A. Anatomy and Biomechanics (Figs. 13-1 to 13-3)—The normal ankle is a three-bone articulation stabilized on both sides by ligamentous structures. The tibia joins the fibula and houses the talus in a mortise configuration held fast by four syndesmotic ligaments and the interosseous membrane. The medial malleolus yields the deltoid ligament, which is divided into two layers: the superficial layer, and the shorter, stouter, stronger, deep layer. The fibula gives rise to the three components of the lateral collateral ligamentous complex: the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL) (the strongest lateral ankle ligament), and the posterior talofibular ligament (PTFL). The talus is wider anteriorly and causes widening and deepening of the mortise in dorsiflexion to enhance stability of the joint. Motion is predominantly sagittal but not purely hinged because dorsiflexion also yields slight external rotation, whereas plantar flexion also causes internal rotation of the talus with respect to the tibia. The articulation between the tibial roof (plafond) and the talar dome is not flat, but demonstrates a shallow bicondylar appearance dorsally with corresponding indentations on the plafond. This configuration is rather stable, but subtle shifts in the articulation lead to extreme decreases in contact area and corresponding increases in contact stress. A 1 mm talar shift can reduce the contact surface 42%. This effect can be quite extraordinary because the normal joint reaction force in a one-legged stance can be as high as four times the body weight, with only 6% to 16% of this being borne on the fibula and the remainder absorbed through the tibiotalar articulation.
B. Fracture Types—Ankle fractures can be subdivided into several categories: those that involve the malleolar projections and those involving the tibial plafond.
1. Malleolar fractures—Malleolar fractures can include bimalleolar, trimalleolar, or isolated medial or lateral malleolar fractures.
• Examination—There is a history of a twisting injury or a low-energy fall, local swelling, ecchymosis, occasional deformity, or rare neurovascular compromise (the risk increases with higher-energy injuries).
• Classification—The fractures are classified based on radiographic findings. Two popular systems exist. The Danis-Weber (AO/ASIF) classification is based on the level of the fibular fracture. The Lauge-Hansen classification (older and more complex) is based on the position of the foot at the time of the injury, combined with the applied deforming forces; it describes the initial point of injury and the path it will take. Both classifications are commonly used, but neither is universally accepted, although they overlap somewhat. A Weber A type fracture corresponds to a Lauge-Hansen supination-adduction injury, whereas a Weber B is the equivalent of a Lauge-Hansen supination-external rotation or a pronation-abduction injury. A Weber C type fracture corresponds to a Lauge-Hansen pronation-external rotation type injury (Fig. 13-4).
• Treatment—Treatment is based on the amount of distortion of the anatomic structures and articular incongruity. Goals include the restoration of proper anatomy, articular congruity, and biomechanical function.
(a) Isolated lateral malleolar fractures—In the absence of a medial injury, isolated lateral malleolar fractures do not alter tibiotalar mechanics and therefore can be treated with protected weightbearing in a walking cast or brace as soon as symptoms allow. Ligamentous structures and medial stability prevent displacement of the fracture and more important, lateral shift of the mortise. Care must be taken to rule out the possibility of a medial ligamentous or syndesmotic injury (Fig. 13-5).
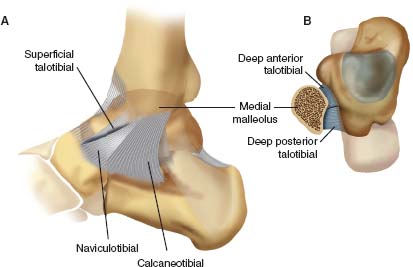
FIGURE 13-1 The medial collateral (deltoid) ligament of the ankle includes both superficial and deep components. A. The superficial components include the superficial talotibial, naviculotibial, and calcaneotibial components. B. The deep deltoid ligament fibers run transversely from the posterior colliculus of the tibia to the talus.

FIGURE 13-2 The lateral ankle ligaments include the anterior talofibular (the most important stabilizer and the most commonly injured), the calcaneofibular, and the posterior talofibular.
(b) Isolated medial malleolar fractures—Isolated medial malleolar fractures have a relatively high risk of nonunion (5% to 15%) with over 2 mm of displacement. Therefore all but nondisplaced fractures should be treated with open reduction with internal fixation (ORIF). Vertically oriented fracture lines are more unstable and are associated with stress fractures. (Strong considerations should be given to operative management of vertically oriented fractures as they tend to be stress fractures and may fall into varus with casting. Two cancellous screws or one screw and a K-wire are required to control rotation in addition to applying a compressive force across the fracture site.
(c) Bimalleolar fractures and equivalents—Bimalleolar fractures and equivalents create loss of both medial and lateral support (with a fractured distal fibula and either a fracture of the medial malleolus or a deltoid ligament rupture). These are unstable fractures, and therefore there is poor control of reduction with nonoperative treatment. ORIF of both fragments is the treatment of choice. Bimalleolar equivalents are Weber B fracture patterns (aka SER- IV equivalents) with an associated deltoid ligament injury. Clues to a bimalleolar equivalent are medial hindfoot ecchymosis, medial ankle tenderness, bone flecks off the distal tip of the medial malleolus, and a widened medial clear space. Stress views should be performed to evaluate opening of the medial clear space and a medial clear space greater than 4 mm is an indication for surgery. Magnetic resonance imaging (MRI) may be helpful to evaluate the deltoid if stress views are unclear. It is unnecessary to repair the deltoid ligament in a bimalleolar equivalent; anatomic reduction of the fibular yields restoration of the mortise in about 90% of cases. In the remaining 10% of cases a medial arthrotomy is required for extraction of an incarcerated deltoid ligament. Occasionally, the tibialis posterior tendon is interposed between the medial fragments; this is sometimes suggested radiographically by a posteromedial flake of bone on the injury films. Nonoperative care is acceptable when there is no injury to the deltoid ligament and no talar shift (one can accept up to 2 mm of fibular displacement). A high fibular fracture suggests a syndesmotic ligament injury. These are stable after repair of both malleoli. However, with a bimalleolar equivalent, syndesmotic fixation should be incorporated when the fibular fracture is more than 4.5 cm from the joint line and when the deltoid ligament is not repaired. Recent studies have shown that fracture pattern does not reliably predict a syndesmotic injury. Intraoperative stress testing should be performed after definitive fixation of ankle fractures. Intraoperative radiographs at the time of surgery help assess medial stability after fibular fixation to determine the need for syndesmotic screw fixation, but the most reliable indication is attempting manual displacement of the fibula from the tibia while under direct visualization. Careful attention should be paid to proper replacement of the fibula in the tibial groove posterior to the mid-line to avoid malreduction while applying syndesmotic fixation. Contralateral ankle films and possible open repair of the syndesmosis may be necessary. Because of the shape of the talus, the ankle should be maximally dorsiflexed before placement of a syndesmotic screw; failure to do this results in limited ankle dorsiflexion. Syndesmotic screws have been shown to alter the mechanics of the distal tibiofibular joint (especially external rotation), so they should be removed but no sooner than 8 to 12 weeks to allow for ligamentous healing. Weightbearing may begin after 6 weeks if the screw has captured three cortices.
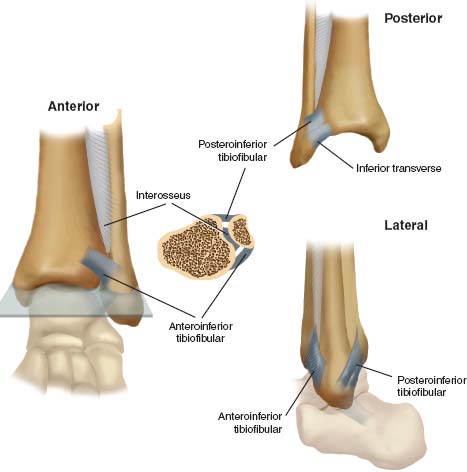
FIGURE 13-3 The syndesmotic ligaments include the anteroinferior tibiofibular ligament (AITFL), the posteroinferior tibiofibular ligament (PITFL), the inferior transverse ligament (ITL), and the interosseous ligament (IOL).
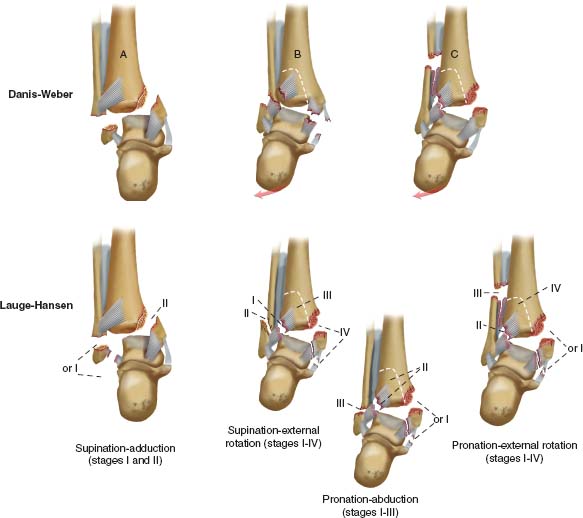
FIGURE 13-4 Danis-Weber (AO/ASIF) and Lauge-Hansen classifications of ankle fractures.
(d) Trimalleolar fractures—Trimalleolar fractures represent a bimalleolar fracture combined with a bony injury to the posterior tibial plafond (posterior malleolus). ORIF is necessary because these injuries are unstable. The principles are the same as those for bimalleolar fractures. The posterior fragment frequently maintains its attachment to the fibula by the posteroinferior tibiofibular ligament (PITFL) and therefore reduces once the lateral malleolus is repaired. The posterior malleolar fragment should be fixed if over 25% of the posterior distal tibial articular surface is involved on the lateral radiograph and the fragment is still more than 2 mm displaced after reduction of the fibula. Contact stresses at the ankle do not increase until 25% to 40% of the posterior joint surface is removed. Anterior or posterior surgical approaches for ORIF are acceptable.
2. Pilon fractures—Higher-energy injuries involving the tibial plafond are discussed in detail in Chapter 12.
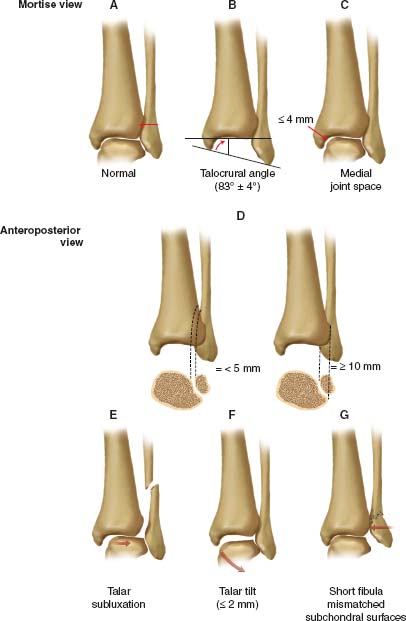
FIGURE 13-5 Restoration of the ankle mortise requires anatomic reduction of the lateral malleolus so that its articular surface is congruous with the reduced talus. A. On a mortise radiograph, the condensed subchondral bone should form a continuous line around the talus, and there should be no proximal displacement, malrotation, or angulation of the lateral malleolus. B and C. A proper talocrural angle and normal joint space width also indicate normality. On the mortise view, the medial joint space should be less than or equal to 4 mm, and the superior joint space should be within 2 mm medially of its width laterally. D. Adequate tibiofibular overlap on the anteroposterior view indicates a proper syndesmotic relationship. The space between the medial wall of the fibula and the incisural surface of the tibia should be less than 5 mm. The anterior tubercle of the tibia should overlap the fibula by at least 10 mm. E and F. Talar malalignment is indicated by the talus’s lateral displacement or tilt into valgus. G. Although the talus may be reduced by external pressure, its alignment is not maintained by a shortened, malrotated lateral malleolus, as shown.
3. Open ankle fractures—Treatment depends on the soft tissue injury. Gustilo Type I, II, and sometimes IIIA open injuries can be treated by the same principles as described for closed injuries as long as thorough and extensive debridement is performed. Closure or coverage is preferable within 5 days. More severe soft-tissue injuries are frequently associated with greater bony destruction as well. These often necessitate a combination of internal and external fixation and multiple debridements with secondary soft tissue coverage such as a muscle pedicle flap. Antibiotics should be given for at least 48 hours after closure.
C. Techniques for Fixation of Ankle Fractures—The technique used for the fixation of ankle fractures depends on the type of fracture sustained. Fixation usually begins with lateral stabilization because, usually, this is simpler and provides enough fixation to hold the mortise reduced. Care should be taken to avoid the superficial peroneal nerve and less commonly the sural nerve. Lag-screw fixation of the fibular fracture is incorporated when possible. Liberal use of intraoperative radiographs is a must to assess reduction.
Fracture dislocations should undergo emergent reduction followed by immediate internal fixation, splinting with very close follow up, or a spanning external fixator. Fractures that remain dislocated or subluxated can lead to skin compromise and/or further cartilaginous injury.
1. Difficult repairs in osteoporotic fibulae—Difficult repairs in osteoporotic fibulae are sometimes better approached with a posteriorly applied antiglide plate. This can obviate the need for screws in the distal fragment by acting as a buttress and preventing proximal migration of the fibula. It appears that a locking plate offers at least the same biomechanical strength as a conventional plate.
2. Severe fibular comminution—Severe fibular comminution may be treated by reducing the distal fragment to the talus with K-wire fixation, applying a plate, and bone grafting the resultant defect. Contralateral ankle films and preoperative templating can prevent malreduction, which is most commonly shortening of the fibula.
3. Seriously ill patients—Seriously ill patients with isolated fibular fractures may be treated with intramedullary rods (e.g., Rush rods). The obvious limitation is the lack of rotational control.
4. Small medial malleolar fragments—Small medial malleolar fragments may be difficult to stabilize with screws, and tension band wiring is a useful alternative.
5. Syndesmotic fixation—Syndesmotic fixation is obtained with a 30° anteriorly directed cortical screw (a positioned screw, not a lag screw). The ankle should be maximally dorsiflexed, and clamped, and a set screw placed. A lag screw should not be placed across the syndesmosis. The optimal position is 2 cm proximal to the joint and 3.5 or 4.5 mm screws may be used in a bicortical or unicortical fashion.
D. Associated Injuries—Any open reduction should be accompanied by direct visualization of the joint because osteochondral lesions are common. Also, plafond extension or lateral ligament disruption should be addressed if encountered.
E. Complications
1. Soft tissue problems—Fracture blisters are managed by delaying treatment until it is reasonable and safe to proceed with surgery. Pneumatic compression is sometimes helpful in reducing edema and decreasing the time to surgery. Clear fracture blisters are relatively safe and may be debrided at the time of surgery. Blood-filled blisters should be avoided for their high risk of necrosis and slough. The risk of slough is also increased as much as 10% to 20% by delaying closed reduction of a dislocated ankle. If fracture blisters are present, or there is difficulty in maintaining the reduction, a temporary external fixator may be placed.
Open fractures with inadequate soft tissues for closure pose a difficult problem. Irrigation and debridement should be performed followed by a VAC prior to definitive soft tissue coverage. VAC therapy continued after soft tissue coverage can further increase the survival of a free flap. Fractures tend to have the lowest rate of infection when definitive soft tissue coverage occurs within 5 to 7 days after injury.
2. Ankle fractures in diabetes—The clinician must rule out a Charcot process; if a Charcot process is present, total contact casting should be considered. If this fails, arthrodesis should be performed. Healing of bone and soft tissue in patients with diabetes takes two to three times as long as healing in patients without diabetes.
3. Malunions—Malunions usually occur through a rotational deformity of the lateral malleolus. (This deformity is frequently subtle and leads to abnormal joint forces.) They are repairable with a fibular derotational osteotomy and sometimes an interpositional bone graft to restore length.
4. Posttraumatic arthritis—The best treatment for painful posttraumatic arthritis is arthrodesis in neutral dorsiflexion, 5° of hind-foot valgus, and rotation equal to that on the unaffected side.
5. Nerve injury
• Lateral malleolus—The direct lateral approach has the highest incidence of injury to the superficial peroneal nerve (SPN). It exits its fascial hiatus about 9 cm above the tip of the lateral malleolus but its location may vary between 4 and 13 cm. The posterolateral approach decreases the risk of injury to the SPN but increases the risk of injury to the sural nerve.
• Medial malleolus—The saphenous nerve is a very consistent structure and runs with the saphenous vein about 1 cm anterior to the medial malleolus. A direct medial approach can minimize injury to the nerve.
6. Return to function—A return to normal automobile braking time following ORIF of an ankle fracture is about 9 weeks.
II. Soft-Tissue Injuries of the Ankle
A. Ankle Sprains—The most common ligamentous injury in the human body is an ankle sprain; it accounts for 15% of all athletic injuries. Some 20% to 40% of all ankle sprains proceed to chronic instability. Peroneal tendon weakness is the number one cause of recurrent ankle sprains in ballet dancers.
1. Anatomy—The ankle is stable when loaded and unstable when unloaded. Ankle ligaments include the deltoid ligament medially (see Fig. 13-1), and the ATFL (which is intracapsular), CFL, and PTFL laterally (see Fig. 13-2). Subtalar ligaments include the lateral talocalcaneal ligament, cervical ligament, interosseous talocalcaneal ligament (between the middle and the posterior calcaneal facets
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






