Table 5–3. (From Rockwood Jr, CA, Matsen F III. The Shoulder. Philadelphia, PA: WB Saunders; 1990:423, Figure 12–13. Reprinted by permission.) Tossy et al7 and Allman8 initially described the classification of AC injuries in the 1960s. This original classification system included types I, II, and III; however, in 1984 Rockwood1 modified the classification system to include types IV, V, and VI (Table 5–2). AC joint injuries are approximately five times more common in men than in women, with type I and II injuries occurring twice as often as the more severe separations.10 Grade III separations account for ~15% of all shoulder sprains in male hockey players.
Rehabilitation of Acromioclavicular Joint Injuries
Treatment of Type I and II Injuries
Treatment of Type III Injuries
 Acromioclavicular Joint Anatomy and Biomechanics
Acromioclavicular Joint Anatomy and Biomechanics
 Classification of Acromioclavicular Joint Injuries
Classification of Acromioclavicular Joint Injuries
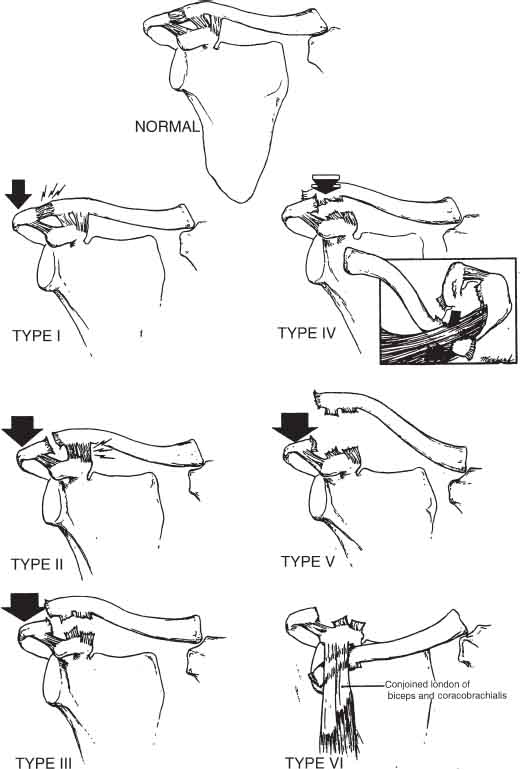
| Type I | A sprain to the AC ligament with no affect on the CC ligament or deltotrapezial fascia constitutes a type I injury. A type I injury has no displacement of the AC joint. |
| Type II | A complete disruption of the AC joint ligament complex and a sprain of the CC ligament with no effect on the deltotrapezial fascia constitute a type II injury. This injury will present visually with a <25% superior migration of the distal clavicle. |
| Type III | A complete disruption of the AC joint ligament complex, a complete disruption of the CC ligaments, and damage to the deltotrapezial fascia constitute a type III injury. This injury will present visually with a 25 to 100% superior migration of the distal clavicle. |
| Type IV | A complete disruption of both the AC and CC ligament complexes constitutes a type IV injury. The type IV injury will also present with a detached deltotrapezial fascia and a posteriorly migrated distal clavicle that penetrates through the trapezius. |
| Type V | A complete disruption of both the AC and CC ligament complexes as well as a detached deltotrapezial fascia and an exaggerated superior dislocation of the distal clavicle between 100 to 300% constitute a type IV injury. |
| Type VI | A complete disruption of the AC and CC ligament complexes as well as a detached deltotrapezial fascia constitute a type VI injury. The distal clavicle displaces inferiorly into the subacromial or subcoracoid position. |
 Examination and Presentation of Acromioclavicular Joint Injuries
Examination and Presentation of Acromioclavicular Joint Injuries
Pain associated with an AC injury may be difficult to localize because of the complex sensory innervations of the joint.2 The most important information during the examination process is gleaned by a thorough and extensive history. This information enables us to determine if the pain is a result of a separation or an ongoing degenerative process. Once it is determined that the pain is a result of an acute separation, further examination should address the level of pain, its location, and positions of relief. Each patient should also undergo a radiographic examination. The following are the general presentations of each separation type (Table 5–4):
Type I With only a sprain of the AC joint ligaments, no joint deformity is apparent during physical or radiographic examination. Minimal tenderness and swelling may be present over the AC joint; however, the injury is inherently stable because the AC and CC ligaments are structurally intact.1 The pain is generally self-limiting; however, patients will often report discomfort with full-arm abduction and flexion.
Type II In type II injuries, the AC ligament complex is completely torn; therefore, vertical stability is maintained but sagittal stability is compromised.1,11,12 On physical examination, like patients with type I injuries, patients with type II injuries present with pain as the primary symptom. Patients may present with a mild superior migration of the distal clavicle, as compared with the acromion. This migration may be better appreciated by running a finger along the acromion medially to the AC joint.2 Radiographic examination may also reveal this superior migration of the distal clavicle; however, the separation will be less than 100%. Patients may also present with minimal to moderate strength and ROM deficiencies. These deficiencies are typically secondary to the pain and not an alteration in the biomechanics of the AC joint.13
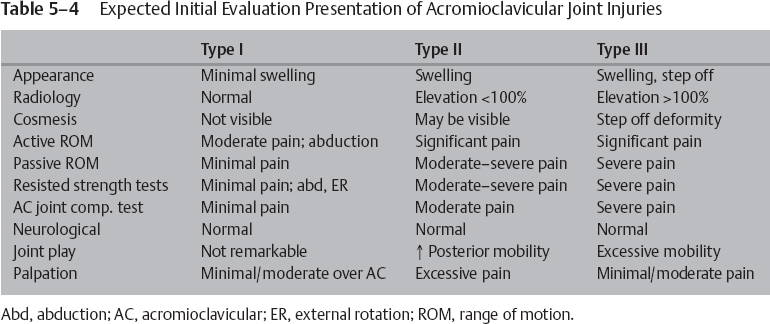
Type III In type III injuries, because the AC and CC ligaments are torn and the deltotrapezial fascia is detached, patients typically present with pain and an easily identifiable deformity called a step-off deformity (Fig. 5–4). Patients will typically present holding the arm in the adducted position to counteract the pain produced by the weight of the arm.2 Upon radiographic evaluation, the clavicle appears elevated; however, further evaluation will show that the elevation is actually the inferior displacement of the acromion. The loss of the conoid and trapezoid ligaments will compromise the horizontal and vertical stability of the clavicle. Upon palpation, increased tenderness will be noted over the AC and CC joints, as well as excessive pain with any active arm movement.
Type IV In type IV injuries, a similar clinical presentation as the type III injury, is commonplace. The difference in presentation includes the level of pain (greater in type IV injuries) and the displacement of the clavicle. In type IV injuries, the distal clavicle may be displaced into the trapezius muscle. This displacement into the muscle often causes the excessive pain that patients experience. The clavicular displacement is noted upon clinical presentation by a bump in the posterior skin of the shoulder. Radiographically, this can be confirmed by an axillary x-ray. It is also important to note the SC joint for an anteriorly dislocated clavicle. An anteriorly dislocated clavicle at the SC joint would reduce stress on the clavicle.2
Type V The type V injury is similar to a type III injury but more severe. Clinical presentation will include a severe shoulder droop, marked pain, and a CC distance increase up to three times.2 However, the biggest difference from the type V and type III injury is the involvement of the deltoid and trapezial fascia. In the type V injury the fascia of the deltoid and trapezius is extensively stripped away from the bone. This condition is evident when the patient performs a shoulder shrug and the AC joint space does not reduce. Radiographically, the space between the clavicle and the acromion increases 100 to 300%.

Figure 5–4 Step-off deformity is a clinically distinguishable sign that is noticeable in type III acromioclavicular joint injuries.
Type VI The type VI injury, although rare, is characterized by the inferior migration of the distal clavicle. Clinically, the acromion will be prominent on palpation with an obvious step down to the clavicle. It has been reported that occasional transient paresthesia accompanies this dislocation; however, it subsides with reduction.14 Radiographically, the distal clavicle will be subluxed under the coracoid or acromion.
 Treatment of Acromioclavicular Injuries
Treatment of Acromioclavicular Injuries
Although the focus of this book is on non-operative treatment approaches, it is difficult to discuss the AC joint without the often-debated surgical versus nonsurgical treatment approaches. The consensus is that types I and II AC joint separations are best treated with a conservative approach, whereas types IV through VI are best addressed with one of many surgical approaches; AC ligament repair, dynamic muscle transfer, CC ligament reconstruction, or CA ligament transfer. The greatest area of debate is the treatment decision making for type III AC joint injuries. In a literature review by Phillips et al,15 88% of surgically treated patients reported a satisfactory outcome; 87% of nonsurgically treated patients had a satisfactory outcome. A meta-analysis of the mix data from these studies showed no significant benefit from surgery.15 There are over 32 methods of conservative treatment16 and over 60 surgical procedures17 that have been described to date; hence, this is a long-running debate. The most recent comparative studies between conservative and operative treatment for type III injuries have determined that nonoperative outcomes are as good, if not better, than current surgical procedures.18–21 Conservatively treated patients have been found to return to work and activities faster than patients who received surgical treatments.19 Considering outcome studies like these, a higher rate of patients will pursue a nonoperative approach to grade III AC joint injuries.
A properly designed rehab program for a nonoperative AC joint injury must be developed to address the functional needs of each specific patient. Professional and amateur athletes, the construction worker, as well as the sedentary desk worker can incur AC joint injuries. Each program must be designed with the patient’s functional demands in mind. A well-designed program will address the five coexisting areas that make up the functionality of our upper extremities; range of motion (ROM), kinesthetic awareness, proprioception, neuromuscular control, and strength (Fig. 5–5). We will now review the goals, steps, and importance of each of the rehabilitation stages: the protective phase, the early mobility and stability phase, the late mobility and stability phase, and the return to activity phase.
Treatment of Type I and II Injuries
The nonoperative treatment of a type I AC joint injury will often not be medically treated because patients typically ignore the injury. If medical care is provided, however, the primary treatment goals are to (1) regulate the pain response, (2) promote a healing environment as well as protect the damaged tissue, and (3) deter ROM loss. These objectives are inherent in the protective phase of rehabilitation.
Immediate care during the protective phase will include icing the injured area incrementally and positioning the arm in an arm sling for up to 1 week. Passive or active assisted ROM exercises are recommended during this period to create nourishment to the articular cartilage and promote collagen synthesis and organization. These may include early supine IR and ER motions beginning at the neutral position and progressing to the scapular plane. It is important that patients use their pain as a guide to ROM exercises. Excessive stressing of the damaged tissues may initiate an excessive inflammatory response.
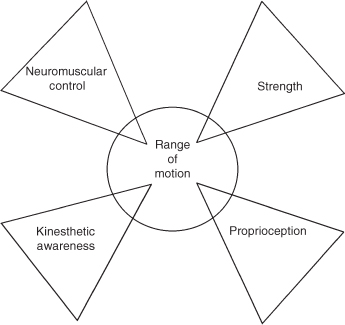
Figure 5–5 A well-designed program will address the five coexisting areas that make up the functionality of our upper extremities: range of motion, kinesthetic awareness, proprioception, neuromuscular control, and strength.
Early treatment (the protective phase) of a type II injury is important because of the complete disruption of the AC joint ligament. Although the CC ligaments are still intact, the horizontal and axial stability of the AC joint is compromised because of the loss of the AC ligament. To maximize the healing and essential scarring to realign the AC joint, it is recommended that the patient wear a Kenny Howard sling or an AirCast AC Joint Sports Sling (Aircast Corp., Summit, NJ) (Fig. 5–6) for up to 3 weeks. If an AC joint sling is not available, for the patient’s comfort a standard shoulder sling should be worn for up to 3 weeks. During this phase of the rehabilitation, the application of ice is recommended to control swelling and to alleviate pain. The important steps taken in the protective phase include (1) educating patients on their injury and rehabilitation, (2) maintaining ROM, and (3) diminishing pain levels.

Figure 5–6 An AirCast acromioclavicular Joint Sports Sling is often prescribed to approximate the injured joint and relieve the weighted arm from distraction.
For the other three phases of rehabilitation, we follow the guidelines for a type III, however progress at a faster pace; we sometimes progress through a stage in a day or two. Patients typically return to activities and sports within 2 to 4 weeks, once full ROM and strength are normal. For contact sports like football and hockey, a protective pad placed over the AC joint is recommended to add protection to the joint (Fig. 5–7).
Treatment of Type III Injuries
Protective Phase
A type III injury is addressed as in a type I/II injury; however, during a type III injury to the AC joint, patients will have a noticeable deformity immediately and will generally have an elevated level of pain because of the structures compromised. With the disruption of the AC ligaments, the CC ligaments, and the possibility of fascia damage to the trapezius or deltoid, patients will present with excessive pain that must be addressed during this protective phase. During this stage, the primary treatment goals are to (1) protect the damaged tissue and promote a healing environment, (2) deter ROM, and (3) regulate the pain response.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree