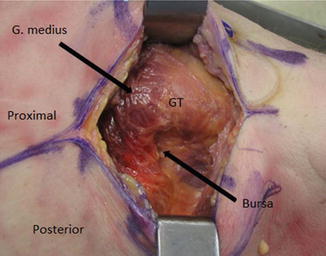
Fig. 1
The vascular supply to the femoral head
There is no true internervous, intervascular, or intramuscular plane in the posterolateral approach. The gluteus maximus, which is split in line with its fibers is not significantly denervated by the approach, because it receives its nerve supply (from the inferior gluteal nerve), proximal to the split. Care should be taken therefore to avoid aggressive proximal dissection of the gluteus maximus. The vascular supply to the gluteus maximus (from the superior and inferior gluteal arteries) is redundant, and vascular compromise is therefore uncommon. Branches of the inferior gluteal artery (which supply the distal two third of the muscle) are invariably cut when splitting the gluteus maximus, so care should be taken to identify and coagulate them before they are avulsed.
The sciatic nerve is the major nerve at risk in the posterolateral approach. The sciatic nerve is rarely exposed during this approach, but knowledge of its location is crucial. Injury to the sciatic nerve is generally due to compression from retractors or excessive stretching (such as with lengthening of the limb); direct transection is rare. When viewing the field from the surgeon’s perspective, the sciatic nerve (or its tibial and peroneal branches) enters the field deep to the piriformis muscle belly. It then continues its course (viewed from the surgeon) superficial to the remainder of the short external rotators (the superior gemellus, obturator internus, inferior gemellus, and the quadratus femoris) and then runs deep to the tendinous insertion of the gluteus maximus (Fig. 2). The femoral nerve is also at risk of indirect injury, usually from anterior acetabular retractor placement. In placing the anterior retractor, care must be taken to hug the bony anterior wall and avoid impinging soft tissue between the retractor and the anterior walls of the acetabulum.
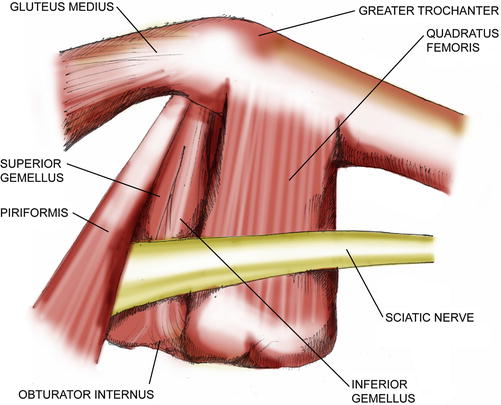
Fig. 2
The course of the sciatic nerve as viewed from the surgeon’s perspective
Surgical Technique
Positioning
The patient is positioned in the lateral decubitus position. Care must be taken to ensure that the pelvis is level and secure, particularly in the setting of total hip arthroplasty , as a tilted or rotated pelvis may lead to improper positioning of the acetabular component. The pelvis is secured using well-padded hip positioners on the sacrum posteriorly and the pubis and/or iliac crests anteriorly. Alternatively, a bean bag may be used. Using the floor as an external reference, care is taken to ensure that the gluteal crease is parallel to the floor. As an additional check, the anterior superior iliac spines may be palpated and interspinous line should be perpendicular to the floor. An axillary roll is placed just distal to the axilla on the proximal chest wall to minimize neurovascular compromise on the dependent upper extremity. The dependent leg is well padded to minimize pressure injury to this extremity or compression of the superficial peroneal nerve (Fig. 3).


Fig. 3
Patient positioning for the posterolateral approach. The contact points of the hip positioner are well padded and an axillary roll has been placed (not shown). Care is taken to ensure that the pelvis is secure and perpendicular to the ground
Superficial Exposure
Proper placement of the skin incision facilitates exposure of the deeper structures, enables the use of more limited incision sizes, and avoids the need for aggressive soft tissue retraction. Begin by palpating and outlining the greater trochanter. Palpation of the trochanter can be facilitated by abduction and adduction of the hip by an assistant. This is particularly helpful in obese patients. In very large patients, a 22-guage spinal needle can be helpful in sounding the proximal femur and identifying the borders of the greater trochanter. A longitudinal incision (ranging from 7 to 20 cm) is made over the posterior one third of the greater trochanter. Too anterior an incision makes retraction of the posterior flap difficult, particularly in the setting of an obese or muscular patient. Too posterior an incision puts the sciatic nerve at risk. Proximally, the incision may be directed toward the posterior superior iliac spine, and distally it is directed in line with the femoral shaft. A good rule of thumb for total hip arthroplasty is that one third of the incision should be proximal to the proximal tip of the greater trochanter and two third should be distal. The skin incision is performed sharply and care is taken to cauterize subcuticular vessels (Fig. 4).
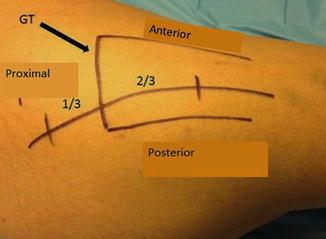
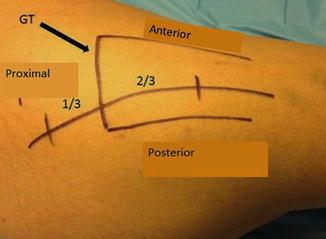
Fig. 4
The incision is centered at the posterior one third of the trochanter. Two-thirds of the incision is distal to the tip of the trochanter (GT greater trochanter)
Next, the subcutaneous tissues are dissected using a knife or electrocautery. Care should be taken to identify and cauterize subcutaneous vessels. When performing the subcutaneous dissection, the surgeon should pause frequently to palpate the greater trochanter, which becomes more easily palpable with increasing dissection. The goal is to create one subcutaneous plane that is directed toward the midline of the greater trochanter in the anteroposterior plane. Once the fascia lata is identified, a Cobb elevator may be used to gently clear the remaining subcutaneous tissues in order to expose the fascia and to facilitate closure of full thickness fascial flaps at the conclusion of the case (Fig. 5).
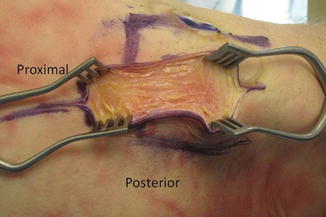
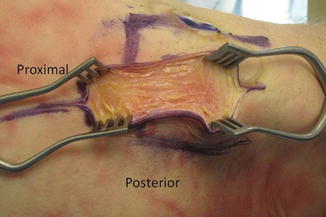
Fig. 5
Subcutaneous dissection is carried out with electrocautery. Care is taken to aim the plane of dissection toward the midline of the greater trochanter in the anteroposterior plane
Next the fascia is incised in line with the incision. Starting at the distal aspect of the incision approximately 3 cm of fascia is incised from distal to proximal (Fig. 6). Next the surgeon uses the index finger to sweep 360° underneath the fascial incision in order to break up bursal adhesions. Manually releasing these adhesions facilitates the creation of full thickness anterior and posterior fascial and gluteal flaps. Next the fascial incision is carried proximally. The gluteus maximus is split in line with its fibers, and electrocautery is used to coagulate branches of the inferior gluteal artery which are invariably cut. Approximately 5 cm of gluteus maximus splitting is generally adequate to provide excellent exposure of both the femur and acetabulum . Further proximal dissection of the gluteus maximus risks injury to the inferior gluteal nerve and denervation of the muscle. A Charnley retractor is then placed, first on the posterior flap (where the sciatic nerve is at risk if the retractor is placed to deeply) and then the anterior flap (Fig. 7).
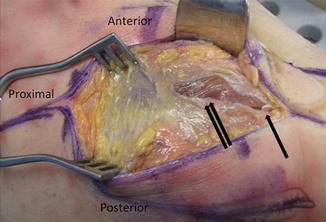
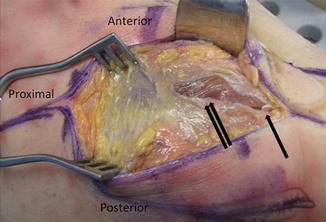
Fig. 6
An incision is made in the distal aspect of the fascia lata and the dissection is carried proximally where the gluteus maximus is split in line with its fibers (Single arrow: distal extent of fascial incision; Double arrow: gluteus maximus)