Quadriceps Tendon Repair
Patient Presentation and Symptoms
The quadriceps tendon disruption is usually caused by landing on a flexed knee during an eccentric muscle contraction. It is associated with intense pain, and the patient typically seeks immediate medical attention.
Indication
Complete disruption of the extensor mechanism
Contraindication
Open wounds may necessitate a staged repair.
Physical Examination
- Swelling and tenderness to palpation at the superior pole of the patella
- Palpable defect of the quadriceps tendon
- Subcutaneous hemarthrosis
- Inability to perform a straight leg raise or presence of an extensor lag
- Difficulty ambulating
Diagnostic Tests
- Anteroposterior (AP) and lateral radiographs will show patella baja.
- Magnetic resonance imaging (MRI) will demonstrate partial versus complete disruptions.
Special Considerations
After the initial discomfort subsides, symptoms may dissipate, especially if either the medial or lateral retinaculum is intact. In a complete rupture, the knee cannot be extended from either a flexed or supine position. In varying degrees of incomplete rupture, the patient may be able to perform a straight leg raise in an extended position but not from a flexed position.
Preoperative Planning and Timing of Surgery
Early intervention is desirable and yields the best results. Neglected chronic ruptures are less satisfactory.1 Often there is retraction of the tendon and a large gap between the tendon edges or osteotendinous junction. Special techniques may be employed to obtain repair in chronic ruptures.
Special Instruments
- Tourniquet
- Anterior cruciate ligament (ACL) Beath pin
- Power drill
- No. 5 nonabsorbable sutures/Fiberwire™ (Arthrex)
- No. 2 nonabsorbable sutures/Fiberwire
- 5-mm Mersilene tape
- Allograft tendon (anterior tibialis, hamstring) for chronic ruptures
Anesthesia
Options are general anesthesia, spinal anesthesia, or femoral nerve block.
Patient Position
Supine position
Surgical Procedure
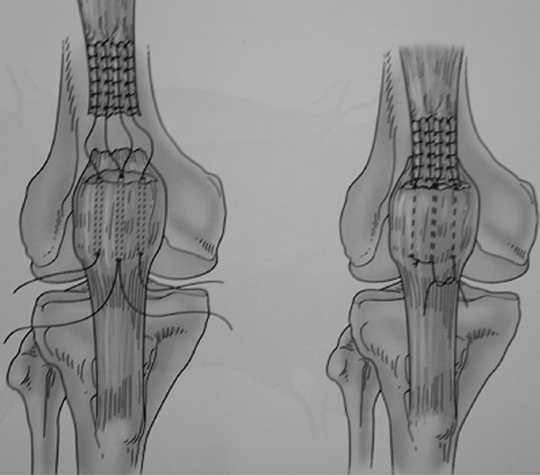
Acute Ruptures (Fig. 32–1)
- Make a straight midline incision four fingerbreadths above the superior pole of the patella to the inferior pole. Expose the entire extensor mechanism including the medial and lateral retinacula.
- The torn quadriceps tendon is identified and debrided back to healthy tissue without excising healthy tendon.
- If the rupture occurs at the osseous tendon junction, the proximal end of the rectus femoris and vastus intermedius tendon is cut fresh and the superior pole of the patella is debrided of residual tendon.
- A transverse trough is created in the superior pole of the patella near the articular surface to avoid patellar tilt.
- A No. 5 nonabsorbable suture is secured with an interlocking stitch (Krackow or Bunnell) in the medial half of the quadriceps tendon exiting at the tendon edge. Similarly a suture is passed in the lateral half of the tendon.
- Three longitudinal interosseous holes are created from proximal to distal approximately 1 to 1.5 cm apart, roughly dividing the patella equally.
- The free ends of the suture are passed interosseously with a Keith needle, suture retriever, or ACL Beath pin through the patella proximal to distal.
- The lateral-most and medial-most sutures are passed through their respective holes while the center two suture ends are passed through the central hole.
- The proximal end of the tendon is pulled into the trough and held with a clamp while the knee is flexed so that patellar tracking can be assessed. The repair is completed by tying the No. 5 nonabsorbable sutures distally. The repair of the retinacula is done with interrupted No. 2 nonabsorbable suture.
- If there is a tendon stump remaining on the superior pole of the patella, the repair can be performed with multiple interrupted No. 2 nonabsorbable sutures. The retinaculum is adequately tensioned with interrupted sutures.
- Alternatively, the Scuderi technique can be utilized to repair acute quadriceps tendon ruptures. The technique utilizes a distally based inverted triangle approximately 5 cm proximal to the rupture. The flap is folded distally over the rupture and sutured in place to the patella.2 A pullout wire is then placed about the repair and removed at 3 weeks (Fig. 32–2).
- With Mesiline tape the repair can be protected internally with a cerclage suture passed transversely through the midpatella and proximal to the rupture. This is tied with the knee at 45 degrees of flexion.
- The wound is closed in layers over a Hemovac drain.
- Three longitudinal interosseous holes are created from proximal to distal approximately 1 to 1.5 cm apart, roughly dividing the patella equally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








