A. Overview—Fractures of the proximal humerus are classified according to the patterns of displacement of the four major segments. These include the humeral head, the greater and lesser tuberosities, and the humeral shaft. A proximal humerus fracture is considered displaced if any major segment is displaced more than 1.0 cm or angulated greater than 45°. As described by Neer, this classification system is based on anteroposterior and lateral radiographs. Recently, the use of three right-angle trauma series radiographs has improved the accuracy in diagnosing fracture displacement. Computed tomography (CT) can be helpful in preoperative planning by delineating the degree of displacement and rotation of the fracture fragments, especially with fractures that involve the tuberosities and humeral head.
Proximal humerus fractures comprise 4% to 5% of all fractures. In younger patients, these fractures are commonly associated with violent trauma, whereas in older patients, minor trauma and decreased bone mineral density lead to the majority of proximal humerus fractures.
The proximity of the neurovascular bundle to the glenohumeral joint makes it subject to injury with proximal humeral fractures, and necessitates a thorough neurovascular examination. The finding of a palpable distal pulse does not eliminate the possibility of a vascular injury due to the rich collateral circulation of the proximal humerus.
The majority of proximal humerus fractures are minimally displaced and can be treated with immobilization and early range of motion. Displaced fractures are optimally treated by closed or open reduction to restore anatomic alignment. In some cases, prosthetic replacement is the treatment of choice based on the disruption of the blood supply to the humeral head.
B. Physical Examination
1. Shoulder—The shoulder must be well visualized. Gowns are used to expose the entire shoulder for women, while men can be undressed from the waist up.
2. Cervical spine—The cervical spine should be examined prior to the shoulder, and radiographs obtained if there is any concern of concomitant injury.
3. Neurovascular examination—The neurovascular evaluation of the extremity is essential and can usually be obtained in a fractured extremity with gentle motion and isometric contraction. The presence of sensibility in the axillary distribution (lateral arm) is not a reliable test of the integrity of axillary motor function. Neurovascular injuries occur in 5% to 30% of complex proximal humerus fractures.
C. Imaging
1. Radiographs
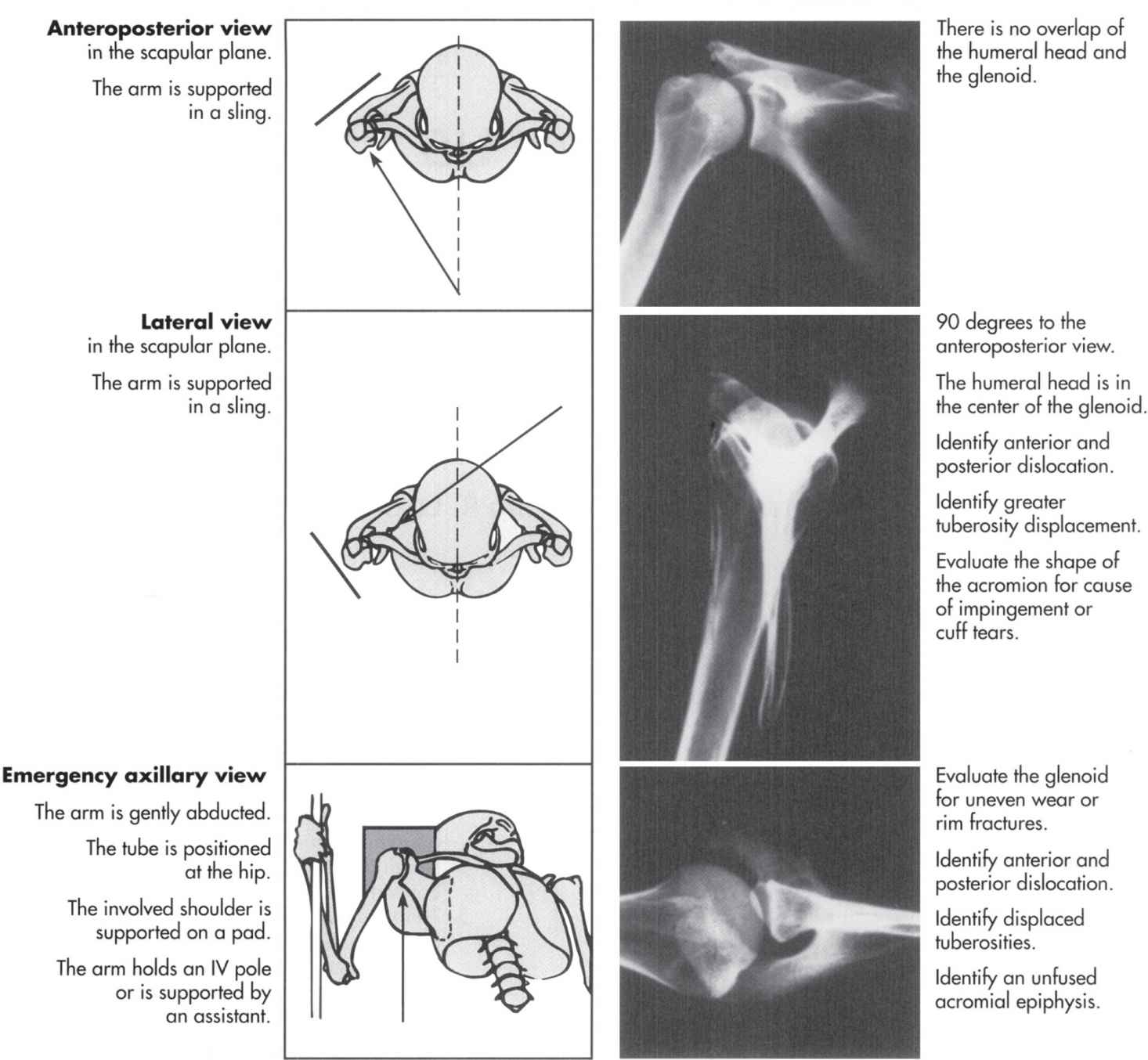
• Trauma series (Fig. 19-1)—Three right angle views of the shoulder are essential to determine the relationship of the four major segments of the shoulder in space. These views are taken in the sagittal, coronal, and axial planes of the scapula, rather than the body.
FIGURE 19-1 Trauma series views of the shoulder (From Norris TR. In: Chapman MW, Madison M, eds. Operative Orthopaedics. Philadelphia, PA: JB Lippincott; 1988, with permission.)
• Rotational anteroposterior (AP) views—Supplement to the trauma series, these views reveal the greater tuberosity in external rotation and humeral head impression fractures with internal rotation.
2. CT scanning
• Low-dose CT scanning—Low-dose CT provides extremely accurate imaging to evaluate complex proximal humeral fractures, and in some cases can change the treatment plan as contemplated, based on the initial radiographs.
• Three-dimensional CT scanning—3D CT is now available in many institutions using the standard data obtained from the initial scan. These images allow depiction of the relationship of the fractures in any direction.
3. MRI scanning—MRI is used in the determination of soft-tissue injuries involving the rotator cuff and the neurovascular structures around the shoulder. MRI also allows early assessment of osteonecrosis following trauma, which may not be evident on plain films for a number of years.
4. Arteriography and venography—Arteriography and venography are required when a vascular injury is suspected, as the finding of a distal pulse does not rule out an arterial injury. The circumflex vessels connect with the profunda brachii through the ascending deltoid vessels and feed the distal arteries. Arterial injuries are more likely to be seen with traumatic dislocations in the elderly secondary to noncompliant, atherosclerotic vessels. Venous duplex ultrasound scanning in indicated for suspected injuries to the subclavian or axillary vein.
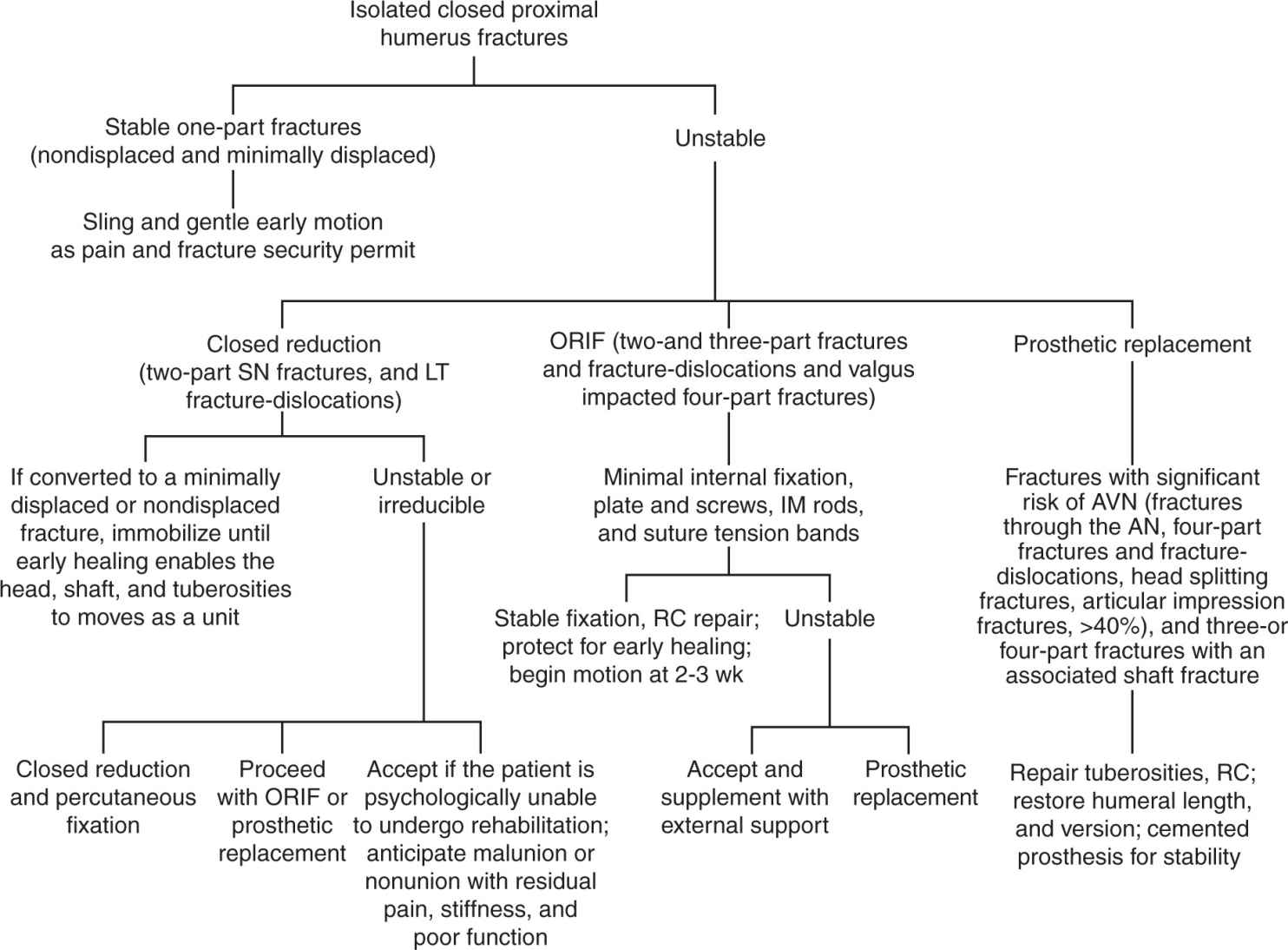
D. Injury Classification and Treatment (Figs. 19-2 and 19-3)
1. One-part fractures—Fractures without displacement of 1 cm are not likely to disrupt the blood supply to the humeral head and are referred to as minimally displaced. The surrounding soft tissues (periosteum, capsule, and rotator cuff) tend to hold the fragments together and allow near anatomic healing. These fractures are optimally treated by immobilization and early functional exercises to avoid stiffness. Functional outcome improves if physical therapy is initiated within 2 weeks of the injury.
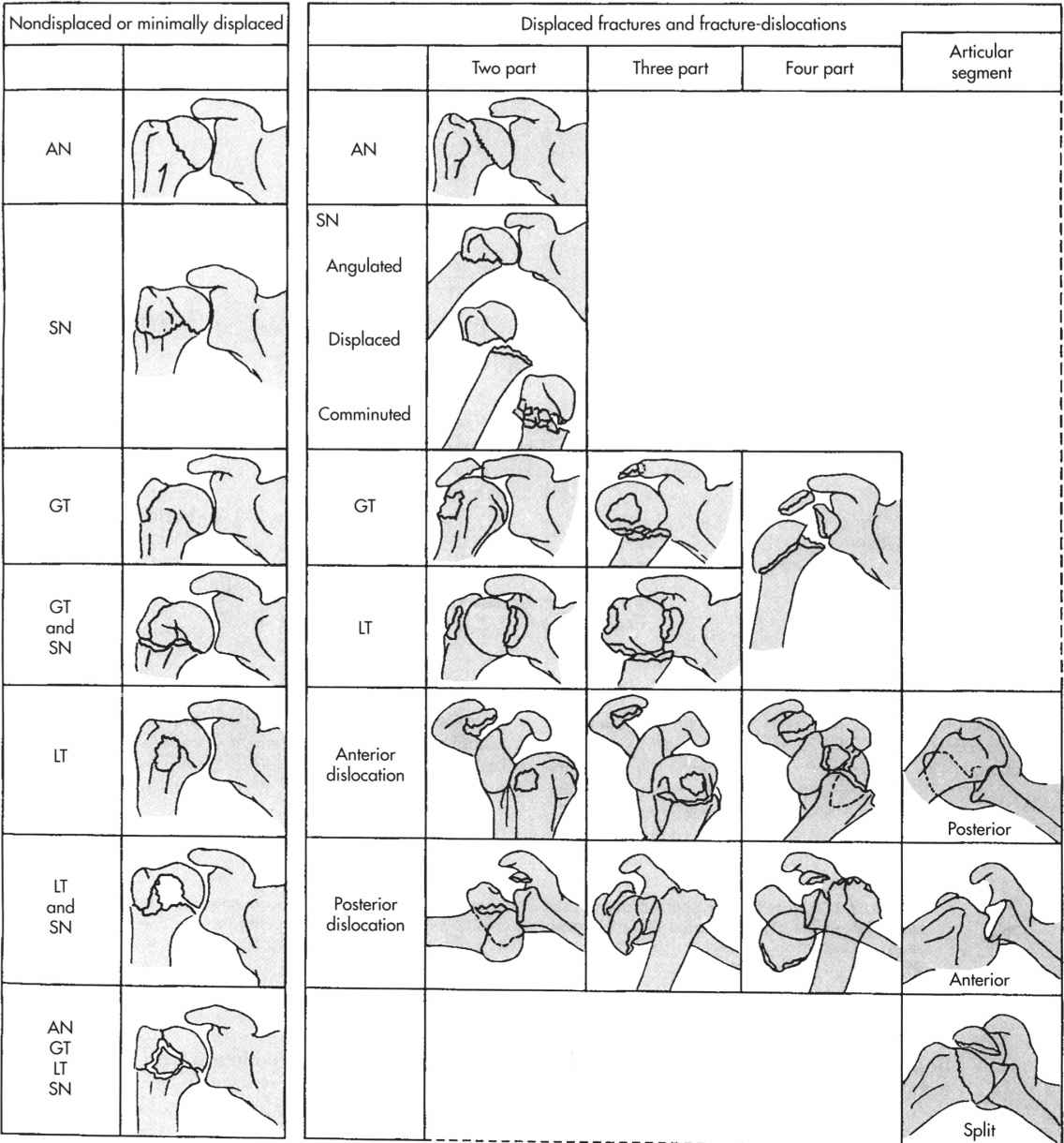
FIGURE 19-2 Four-part classification of proximal humerus fractures and fracture-dislocations. AN, Anatomic neck; GT, greater tuberosity; LT, lesser tuberosity; SN, surgical neck. (Redrawn from Browner BD, Jupiter JB, Levine AM, et al., eds. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries. Vol 2, 2nd ed. Philadelphia, PA: WB Saunders; 1998, with permission.)
FIGURE 19-3 Algorithm for isolated closed proximal humerus fractures. AN, Anatomic neck; AVN, avascular necrosis; IM, intramedullary; LT, lesser tuberosity; ORIF, open reduction with internal fixation; RC, rotator cuff; SN, surgical neck. (Reprinted with permission from Browner BD, Jupiter JB, Levine AM, et al., eds. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries. Vol 2, 2nd ed. Philadelphia, PA: WB Saunders; 1998.)
2. Two-part fractures—Isolated two-part fractures involving the tuberosities are rare, and usually occur as a consequence of a glenohumeral dislocation.
• Two-part lesser tuberosity fractures—Usually associated with posterior glenohumeral dislocation. Axillary radiographs and CT scanning are useful in confirming the diagnosis. Displaced fragments require open reduction and internal fixation.
• Two-part greater tuberosity fractures—May accompany an anterior glenohumeral dislocation and are associated with longitudinal tears of the rotator cuff. Surgical treatment is indicated for fractures with more than 0.5 cm of displacement or 45° of rotation, with repair of the rotator cuff.
• Two-part surgical neck fractures—Classified as impacted and stable or displaced and unstable. Treatment for displaced fractures includes open reduction and internal fixation versus percutaneous pin fixation.
3. Three-part fractures—Include displacement of three segments including the humeral head, the shaft, and one tuberosity. Closed reduction is difficult to obtain due to the unopposed muscle pull on the remaining tuberosity. Axillary radiographs allow best visualization of the rotation of the articular surface of the humeral head. Open reduction and internal fixation using tension band wiring which incorporates the rotator cuff tendon provides good fixation. Prosthetic replacement is indicated when secure fixation cannot be obtained, usually in elderly patients with osteoporotic bone.
4. Four-part fractures—Each major segment is displaced, and the articular surface is devoid of soft tissue, increasing the risk of osteonecrosis. Open reduction and internal fixation is indicated in young patients with good bone quality, or with valgus impacted four-part fractures where the impacted head still has an intact medial soft-tissue hinge. Prosthetic replacement is often the preferred method of treatment. In patients with significant preexisting glenoid arthrosis, glenoid resurfacing is also indicated. Proper tension of the cuff musculature with near anatomic positioning of the tuberosities and restoration of humeral length is critical for functional recovery. Following prosthetic replacement, early passive motion is imperative to prevent stiffness. Active motion should be delayed for 8 to 12 weeks until the tuberosities have firmly united to the humeral shaft.
5. Fracture-dislocations—Often the result of high-energy injuries, these fractures are distinct from the previously classified fractures in that they carry a higher risk of neurovascular injury. Posterior fracture dislocations are often missed due to poor radiographic evaluation, thus necessitating the three view trauma series in all shoulder injuries.
6. Head-splitting fractures—Head-splitting fractures are most commonly treated with hemiarthroplasty; however, if large fragments and good bone quality are present, open reduction and internal fixation can be attempted. Articular impression fractures are commonly associated with chronic dislocations, and stability usually depends upon the percentage of articular surface defect. Defects less than 20% tend to be stable after immobilization, whereas defects up to 40% or more may require soft-tissue transfers or hemiarthroplasty.
E. Complications
1. Nonunion—A number of factors can lead to nonunion of proximal humerus fractures including inadequate fixation or immobilization, traction at the fracture site, soft-tissue interposition, and osteonecrosis. Nonunion most commonly occurs in patients with two-part surgical neck fractures. Treatment is aimed at anatomic reduction and stable fixation of the fracture fragments as described for acute fractures. When this goal cannot be met, prosthetic replacement is the treatment of choice.
2. Malunion—Malunions are often associated with stiffness of the shoulder or blocked range of motion. Treatment involves correcting the underlying restriction whether involving the release of soft tissues or osteotomies to restore normal anatomy. In cases where traumatic arthritis has developed, or inadequate bone stock remains after correction, hemiarthroplasty or total shoulder replacement may be indicated.
3. Avascular necrosis—Avascular necrosis usually occurs following three- or four-part fractures treated either closed or open, where the blood supply to the humeral head is compromised. The primary blood supply to the humeral head is the arcuate artery, which is a continuation of the ascending branch of the anterior humeral circumflex artery. Open procedures using plates and screws are associated with a higher incidence of avascular necrosis than tension band wiring or pinning due to extensive soft-tissue stripping. Treatment is based on the presentation of symptoms as a consequence of the avascular necrosis. Collapse of the humeral head may lead to the development of traumatic arthritis and disabling pain. Early prosthetic replacement may eliminate the need for soft-tissue releases, which may be necessary after longstanding collapse of the humeral head.
4. Neurologic injury—The musculocutaneous nerve is at risk of injury from proximal humerus fractures, dislocations, or excessive traction of the conjoint tendon during open reduction and internal fixation. Symptoms can present as numbness and tingling along the anterolateral aspect of the forearm, which is supplied by the terminal branch of the musculocutaneous nerve, the lateral antebrachial cutaneous nerve.
5. Arthrodesis—Indications include a young patient with nonfunctioning shoulder musculature, prior deep infection, loss of articular cartilage, and severe pain refractory to conservative treatment. The shoulder should be positioned in such a way that the arm rests comfortably without winging of the scapula and the hand can be used functionally: 20° of flexion, 30° of abduction and 40° of internal rotation is the optimal position for a shoulder arthrodesis.
II. Acute Dislocations of the Shoulder (Glenohumeral Joint)
A. Overview—Approximately 30% of the humeral head articulates with the glenoid at any given arm position (angle). The minimally constrained design of the glenohumeral joint affords it a wide arc of motion at the expense of inherent instability of the shoulder. Unlike the hip joint, the osseous structures of the glenohumeral joint contribute only a small portion to the joint’s overall stability. Rather, the surrounding soft tissues, which include the rotator cuff, glenoid labrum, and glenohumeral capsular ligaments, are of paramount importance in maintaining stability of the articulation.
1. Mechanism of injury—Patients with acute dislocations commonly note an episode of significant trauma. In the case of anterior dislocations, force applied to an abducted and externally rotated arm is usually involved. Such injuries can occur after a fall or motor-vehicle accident, or during contact sports. Posterior dislocations typically involve significant trauma and also can occur secondary to falls, car accidents, or seizure disorders.
2. Presentation
• Anterior dislocations—Patients with anterior dislocations typically manifest a loss of the normal deltoid contour. Palpation of the shoulder demonstrates prominence of the acromion process laterally and posteriorly, and a prominent humeral head can often be felt anteriorly. The arm is often maintained in a partial externally rotated and abducted position.
• Posterior dislocations—Posterior dislocations are not as common and represent approximately 5% of dislocations of the shoulder. Clinical deformities are not as evident, but can include prominence of the humeral head posteriorly and of the coracoid process anteriorly. There may be a mild loss of the normal deltoid contour with notable flattening anteriorly. The arm is typically held in an adducted and internally rotated position. Patients typically experience a loss of arm external rotation as the humeral head is wedged against the posterior aspect of the glenoid.
• Posterior subluxation—Recurrent posterior subluxation can occur after an initial posterior directed force on the humeral head relative to the glenoid in the elevated arm such as a baseball player sliding into base. It can also be a sequela after a primary posterior dislocation. Clinical findings typically include a posterior prominence during midranges of forward arm elevation that disappears with a palpable clunk during terminal elevation and abduction.
3. Physical examination—The evaluation of patients with acute dislocations should include a thorough neurovascular examination both before and after any attempts at closed reduction. Injuries to the axillary nerve and artery occur infrequently, but they should be noted. Few patients have an expanding subdeltoid hematoma, indicating an underlying vascular injury. Palpable distal pulses may be present despite an injury to the axillary artery because of the abundant collateral circulation surrounding the shoulder.
4. Radiographic evaluation—Standard radiographs should be obtained to confirm the direction of the dislocation and evaluate the shoulder for associated fractures and any possible obstructions to reduction. An AP view in the plane of the scapula, an axillary view, and the scapular lateral (Y) view can aid in the detection of glenoid rim fractures, articular impression fractures of the humeral head, and fractures of the tuberosities. A standard AP radiograph alone may not be sufficient for detecting posterior dislocations because the displacement typically occurs at a right angle to the plane of the film. On a normal AP radiograph, the humeral head typically fills the glenoid fossa. A vacant glenoid sign refers to a partial vacancy of the glenoid fossa, and a positive rim sign refers to a space between the anterior glenoid rim and humeral head of greater than 6 mm. These signs suggest a posterior dislocation as viewed on the AP film. The axillary radiograph remains the single most important X-ray film in assessing the presence and direction of a glenohumeral dislocation.
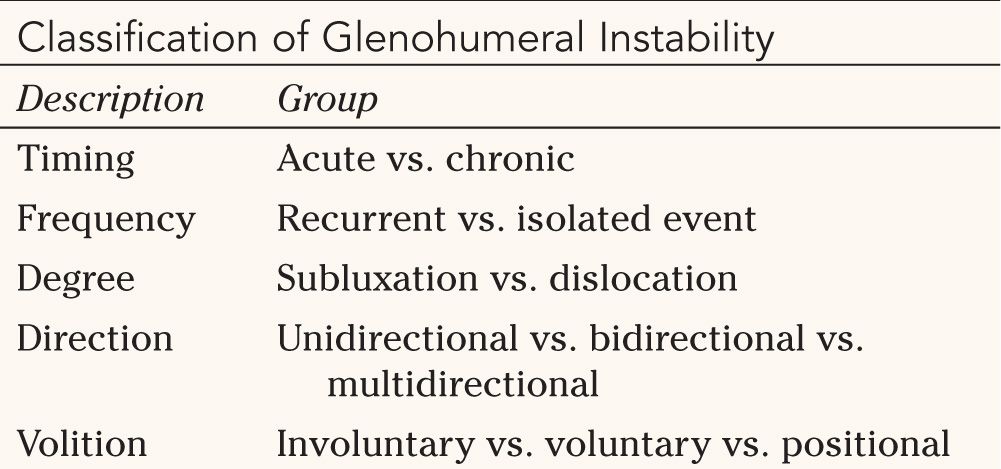
5. Classification (Table 19-1)—Glenohumeral instability has commonly been categorized into one of two groups: traumatic unidirectional and atraumatic multidirectional. However, instability can also be considered as a continuum with these categories at the extremes and varying forms in between. For example, an athlete with global glenohumeral ligamentous laxity may develop symptoms after a traumatic event and manifest findings consistent with both traumatic and atraumatic forms of instability. When glenohumeral instability is described, the timing, frequency, degree, direction, and volition should all be considered.


C. Associated Injuries
1. Axillary nerve palsy—The axillary nerve is vulnerable to injury as it courses along the anteroinferior aspect of the glenohumeral joint. The nerve may be subject to excessive compression and traction with luxation of the humeral head. The incidence of axillary nerve injuries after acute dislocation has been reported to range from 5% to 33%. Age, degree of trauma at the time of injury, and duration of the dislocation all appear to have an impact on both the incidence and prognosis of nerve injury. In addition, proximal humerus fractures, blunt trauma, and gunshot injuries all have been associated with axillary nerve palsy. EMG studies are indicated and can document the status of recovery 3 months after injury when physical examination reveals persistent absence of deltoid muscle function.
2. Vascular injury—Vascular injury is more commonly seen in elderly patients after acute dislocations. Stiffer, less pliable vessels predispose these patients to such injuries, which can involve the axillary artery or vein or branches of the axillary artery, including the subscapular, thoracoacromial, and circumflex arteries. Vessel damage may occur at the time of injury or during reduction. A loss or decrease in the radial pulse may not always be present because of the abundant collateral circulation. An expanding subdeltoid hematoma may be evident, and arteriography should be performed if the diagnosis is suspected.
3. Glenoid rim fracture—Displaced fractures involving more than 20% of the glenoid rim decrease the effective surface area of glenoid articulation and can predispose patients to recurrent instability. The anterior band of the inferior glenohumeral ligament inserts onto the glenoid labrum at the anteroinferior aspect of the glenoid rim. An avulsion fracture of this ligament will result in a bony Bankart lesion and occurs less frequently than an isolated soft tissue avulsion of the anteroinferior labrum from the glenoid rim (Bankart lesion). Malunion of such fractures also disrupts the concavity of the already shallow glenoid fossa, further compromising joint stability. Surgical treatment with anatomic reduction and fixation of the fractured fragments is recommended (Fig. 19-4).
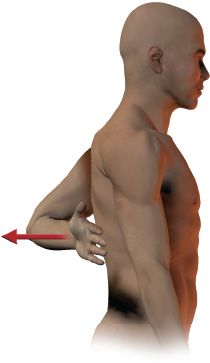
4. Rotator cuff tear—Rotator cuff tears occur in 14% to 63% of patients after acute anterior or inferior dislocations. The incidence increases in older persons and has been reported in 63% of patients over 50 years of age. Patients should be reevaluated 7 to 10 days after the initial injury to look for associated soft-tissue injuries. By 10 days the acute symptoms will have subsided to some degree and may allow for better evaluation of the rotator cuff. Typically, patients are unable to sufficiently elevate the arm in the post-injury period. There may be weakness in external rotation. The supraspinatus is commonly torn with variable degrees of infraspinatus involvement. Patients with recurrent anterior instability generally have disruption of the subscapularis tendon. An MRI is the study of choice when a rotator cuff tear is suspected. Satisfactory treatment can be achieved with primary repair of the tendon without reconstruction of the capsulolabral complex. The “lift-off test” described by Gerber can be performed to assess the functional integrity of the subscapularis. The arm is placed behind the back and the patient is asked to lift the hand from his back through further internal rotation of the arm. Inability to maintain the arm in this lifted position is a positive test suggestive of a subscapularis tendon tear (Fig. 19-5).
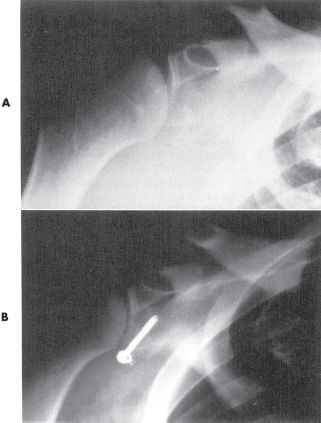
FIGURE 19-4 Preoperative (A) and postoperative (B) AP radiographs of a patient with a fracture of the anteroinferior glenoid rim associated with a traumatic anterior glenohumeral dislocation.
• Tensile failure—Traumatic lesions of the rotator cuff may also occur secondary to occult underlying instability. Such findings are more commonly seen in throwing athletes. It has been suggested that the rotator cuff lesions are the result of a continuum progressing from instability to subluxation, impingement, and tension overload of the cuff with resultant tearing. Articular surface partial-thickness tearing of the supraspinatus or subscapularis is commonly seen. Repeated mechanical stress causes failure of the glenohumeral static restraints and places increased demands on the dynamic stabilizers. The rotator cuff is subject to injury through both repetitive tensile loading and secondary impingement mechanisms.
5. Tuberosity fractures—Fractures of the greater tuberosity may occur in association with anterior dislocations. Although tearing of the rotator cuff is not typically seen with posterior dislocations, avulsion fractures of the lesser tuberosity may occur. Recurrent instability is rare after these injuries, and ranges from 1% to 4%. Fracture-dislocations of the shoulder are generally more stable after healing compared with simple dislocations. In a simple shoulder dislocation, all of the energy of the injury is used to tear the capsular and ligamentous structures. In a fracture-dislocation, some of the energy is dissipated by the bone (tuberosity fracture), so the ligamentous component of the injury is less, and therefore there are fewer long-term problems with shoulder instability.
D. Treatment and Treatment Rationale
1. Initial management—Initial treatment of an acute glenohumeral dislocation should follow a complete physical and radiographic evaluation, including assessment of the patient’s neurovascular status before and after reduction. Closed reduction should be performed in a relaxed and sedated patient. Intravenous sedation with a narcotic agent and benzodiazepine is routinely used in an emergency department setting before reduction. Inadequate sedation can lead to a traumatic reduction, inciting further injury to an already-compromised joint. Various reduction techniques have been described and include traction-counter traction methods, the modified Stimson maneuver (application of weight to the flexed arm in the prone patient [anterior dislocation]), and digital reduction of the humeral head within the axilla during applied traction on the partially abducted and externally rotated arm (Milch technique). The decision to proceed with surgical or nonsurgical management should include consideration of the patient’s age, activity level, type of injury, number of prior dislocations, chronicity of the injury, and anticipated demands after treatment. Many of these injuries can be effectively treated with nonoperative measures. Patients with traumatic anterior subluxation events may describe a sensation of the shoulder “popping out and then back into place.” MRI studies may not always demonstrate a labrum tear or Hill-Sachs lesion. Initial treatment should include a short period of rest and immobilization followed by a physical therapy rehabilitation program. Patients with recurrent dislocations, dislocations associated with displaced tuberosity or glenoid rim fractures, irreducible dislocations by closed means, chronic dislocations, and young patients with acute primary anterior dislocations can be considered candidates for surgical treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree