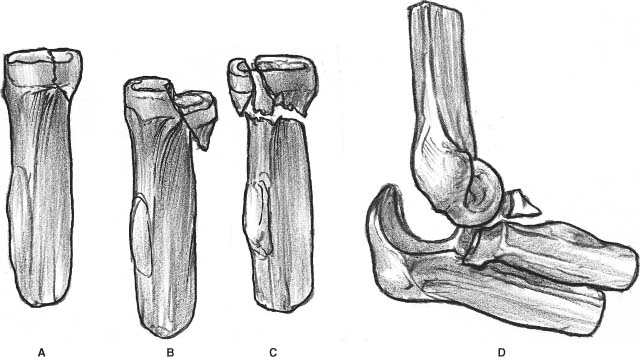
2 Fractures of the radial head are a very common injury of the elbow joint, and their proper management is still difficult and controversial. The radial head is considered a multifunctional stabilizer of the elbow. It provides stability of the elbow in three planes. In association with the medial collateral ligament (primary stabilizer), it prevents valgus instability in the coronal plane.1 The posterolateral ligamentous structures, along with the coronoid process and the medial ligaments, prevent posterior dislocation in the sagittal plane. In the axial plane, it works with the interosseous membrane to prevent the shaft of the radius to ride up. Although it represents the most common single fracture of the elbow in adults, it is often misdiagnosed because symptoms are similar to elbow sprains. Radial head fractures usually result from a fall onto the outstretched hand. Thus, a history of a similar mechanism of injury, painful rotation of the forearm, tenderness at the lateral aspect of the elbow, and loss of its full extension should be considered as a radial head fracture (or should suggest the diagnosis), unless a negative radiograph is obtained. This type of fracture may be isolated or associated with more complex injuries such as fractures and dislocations around the elbow, soft tissue injuries, and rupture of the distal radioulnar joint. A fracture of the radial head is a common injury as a result of indirect trauma and constitutes approximately one third of all fractures and dislocations of the elbow. Radial head fractures are involved in approximately 20% of elbow trauma cases,2 and 5 to 10% of elbow dislocations are associated with a radial head fracture.3,4 Eighty-five percent of fractures occur in adults between 20 and 60 years of age (mean age 30–40 years), and the ratio between males and females is approximately 1:2.5 Undisplaced or minimally displaced fractures represent 40 to 60% of all the fracture types seen.6 The vast majority of fractures of the radial head are provoked after a fall with the arm abducted and the elbow between 0 and 80 degrees of flexion, as shown by Amis and Miller in their cadaver study.7 The force of the fall at the moment of injury is of varying value and results in a valgus pronation force that is transmitted across the proximal radius to the elbow. The radial head is pushed against the capitellum and may be split or broken. The articular cartilage of the capitellum may be bruised or chipped, resulting in an injury not only to the radial head, but also to the capitellum. Occasionally, a fracture of the radial head may be a result of a valgus force to the elbow, and the injury may also become complicated by a fracture of the olecranon.8 A direct blow could also cause a radial head fracture, but it is considered uncommon.6 Although fracture of the radial head may be an isolated lesion, the displaced and often comminuted radial head fracture can be frequently associated with (1) a fracture of the coronoid process; (2) a torn medial collateral ligament that renders the elbow joint completely unstable to valgus stress; and/or (3) an injury to the interosseous membrane and the triangular fibrocartilage complex, causing axial instability of the forearm with subluxation of the distal radioulnar joint (Essex-Lopresti dislocation).9 Although the classification of the radial head fractures is a simple radiographic evaluation, the optimal classification that would be perfectly related to various treatment protocols and prognosis has yet to be established. Mason2 classified injuries to the radial head, and later Johnston10 modified this classification. The Mason classification is a purely radiographic one, and it has been proven insufficient to guide clinical treatment. Morgan et al11 demonstrated a poor reliability of classifying radial head fractures by the system of Mason. Additionally, Morrey4 reported that this classification is particularly useful for the simple (uncomplicated) radial head fractures. If the fracture is complex, the treatment plan is based on the associated injury.4,5 However, it has been traditionally used to characterize radial head fractures (Figure 2-1A-C). Mason type I are undisplaced fractures; type II, displaced, with involvement of more than 30% of the head and usually less than its half; and type III, comminuted fractures involving the entire head. Johnston10 has added the type IV category, which characterizes a concurrent radial head fracture and an ulnohumeral dislocation (Figure 2-1D). Mason did not include associated injuries, presenting as an acute mechanical block or tears of the interosseous membrane of the forearm that may influence the treatment and the final outcome after a radial head fracture. For that reason, many authors have attempted to propose modifications based on the physical signs and the associated injuries, beyond the pure radiographic fractures patterns. The Hotchkiss12 modification includes clinical examination and provides guidelines for the treatment of such injuries (Table 2-1). The Schatzker8 classification divides radial head fractures into three types: type I, split-wedge fracture; type II, impaction fracture; and type III, severely comminuted fracture. The Arbeitsgemeinschaft für Osteosynthesefrage (AO) classifies the different fracture patterns into simple (21-B2.1), multifragmentary without depression (21-B2.2), and multifragmentary with depression (21-B2.3).13 Although this classification is good for coding purposes, it is not very helpful for daily practice and does not indicate the severity of the articular head fracture.8 FIGURE 2-1. Mason-Johnston classification of radial head fractures. (A). Type I, undisplaced. (B). Type II, large, displaced fragment. (C). Type III, comminuted. (D). Type IV, associated with elbow dislocation. Morrey5 reported one additional level of classification (Mayo classification), which can be expressed in several ways: uncomplicated and complicated, simple and complex, or with or without associated injury. The additional injury in complicated fractures may be either another fracture or ligament injury or both (Figure 2-2). Complicated injury patterns about the elbow joint are considered as complex elbow instability. The degree of ligamentous injury that occurs with a radial head fracture is not always fully appreciated. Previous investigators have reported various results with regard to the incidence of associated bony or ligamentous injuries.9 The combination of a radial head fracture with attenuation or tear of the medial collateral ligament has been reported to occur in 1 to 2% of patients.5 Roidis et al14 reported on the results of an MRI evaluation of 24 consecutive patients with an acute radial head fracture (Mason types II and III) without documented dislocation or tenderness at the distal radioulnar joint (DRUJ). The evaluation was done with elbow antero-posterior and lateral x-ray images and magnetic resonance imaging (MRI) performed with the patient in a splint in sagittal, coronal, axial, axial oblique, and coronal oblique planes.15 The authors investigated the integrity of both medial and lateral collateral ligaments, as well as the presence of capitellar osteochondral defects or bone bruises and loose bodies. The MRI evaluation of the participants in this study revealed the presence of a high percentage of ligamentous injuries. The incidence of associated injuries was the following: medial collateral ligament not intact: 13/24 (54.16%), lateral collateral ligament not intact: 18/24 (80.1%), both collateral ligaments not intact: 12/24 (50%), capitellar osteochondral defects 7/24 (29.1%), capitellar bone bruises 23/24 (95.83%), and loose bodies 22/24 (91.67%).
Radial Head Fractures
Anatomy
Incidence and Mechanism of Injury
Classification
| Type | Characteristics | Functional limitations |
| Type I | Nondisplaced or minimally displaced fracture of head or neck | Foramen rotation (pronation/supination) is limited only by acute pain and swelling No mechanical block Intra-articular displacement of the fracture is usually less than 2 mm or a marginal lip fracture |
| Type II | Displaced (usually greater than 2 mm) fracture of the head or neck (angulated) | Motion may be mechanically blocked or incongruous Technically possible to reduce and repair by open reduction with internal fixation (without severe comminution) Fracture involves more than a marginal lip of the radial head |
| Type III | Severely comminuted fracture of the radial head and neck | Judged not reconstructable by radiograph or during surgery Usually requires excision for movement (delayed excision should be considered) |
| All of these fractures may be associated with posterior elbow dislocation with or without coronoid fracture, interosseous ligament injury of the forearm, and/or injury to the triangular fibrocartilage complex of the wrist. | ||
| Adapted from Hotchkiss RN. Fractures of the radial head and related instability and contracture of the forearm. In: W. Dilworth Cannon, Jr., ed.Instructional Course Lectures. American Academy of Orthopaedic Surgeons; 1998:173–177. | ||
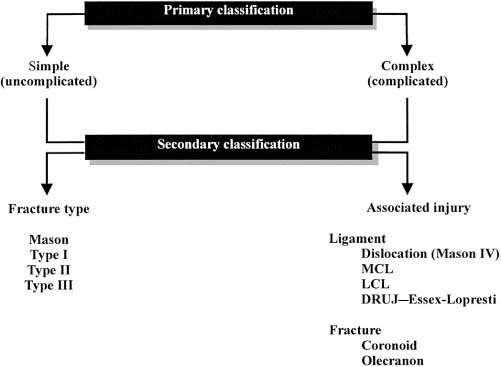
FIGURE 2-2. Mayo classification and radial head fracture, including consideration and associated injuries (Adapted from Morvey BF. Radial head fracture. In: Morvey BF, ed. The Elbow and its Disorders, third ed. Philadelphia: WB Saunders, 2000.) DRUJ, distal radioulnar joint; LCL, lateral collateral ligament; MCL, medial collateral ligament.
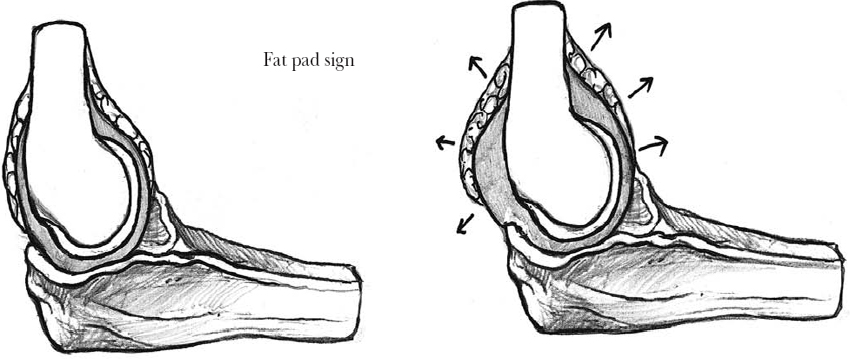
FIGURE 2-3. Displaced anterior and posterior fat pads may be the only sign of an undisplaced fracture.
The results of this study clearly showed a high incidence of osteochondral and ligamentous injuries in cases of radial head fractures initially presented as uncomplicated, questioning the validity of the radio-graphic classification systems. Radial head fractures that initially present as uncomplicated—displaced or comminuted (Mason types II and III)—may have some associated ligamentous injuries that dramatically alter the classification, the prognosis, and the appropriate treatment protocols. The cost per MRI examination is very high and is not recommended as part of a routine preoperative work-up. It is absolutely necessary to perform a detailed clinical and radiographic examination in every case of comminuted radial head fracture. Careful intraoperative examination performed under fluoroscopy may be helpful in determining the presence of associated ligamentous injuries. Because of the high incidence of intra-articular loose bodies, careful intraoperative evaluation and irrigation of the joint should be performed. A high level of suspicion should be employed when treating this type of fracture because concomitant osseous, osteochondral, and/or ligamentous injuries may be present. In that way, an “uncomplicated” fracture may actually be a complicated fracture leading to elbow instability that can be very easily misdiagnosed.
Diagnosis
Most radial head fractures can be diagnosed with a careful history and physical examination, as well as by a standard radiographic evaluation with anteroposterior and lateral projections of the elbow. The direction of the beam in anteroposterior projection must be perpendicular to the radial head because the elbow joint can rarely be extended.16 The radiographic evaluation may reveal a vertical split or a single fragment of the lateral portion of the head, usually displaced distally, or multiple fragments of the radial head. The radial head-capitellum view can be useful in identifying fractures of the posterior half of the radial head.17 The presence of a fat pad sign refers to intra-articular hemarthrosis and sometimes is the only visible radiographic sign in an undisplaced radial head fracture (Figure 2-3). An additional radiographic evaluation of the wrist should be made if pain is present to exclude injury of the DRUJ. Although concomitant injury to the capitellum (bruised or chipped) is an important complication, it may not be established radiographically. Tomograms or computed tomography (CT) scans about the elbow joint may be useful in defining the comminution and the degree of displacement, especially when open reduction and internal fixation are considered.
Treatment
Historically, Helferich in 1897 suggested excision of the radial head as a treatment method, as quoted by Schwartz and Young in their review for the treatment of radial head fractures.18 Brockman in 1930 described two cases of symptomatic proximal migration of the radius after radial head excision.19 Watson-Jones in 1940 recognized the hazards of early excision of the radial head when associated with disruption of the elbow and recommended delayed excision.20 Odenheimer and Harvey in 1979 reported internal fixation of radial head fractures with wires.21 It is evident that although radial head fractures are considered a relatively benign injury,22 their treatment is of great importance and has developed over the years by using various techniques and methods.
The principal goal of treatment is to maintain good elbow function and, thus, to retain adequate motion and joint stability. In general, according to Morrey,5 the treatment of radial head fractures is based on the fracture type and the presence of any associated injury (complicated or uncomplicated fractures).
Type I: Undisplaced Fractures
There is no doubt that radial head fractures with no or minimal displacement should be treated conservatively. As early as 1943, Mason and Shutkin established the preferred method of treatment to be early motion.23 The early motion is helpful to maintain the shape and molds slight incongruities without risk of further displacement.12,24 Aspiration followed with or without instillation of local anesthetic into the elbow joint helps to decompress the joint from hematoma and thus reduces pain (Figure 2-4). It also allows the joint’s range of motion to be evaluated, thus identifying the presence or absence of bony blocks. Holdsworth et al25 found that aspiration, although a safe procedure, which improved the initial range of motion and provided pain relief, did not alter the final outcome.
Several positions of immobilization have been advocated for the treatment of these fractures. Thompson26 and Unsworth-White et al27 in their studies compared flexion versus extension splinting in the treatment of Mason type I fractures. Both studies showed that splinting in full extension is better than 90 degrees of flexion. The loss of extension in their group of patients was less than 10 degrees in comparison with the other groups.
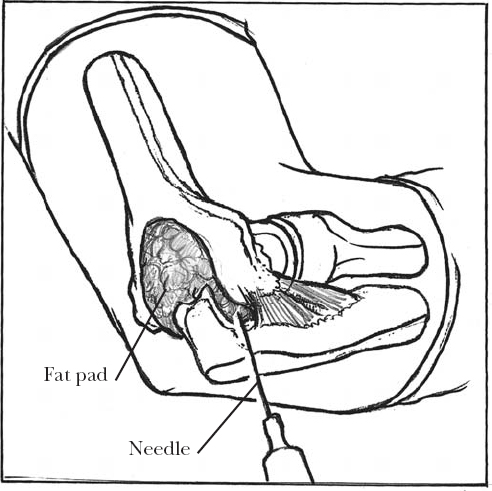
FIGURE 2-4. Aspiration of the hemarthrosis can provide pain relief and allow the examiner to assess range of motion of the elbow. The needle is inserted in the center of a triangle (known as the “soft spot”) formed by the radial head, lateral epicondyle, and tip of the olecranon.
Patients with type I fractures usually obtain good to excellent restoration of elbow function after 2 to 3 months of active motion exercises. Early motion compared with prolonged immobilization appears to offer advantages in elbow function.5 Early motion should be restricted for fractures that involve less than one third of the articular surface in the elderly or low-demand individuals. Active patients with undisplaced fractures involving more than one third of the articular surface should be splinted for a minimum of 2 weeks, followed by protected motion for an additional 7 to 10 days.22 Good results in type I fractures can be expected in 86 to 100% of patients.6,28 Minimal loss of elbow extension and forearm rotation is not uncommon, but the loss rarely affects arm function. Contracture, occasional pain, and inflammation are uncommon. Displacement and nonunion are rare and are treated by osteosynthesis or delayed excision of the radial head. Occasionally, osteochondral fracture of the capitellum may be responsible for a poor result in type I fractures.12
Type II: Displaced Fractures
Early studies advocated either conservative management or excision of the radial head as the standard treatment for type II fractures.10,29 As knowledge increased, the understanding of the functional importance of the radial head as a secondary stabilizer to valgus stress and as an axial weight-bearing structure led to the better understanding of its biomechanics and dictated treatment options. Currently, a variety of techniques have been developed based on the specific type (degree of displacement) of fracture being treated, but the final choice of treatment is still controversial.
The evaluation of the mechanical block is highly important for the final treatment decision, as not all of the marginal displaced fractures require internal fixation.4,30 Minimally displaced or undisplaced Mason type II fractures can be managed conservatively in a manner similar to that of type I fractures. MacAusland and Wyman stated that surgery is not advisable in the presence of 70 degrees of active pronation and supination regardless of the radiographic findings.31 If displacement occurs despite immobilization, a delayed radial head excision can be performed from 1 month to 20 years with 77% good or excellent results, as reported by Broberg and Morrey.32 Acute mechanical block in displaced type II fractures is best treated by open reduction and internal fixation, especially in young and active individuals. Preservation of the radial head should always be considered when associated injuries about the elbow and the forearm are present. Treatment options include open reduction and internal fixation, excision of the fragments, excision of the radial head, and prosthetic radial head replacement.
Open Reduction and Internal Fixation
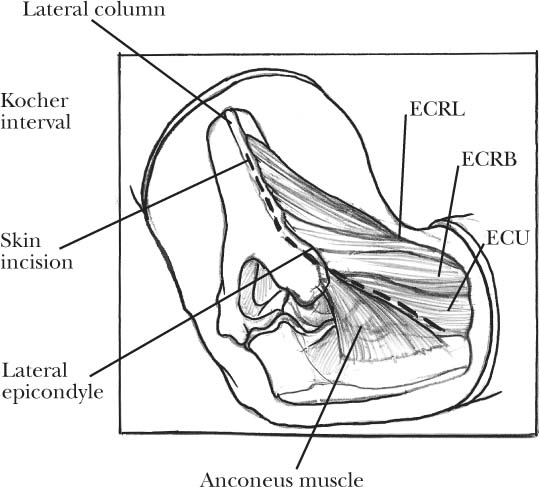
Currently internal fixation is popular because contemporary techniques have improved surgical outcomes.33 AO mini-screws and mini-plates (Synthes, Paoli, PA), Herbert screws (Zimmer, Warsaw, IN), and absorbable polyglycolide pins are used for the restoration of the fractured radial head and neck. An insertion of one or two 2.0 or 2.7 mm AO cortical mini-screws parallel to the radiohumeral joint can easily fixate isolated large fragments by using a posterolateral oblique approach (Kocher interval) to the elbow (Figure 2-5). Screw heads are countersunk, and care should be taken that the screw tips do not protrude out the articulating portion of the radial head. Impacted fractures of the head often require elevation to restore the articular surface. The defect beneath the elevated fragment is best filled with cancellous bone graft from the lateral epicondyle of the humerus.22
Hardware placement for the fixation of radial head fractures should not affect the proximal radioulnar joint. The nonarticulated portion of the radial head is referred to as the “safe zone” (Figure 2-6). The safe zone region corresponds to approximately 110 degrees of the radial head surface. Hotchkiss12 estimated the safe zone intra-operatively by reference marks onto the radial head during forearm rotation. Caputo et al34 define this zone as a portion of the radial head that lies between perpendicular axes through the radial styloid and Lister’s tuberosity.
Herbert screws can also used for radial head fractures alone, without extension of the fracture line to the radial neck. They provide a reliable and effective fixation. According to McArthur,35 Herbert screw fixation is the ideal treatment for type II fractures. It provides compression across the fracture and an accurate alignment of the screw without the need for a second surgery for implant removal.
Other treatment options include the use of fibrin adhesive glue that was described in a dog model.36 The use of absorbable polyglycolide pins as another alternative to metallic fixation has given good results without the need for removal by a second surgery.3,37
The partial excision of a displaced fragment, although advocated in the past,29 is not currently being used because it can lead to subluxation of the remaining radial head.5,6
When fractures are extended to the radial neck, the use of an AO mini-plate (2.0–2.7 mm) can be used to secure the head to the shaft of the radius (Figure 2-7). In the case of a comminuted radial neck fracture along the medial side, bone grafting should be considered to support the radial neck.38 When there is no concomitant fracture of the radial head, the use of an intramedullary pin is advisable.39 Patterson et al40 reported the results of a comparative study between different plates for the fixation of radial neck fractures. They concluded that the two important variables affecting construct stiffness are plate thickness and incorporation of a fixed-angle plate. The optimal position for the placement of the plate in complex fractures of the proximal radius associated with neck dissociation is the direct lateral position in neutral rotation.41