I. Overview
A. Divisions of the Femur—The femur may be divided into five general anatomic regions: head and neck, intertochanteric, subtrochanteric, shaft, and supracondylar/intercondylar.
1. Subtrochanteric region—The subtrochanteric zone of the femur is typically defined as the area extending from the lesser trochanter to a point 5 cm distally. Fractures with a component occurring within this region are usually reported as subtrochanteric fractures, even if fracture extensions proximally and distally are observed.
2. Femoral shaft—The shaft of the femur begins at the top of the femoral isthmus and extends to the distal metadiaphyseal junction, an indistinct transitional zone contiguous with the supracondylar region.
B. Incidence and Mechanisms of Injury
1. Subtrochanteric fractures—Subtrochanteric fractures may occur across all age groups. There is an asymmetric age- and gender-related bimodal distribution of fractures. High-energy injuries are typically seen in young males and low-energy injuries are frequently observed in elderly females. Subtrochanteric fracture extensions occur commonly in elderly patients who sustain a hip fracture due to a fall. Typical high-energy mechanisms that predominate in younger patients result from motor vehicle crashes, falls from heights, and penetrating trauma. Although uncommon, fractures can occur in the subtrochanteric region as a complication of screw fixation for a femoral neck fracture, especially if screws are placed below the level of the lesser trochanter, or if an apex proximal triangle configuration of three screws was used.
2. Femoral shaft fractures—Similar to subtrochanteric fractures, femoral shaft fractures are observed in all age groups. However, younger patients with high-energy blunt mechanisms are most common. The majority (70%) occurs in male patients with an average age below 30 years. Transverse and oblique patterns are the most common configurations in young patients. Older patients, especially females, may sustain a femoral shaft fracture due to a lower energy mechanism such as a fall from standing. Spiral patterns are commonly seen in older patients.
C. Anatomy—Subtrochanteric and shaft regions of the femur are encased in a thick muscular envelope. The muscular attachments typically determine the primary displacements following fracture. Subtrochanteric fractures occurring entirely below the lesser trochanter have the typical deformities of flexion, abduction, and external rotation of the proximal segment. Shortening is common in both shaft and subtrochanteric patterns. The osseus anatomy of the proximal femur has considerable variation. The femoral neck is anteverted an average of 13° ± 7° and is translated 1.0 to 1.5 cm anterior to the axis of the femoral shaft. The neck–shaft angle averages 133° ± 7° in women and 129° ± 7° in men. The adult femur has an asymmetrical anterior bow with an average radius of curvature between 109 and 120 cm. The linea aspera is the posterior cortical thickening of the femoral diaphysis, is a muscular attachment site, and buttresses the concavity of the femoral shaft.
II. Evaluation
A. Initial Management—Due to the high-energy mechanisms observed in young patients, associated injuries are common. The initial management includes adequate resuscitation using advanced trauma life support guidelines and should include fluid replacement for blood loss (up to three units of blood loss can be expected per femur fracture). For older patients with low-energy mechanisms of injury, pathologic (including metabolic) etiologies should be investigated.
B. Physical Findings—Typical findings on physical examination include pain, swelling, and deformity. Associated injuries can be distracting. A visual inspection should include a circumferential evaluation of the limb as well as palpation of all extremities, the pelvis, and the spine. The ipsilateral knee and hip should be examined to determine if there are associated noncontiguous fractures or ligamentous injuries. Subtrochanteric fractures tend to shorten and present with fracture extension (the iliopsoas causes flexion of the proximal fragment) and varus (the hip muscles cause abduction and external rotation of the proximal fragment). Shaft fractures present with limb shortening and variable rotation and translation.
C. Emergency Treatment—Emergency treatment should include realignment of the injured extremity using skeletal traction (preferable at the distal femur using a small diameter tensioned wire) to prevent additional soft-tissue injury, to decrease muscle spasm, to limit ongoing blood loss, and to decrease pain. Open wounds should be irrigated and a sterile dressing should be applied. Pulses should be symmetrical, and the ankle–arm index (AAI) should be equal in both extremities. An AAI of less than 0.9 is an indication for vascular consultation and arterial imaging.
D. Radiographic Imaging—Imaging should allow visualization of the entire femoral shaft, the ipsilateral hip, and the ipsilateral knee joint in both the anteroposterior and lateral planes. The femoral neck should be scrutinized for fracture in both subtrochanteric and femoral shaft fractures. This can be accomplished with dedicated hip radiographs, after review of a pelvic CT or both if applicable. The fracture configuration and location, as well as the femoral anatomy can be determined primarily from biplanar radiographs. Bone loss, bone quality, and the femoral canal diameter can be determined. Contralateral femur radiographs can be useful in segmental or highly comminuted patterns, in anticipation of difficulty with length and rotational determination at the time of treatment.
III. Injury Classifications
A. Subtrochanteric Fractures—There are numerous classifications for fractures of the subtrochanteric region.
1. Russell-Taylor classification—The Russell-Taylor classification (Fig. 6-1) has gained acceptance because it is a useful guide in selecting the best type of internal fixation from both a biomechanical and a biological perspective.
2. Orthopaedic Trauma Association (OTA) classification based on the AO/ASIF
• Types 32-A1.1, 32-A2.1, and 32-A3.1 are elementary patterns without comminution (spiral, oblique, and transverse).
• Types 32-B1.1, 32-B2.1, and 32-B3.1 have butterfly comminution (spiral wedge, bending wedge, fragmented wedge).
• Types 32-C1.1, 32-C2.1, and 32-C3.1 are comminuted versions of the elementary patterns.
3. Fielding and Magliato classification
• Type I fractures occur at the level of the lesser trochanter.
• Type II fractures occur within 1 inch below the lesser trochanter.
• Type III fractures occur 1 to 2 inches below the lesser trochanter.
4. Older classifications—Older classifications include those of Seinsheimer, Waddell, and Boyd and Griffin.
B. Femoral Shaft Fractures—Femoral shaft fractures are initially described according to location, pattern (e.g., transverse, oblique, spiral), and any associated soft-tissue injury. The location is typically described as proximal third, middle third, or distal third; or at the junctions of these approximate locations. Additionally, the location of the fracture relative to the isthmus is important for communication.
1. OTA classification—The OTA (AO/ASIF) classification (Fig. 6-2) describes fractures based on morphology and suggests the mechanism of the applied force. Type A fractures are simple in configuration and are divided into spiral, oblique, and transverse patterns. Type B fractures have components of comminution and include spiral and bending wedge patterns; as well as fragmented wedge patterns. Type C fractures have segmental comminution.
2. Winquist-Hansen classification—The Winquist-Hansen classification was devised to describe comminution as related to the need for interlocking screw fixation in early nail designs (Fig. 6-3). Grade 0 and I fractures were considered axially stable and interlocking was therefore not necessarily needed. Grade III, IV, and V fractures were considered axially unstable and therefore required interlocking to prevent shortening and rotational malunion. However, because of the possibility of unrecognized comminution and the currently predictable performance of statically locked nails, this classification system is now largely used for the purpose of describing communication.
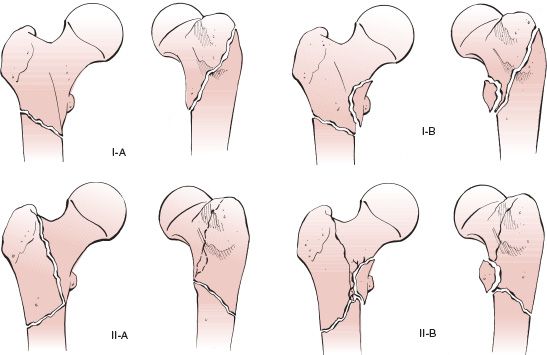
FIGURE 6-1 Russell-Taylor classification of subtrochanteric fractures. Type 1A, Fracture extension with any degree of comminution from below the level of the lesser treochanter to the isthmus with no extension into the piriformis fossa. Type 1B, Fracture extension involving the lesser trochanter to the isthmus with no extension into the piriformis fossa. Type IIA, Fracture extension into the piriformis fossa without lesser trochanter involvement (with medial cortex stability). Type IIB, Fracture extension into the piriformis fossa and involving the lesser trochanter (without medial cortex stability). (Reprinted with permission from Haidukewych G, Langford J. Subtrochanteric fractures. In: Bucholz RW, Heckman JD, Court-Brown C, et al, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
C. Open Fractures—The soft-tissue injuries associated with open fractures are extrapolated from the original system of Gustilo and colleagues. Although not a perfect translation to the femur, it is still used.
1. Type I is an open fracture with a clean wound shorter than 1 cm.
2. Type II is an open fracture with a wound longer than 1 cm and without extensive soft-tissue damage, flaps, or avulsions.
3. Type IIIA open fractures have adequate soft-tissue coverage of the bone despite extensive soft-tissue laceration or flaps; these include open fractures with segmental comminution and fractures caused by a gunshot.
4. Type IIIB signifies periosteal stripping with inadequate soft-tissue coverage of the fractured bone.
5. Type IIIC is an open fracture associated with an arterial injury requiring repair.
IV. Associated Injuries
A. Open Fractures—Open fractures may occur from indirect trauma (e.g., motor vehicle crashes) or from penetrating trauma (e.g., gunshot injuries). These injuries are typically the result of high-energy mechanisms and associated vascular injuries are commonly observed. Intramedullary stabilization remains the treatment of choice for most open fractures. Exceptions include gross contamination that cannot be adequately debrided and substantial surgical delay to treatment. In these cases, a period of skeletal traction with repeated debridements until soft-tissue contamination is reduced is recommended prior to definitive intramedullary stabilization. Low-velocity gunshot injuries do not require an open debridement before intramedullary nailing assuming that no foreign material has been brought into the wound with the projectile. Brumback had no infections in 62 Gustilo Type I, II, and IIIA open fractures and only three infections in 27 Type IIIB injuries (two had delayed treatment). Grosse reported three infections in 115 open femoral shaft fractures, all of which were treated with early IM nailing.
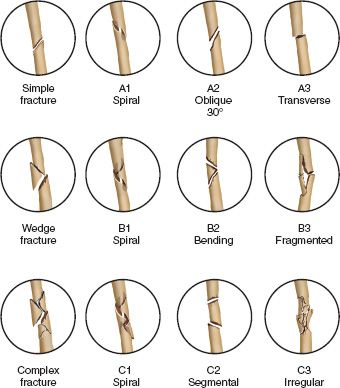
FIGURE 6-2 OTA (AO-ASIF) classification of femoral diaphyseal fractures. Type A fractures have simple patterns: A1, spiral; A2, oblique; and A3, transverse. Type B fractures have wedge patterns: B1, spiral wedge; B2, bending wedge; and B3, fragmented wedge. Type C fractures have complex patterns: C1, spiral comminution; C2, segmental comminution; and C3, irregular comminution.
B. Ipsilateral Femoral Shaft and Neck Injuries—Concomitant femoral neck fractures occur in 3% to 10% of patients with femoral shaft fractures. The femoral neck fracture is often nondisplaced and is missed in 30% to 50% of cases. Most commonly, the femoral neck fracture is basicervical in location (55%), although vertically oriented intracapsular patterns are seen in approximately 35% of patients. Because of the high incidence of missed femoral neck fractures, all patients should undergo a careful review of all available radiographic studies and dedicated hip radiographs. Treatment should be prioritized based on the patient’s overall condition. An accurate reduction and treatment of the femoral neck should take precedence.
C. Floating Knee Injuries—Floating knee injuries (ipsilateral femoral and tibial fractures) are best treated with early stabilization of both injuries, ideally with intramedullary nailing. The femur should be stabilized first. In the event that the patient becomes medically unstable during surgery and both surgeries cannot be completed, femoral fixation allows the patient to sit upright (decreasing the risk of pulmonary complications) and controls pain. The presence of a tibia fracture should not affect the method or direction (antegrade versus retrograde) of medullary stabilization.
D. Fat Embolism—Fat embolism occurs in many trauma patients with long bone fractures, but is usually subclinical. In young patients, a delay in medullary stabilization is associated with an increased incidence of clinically significant fat embolism syndrome.
E. Knee Ligamentous and Meniscal Injuries—Ipsilateral knee ligamentous and meniscal injuries occur commonly in association with femoral shaft fractures. Ligamentous laxity on physical examination is seen in approximately 50% of patients and meniscal tears occur in approximately 30% of patients. Ligamentous stability is best assessed under anesthesia immediately after fracture stabilization.
F. Nerve Injuries—Nerve injuries occur rarely and are more likely following penetrating trauma.
G. Vascular Injuries—Associated vascular injuries are rare, but they represent a surgical emergency. Vascular flow to the extremity should be reestablished within 6 hours if possible to maximize limb salvage rates. Temporary shunting followed by orthopaedic stabilization and definitive vascular repair may be necessary if a time delay exists. In most instances, definitive femoral stabilization can be performed during the same surgical procedure as the vascular repair.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






