I. Overview—The elbow provides the critical linkage as the shoulder moves the hand through space. The normal elbow has an average extension to flexion arc of 0° to 145°. Normal pronation and supination are approximately 80° and 85°, respectively. Functional arcs fall within these limits, with activities of daily living requiring 50° each of pronation and supination and a 100° arc of extension to flexion between 30° and 130°. Less than 130° of elbow flexion diminishes the ability to feed and groom oneself. Fractures and dislocations of the elbow should be evident on routine anteroposterior (AP), lateral, and oblique radiographs. The radiocapitellar view provides an additional and clearer view of this joint. Information from these plain radiographs is almost always sufficient for the surgeon to decide between operative and nonoperative treatment. Once a decision is made to pursue operative treatment, plain radiographs with gentle traction applied to the arm after anesthesia may further clarify fracture anatomy, especially in the case of distal humerus fractures. Computed tomography (CT) is indicated to assess the articular surfaces when the decision to pursue operative treatment on the basis of articular displacement is equivocal after plain radiographs. It is also more ideal to assess fragment size and configuration prior to surgery.
II. Distal Humerus Fractures (Fig. 21-1)
A. Anatomy—The distal humerus consists of an obliquely oriented articular surface comprised of the spool-like trochlea and the hemispheric capitellum, each supported by a condylar column. The olecranon fossa lies between these columns proximal to the articular surface. Its sometimes paper-thin floor is the confluence between the anterior and posterior cortices of the distal humerus and contributes little osseous support. The longitudinal axis of the spool-shaped trochlea is internally rotated 3° to 8° with respect to the humerus and inclines laterally 5° to 8°, thereby creating the valgus carrying angle of the extended elbow. In the male, the mean carrying angle is 11° to 14°, and in the female, it is 13° to 16°. The roughly hemispheric capitellum is centered 1 to 1.5 cm anterior to the central axis of the humeral shaft. The humerocapitellar angle in the adult is 30°. The medial column diverges at an angle of 45° with the humeral shaft, whereas the lateral column diverges 20° to 25°. The medial epicondyle, forming the distal extent of the medial column, lies just posterior to the rotational axis of the trochlea. Thus a cam effect is created, with different portions of the medial collateral ligament (MCL) becoming taut at different angles of flexion. Conceptualizing distal humerus fractures as involving one or both columns simplifies accurate identification and management. Isolated capitellar fractures are discussed separately.
B. One-Column Fractures—These fractures involve part or all of the trochlea. Milch and Jupiter have classified these, depending on how much of the trochlea remains with the involved column. High-columnar fractures involve the majority of the trochlea, and the radius and ulna are displaced with the fractured column. Low-columnar fractures involve a smaller portion of the trochlea, and the radius and ulna remain with the intact humeral column and shaft. For fractures displaced more than 2 mm, anatomic reduction with stable internal fixation allows for early motion and yields consistently better results than closed management. For nondisplaced fractures, the position of immobilization should relax the musculature originating from that column (i.e., pronation for medial column fractures, supination for lateral column fractures). Rigid fixation of high columnar fractures with plates provides improved rigidity over screws alone; low columnar fractures without comminution may be adequately stabilized with screws. In either case, the articular reduction must be anatomic. This can be achieved through indirect reduction at times, but may require an olecranon osteotomy in certain cases. For lateral column fractures where the lateral trochlea is fractured off with the capitellum, a chevron olecranon osteotomy can be levered open on a medial (ulnar) soft-tissue hinge. This provides for adequate articular visualization and anatomic restoration while leaving the medial structures (i.e., the ulnar nerve and MCL) undisturbed. This also simplifies reduction and fixation of the osteotomy.
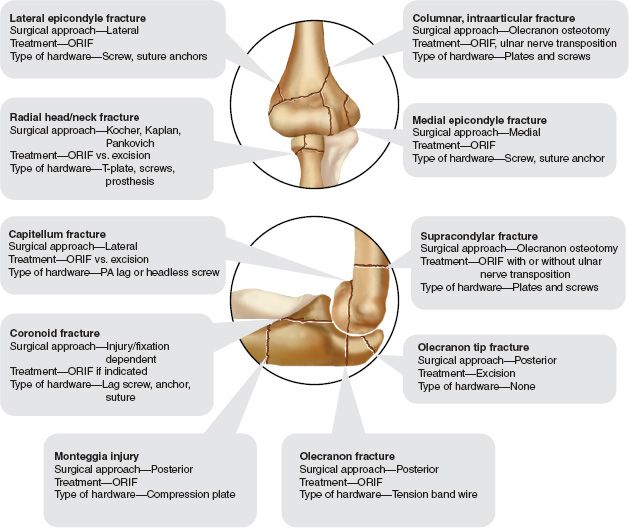
FIGURE 21-1 Treatment of elbow fractures. Although there may be alternative treatments of equal merit, this is the standard information at this time. ORIF, Open reduction with internal fixation; PA, Posteroanterior.
C. Two-Column Fractures—Fractures involving both columns are either intra-articular or extra-articular. While common in children, extra-articular columnar fractures (i.e., supracondylar fractures) are rare in adults (except perhaps in osteoporotic older individuals). Fixation in the presence of closed physes is similar to that used in intraarticular fractures. In adults, efforts must be made to achieve anatomic reductions and rigid internal fixation, despite the allure of percutaneous pin fixation. Shear forces are too great, and postoperative fracture displacement occurs too often with limited fixation. Intra-articular bicolumnar fractures frequently result from high-energy trauma and may be extensively comminuted. Common fracture patterns include the T, Y, H, and the laterally or medially inclined “lambda” fractures. The high risk for stiffness and loss of motion after such fractures is best minimized by stable fixation and early motion. If sufficient stability to permit early range of motion (ROM) cannot be achieved, then anatomic restoration of the articular surface should take precedence. Joint contractures in the presence of healed, congruent articular surfaces can be effectively treated with a soft-tissue release. Two-column distal humerus fractures are best approached posteriorly. Given the relatively high incidence of ulnar neuropathy associated with these injuries (early and late), some recommend anterior transposition of the ulnar nerve at the time of fracture fixation. This can be easily performed from the posterior approach.
An olecranon osteotomy, most reliably and inexpensively stabilized with a tension band wiring technique, affords access to the entire articular surface. The osteotomy should be an apex distal osteotomy centered over the bare articular area of the trochlear notch. Larger fragments, whether columnar or intraarticular, should be stabilized first. The columns are most rigidly fixed with plates along their posterior aspects. Dual plating along the columns is stronger than Y plating or other constructs. The lateral column, with its gently curved posterior aspect, usually accommodates 3.5-mm dynamic compression plates (stronger torsional forces and bending moments). The more malleable 3.5-mm reconstruction plates are better for more distal fractures requiring plate bends with smaller radii of curvature. The use of two plates along the lateral column (one posterior, one lateral) has also been described. The contour of the medial epicondyle usually requires a reconstruction plate posteriorly or a one-third tubular plate along its medial ridge. Alternatively, “prebent” plates are available and can be used in a similar fashion. The trochlea, which is usually fractured in the sagittal plane, is best stabilized with screws along its axis; these may be passed through the various plates for added stability. Since the articular cartilage of the trochlea covers 270° of its surface, fixation of articular fragments is best accomplished with headless compression screws or lag screws countersunk below the subchondral bone. Provisional pin fixation and patience, with accurate contouring of plates, greatly facilitate stable fixation. Even prebent plates often require some additional bending to conform to each patient’s unique anatomy.
Total elbow arthroplasty (TEA) has been used to treat primarily elderly, low-demand osteoporotic patients with comminuted bicolumnar fractures not amenable to open reduction and internal fixation. Such elbow fractures in patients with pre-existing degenerative conditions of the elbow, such as rheumatoid arthritis, are also candidates for primary TEA. It is important not to perform an olecranon osteotomy if TEA is necessary, as this can result in inadequate fixation of the ulnar prosthesis. In higher-demand elbows, however, the surgeon should strive for optimal fracture fixation and bone healing (even if a later contracture release becomes necessary). Postoperative care should include active motion as soon as it is appropriate, depending on the fixation achieved (immediately if at all possible).
III. Capitellum Fractures (Fig. 21-1)—Fractures of the capitellum are rare. The usual configuration is a shear fracture in the coronal plane with superior displacement of the articular surface. Bryan and Morrey have classified these as Type I, complete fractures; Type II, osteochondral fractures; and Type III, comminuted fractures (Table 21-1). Type I fractures consist of the hemisphere of the articular surface and the underlying cancellous bone (typically referred to as the Hahn-Steinthal fracture). Occasionally, Type I fractures may be amenable to closed reduction if attempted early. However, it is difficult to achieve and subsequently maintain adequate reduction. When required and possible, internal fixation is best accomplished with lag screws from posterior to anterior into the posterior portion of the lateral condyle. A lateral approach with subperiosteal release of the common extensor origin is used to expose the capitellum and posterior aspect of the distal lateral column. Type II fractures are less common and consist of an osteochondral shell of the anterior capitellar cartilage (i.e., the Kocher-Lorenz fracture). Occasionally, these fractures are amenable to fixation with headless anterior-to-posterior compression screws if there is enough cancellous subchondral bone for stable fixation. Highly comminuted (Type III) and osteochondral fractures may not be amenable to stable internal fixation. Excision of fragments is then recommended as long as the integrity of the radioulnar interosseous ligament and MCL has been confirmed. In the presence of longitudinal radioulnar instability, excision of the capitellum is analgous to excision of a nonrepairable radial head. In either case, proximal radial migration leads to positive ulnar variance and ulnocarpal impaction. Although avascular necrosis (AVN) of the fragment is rare, delayed excision of a necrotic fragment is appropriate. Excision of capitellar fragments, whether performed initially or delayed, may lead to elbow stiffness. Arthroscopic excision results in improved motion compared with open excision.
IV. Elbow Dislocation (Fig. 21-2)
A. Anatomy—Dislocation of the elbow joint in the adult population has an annual incidence of 13 per 100,000 people. That is about the same incidence as proximal interphalangeal joint dislocations, but less than shoulder dislocations at 17 per 100,000. The osseous anatomy of the elbow is inherently stable and contributes the majority of resistance to varus and valgus forces. The column model (Greek temple) of elbow stability depicts the humerus as spanning the articular surfaces of the radial head and the coronoid process of the ulna. Valgus forces are resisted primarily at the radiocapitellar joint (the lateral column), whereas varus forces are resisted primarily at the ulnohumeral joint (the medial column). The ulnohumeral articulation provides 55% of the resistance to varus with the elbow extended and 75% of the resistence with the elbow flexed 90°. The radiocapitellar joint, though transmitting up to 60% of the axial force from the hand to the humerus, contributes only 30% of the resistance to valgus force at the elbow. In cases of ligament disruption, the osseous columns contribute more of the resistance to varus and valgus loads. The anterior band of the MCL originates from the anterior portion of the medial epicondyle (the center of the ulnohumeral motion axis) and inserts onto the medial base of the coronoid. The lateral, or radial, collateral ligament (LCL) originates from the lateral epicondyle of the humerus at the axis of ulnohumeral motion and inserts into the annular ligament and into the proximal ulna just lateral to the lesser sigmoid notch (Fig. 21-3). Classically, the anterior band of the MCL is considered the primary stabilizer of the ulnohumeral joint, but the role of the LCL, especially the ulnar portion, has been clearly delineated. The MCL contributes 70% of the resistance to valgus loads in the intact elbow. The anterior capsule also provides some resistance to both valgus and varus stress, primarily with the elbow in extension. Clinically, the MCL may provide adequate stability against valgus force even in the case of radial head resection. Biomechanical studies of the LCL, however, suggest that stability to varus force depends on both an intact LCL and a competent coronoid process (>50% intact). The lateral ulnar collateral ligament (LUCL) cradles the radial head and prevents its posterior subluxation along with preventing lateral opening of the ulnohumeral joint. Such instability is termed posterolateral rotatory instability (PLRI). Injuries to the LCL complex have been created biomechanically with application of a supination, hyperextension load. Testing of elbow stability with the forearm in pronation to tighten the LCL has been suggested; testing in supination may lead to confusion between PLRI and MCL laxity if a “clunk” is felt during valgus testing. The collateral ligaments usually fail in their midsubstance, although avulsion fractures, especially laterally, may occur, usually in adults. An attenuated MCL has been associated with valgus instability but not with recurrent dislocation, whereas an incompetent LUCL has been associated with subluxation and recurrent dislocation. An incompetent LUCL leading to PLRI can frequently be detected by the pivot shift test. A supination valgus moment is applied to the flexed elbow with the patient supine. The subluxation is felt as the elbow is extended and a reduction clunk is felt as the elbow is flexed again. The flexor-pronator group and the extensor group of muscles serve as secondary dynamic stabilizers of the elbow joint, as do the triceps, brachialis, and biceps muscles. These muscles span the elbow joint, resisting applied moments, and increasing joint reactive forces (thereby increasing the osseous stability). Grossly unstable elbow dislocations are often associated with rupture of these dynamic stabilizers as well as the static ligamentous restraints.

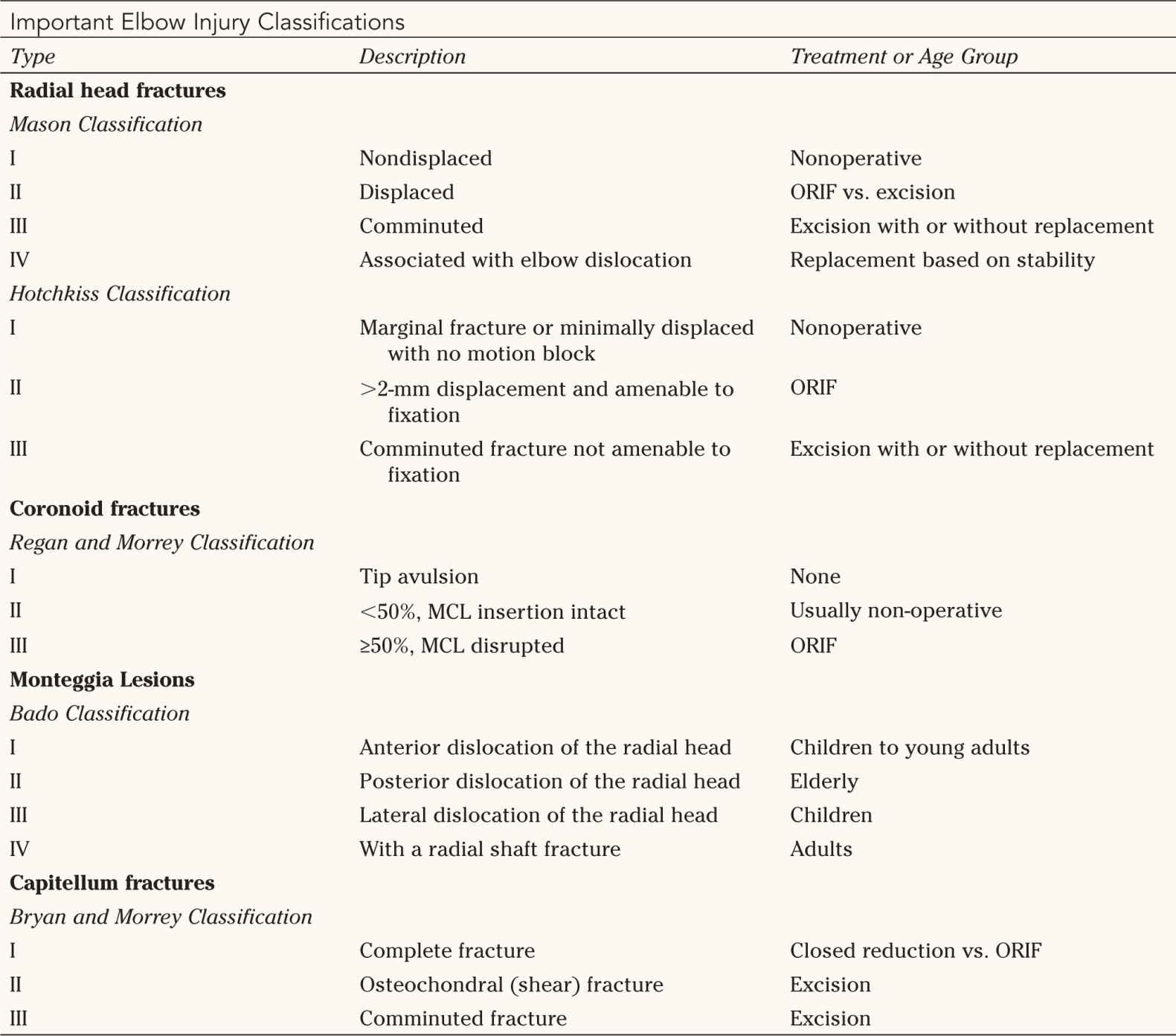
ORIF, Open reduction with internal fixation.

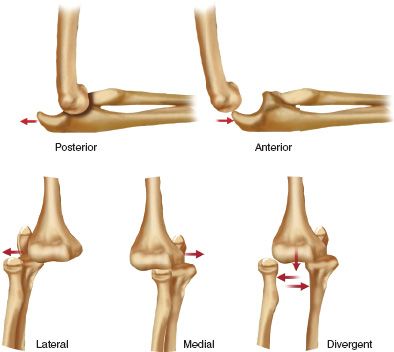
FIGURE 21-2 Elbow dislocations. Note that the classification is based on the direction of displacement of the forearm bones.
B. Evaluation and Treatment—Despite the inherently stable osseous configuration of the joint, dislocations of the elbow represent 20% of all dislocations. The injury occurs most often in young people as a result of relatively high-energy trauma but can nevertheless occur after a seemingly minor fall onto an outstretched hand. Some 90% of elbow dislocations are posterior. Anterior, medial, or lateral dislocations are rare; divergent dislocations (radius and ulna displaced in different directions with disruption of the proximal radioulnar joint) are extremely rare. As the ulnohumeral joint dislocates, the radial head and coronoid are sometimes fractured (in up to 10% and 18%, respectively, of all elbow dislocations); more rarely the olecranon tip is fractured. At surgical exploration, over 90% of elbow dislocations demonstrate osteochondral fractures that may be attributed to the initial trauma or to subsequent overzealous reduction maneuvers. The humeral epicondyles may fracture as well, representing avulsion of the collateral ligaments. These fragments, along with injured soft tissue, can become incarcerated within the joint, necessitating operative intervention. True lateral and AP X-rays are required to confirm a congruent reduction. A CT scan is also informative as to the exact location of the fragment and more subtle impaction and shear fractures, especially those involving the medial coronoid. An incongruent reduction is an indication for surgical exploration with open reduction.
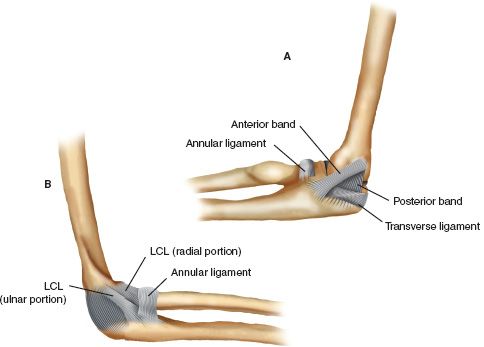
FIGURE 21-3 Elbow joint. A. Medial collateral ligament with its important anterior band. B. Lateral collateral ligament (LCL).
1. Reduction—Reduction under appropriate sedation that provides sufficient muscle relaxation should be followed by an examination of joint stability and ROM. This allows the examiner to gauge the extent of injury to various stabilizers as well as the limits of motion appropriate for early rehabilitation. Blocked motion usually indicates an incarcerated osteochondral fragment. Stability to varus and valgus stress should be tested in 30° of flexion and full pronation. The simple elbow dislocation stable beyond 45° of flexion should generally be splinted in 90° of flexion and neutral pronation/supination. Pronation tightens the LCL and may be used to improve postreduction stability. However, certain patients, especially younger athletes, may enjoy a more rapid recovery of function if open repair of critical ligaments and muscle tendon units is performed acutely.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






