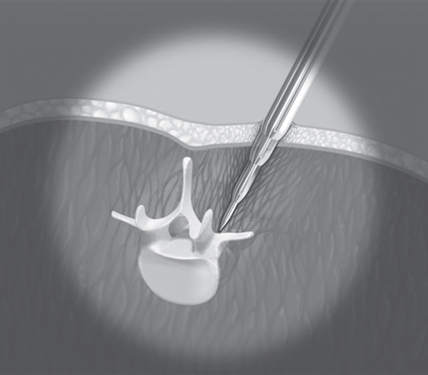
59 Only a small number of patients with low back pain are considered candidates for surgical intervention. Surgical options for the lumbar spine include lumbar decompression, microdiscectomy, and interbody fusion. These procedures are indicated only in those patients who show spinal instability, herniated disk disease, and/or spinal canal or neuroforaminal stenosis (i.e., narrowing). Typically, an associated leg pain due to compression of neural elements secondary to the previously mentioned changes is also observed. Surgical intervention is usually more successful at alleviating the associated leg pain due to nerve root compression than the low back pain. Traditionally, midline approaches to the posterior lumbar spine utilizing a large incision were used for these procedures. This technique demanded large amounts of soft-tissue dissection and prolonged use of self-retaining retractors to achieve adequate visualization, leading to long recovery times for patients undergoing the procedure. Recently, minimally invasive spine surgery has seen a surge in interest because of developments in technology that have solidified its ability to achieve similar outcomes to open spine surgery while reducing approach-related morbidities and hastening patient recovery. Candidates for minimally invasive posterior lumbar spine surgery can be categorized into one of three categories based on the underlying etiology of their symptoms. Those patients who have neural element compression due to herniated disk disease would be good candidates for endoscopic microdiscectomy. Those patients who have nerve root compression due to spinal stenosis may be candidates for a minimally invasive decompression. Those patients who have severe degeneration of the intervetebral disk or facet joints and associated instability of the spine may require a complete discectomy or decompression and fusion of the vertebral bodies. A complete medical history and physical examination should be undertaken to rule out potentially serious underlying medical conditions and help identify the specific pain etiology. When planning a minimally invasive surgery, body habitus and age should be taken under consideration and planned for, as the approach can be more technically demanding for obese or elderly patients. However, neither age nor body mass index (BMI) has been shown to be a contraindication to minimally invasive spine surgery, and it can be accomplished with similar outcomes to the general population. Appropriate imaging studies are vital to decision making in spine surgery, particularly when planning a minimally invasive approach. Imaging studies such as magnetic resonance imaging (MRI), computed tomography (CT), and plain radiographs are needed to determine the underlying spinal pathology. Invasive diagnostic testing, such as nerve root blocks and diskography, can play a role in determining pain etiology. Noninvasive procedures like epidural steroid injections can also play a role in elucidating the specific pain source and determining whether surgery will appropriately address the spinal pathology. Patients with degenerative spinal conditions should first attempt conservative treatment, such as nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, and epidural steroid injections. Surgical interventions should be undertaken only when these conservative treatments fail. In general, minimally invasive procedures may be considered as surgical approaches for treatment of herniated disk disease, spinal stenosis, or any range of spinal pathologies that cause spinal instability, such as spondylolisthesis. Minimally invasive approaches have been refined for microdiscectomy procedures, decompression surgery, and a variety of lumbar fusion procedures. Most of these procedures have been shown to be as effective as their counterpart open procedures. Generally, minimally invasive spine surgery utilizes both a slightly lateral, paramedian approach to minimize iatrogenic soft-tissue damage, and a tubular retractor system is used to create a small surgical portal for the procedure. Serial dilators are used to create the surgical corridor gently, providing access to the vertebral column while minimizing paraspinal muscle retraction (Fig. 59.1). The tubular retractor is then used to maintain visualization of the surgical site (Fig. 59.2). Tubular retractor systems also can be “wanded” to the contralateral side, allowing the surgeon to perform bilateral decompressions from a single unilateral incision. Pedicle screws and rods can also be placed percutaneously, further minimizing the amount of paraspinal muscle trauma during lumbar fusions. Minimally invasive versions of virtually all posterior lumbar spine surgical procedures have been refined and can be potentially utilized in the right circumstances. Fig. 59.1 Sequential dilators are used to prepare the surgical site for placement of a tubular retractor. (With permission of Endius Inc., Plainville, MA.)
Posterior Lumbar Minimally Invasive Surgery
![]() Classification
Classification
![]() Workup
Workup
History and Physical Examination
Spinal Imaging
![]() Treatment
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






