42 Polyarticular Arthritis
The history and physical examination are essential elements for diagnosis.
Exclude fibromyalgia as a cause of pain, and evaluate for common causes such as osteoarthritis.
Identify patients who are likely to have persistent, destructive disease.
Initiate prompt therapy in those with poor prognostic indicators.
Articular disorders are the most common cause of disability in the United States. Recent estimates by the Centers for Disease Control and Prevention (CDC) reveal that approximately one in five (49.9 million) adults in the United States have reported doctor-diagnosed arthritis; of these, 21.1 million adults have reported arthritis-attributable activity limitation.1 A substantial number of these patients manifest polyarticular joint involvement. The presentation of polyarticular joint pain poses a diagnostic challenge to the clinician, given the magnitude of the complaint, urgency to provide relief and preserve joint function, and the uncertainty of the outcome. Although many articular complaints (e.g., tendinitis, bursitis) are self-limiting and require only time and symptomatic management, others may present with or persist as chronic polyarthritis, with the potential for joint damage or disability. Knowledge of the most prevalent or commonly misconstrued causes of polyarthritis can facilitate an accurate diagnosis and appropriate therapy. This chapter will examine the diagnostic approach to polyarthritis, leaving its management to relevant chapters found throughout this textbook (see Chapters 71, 75 through 78, and 81).
Epidemiology and Societal Impact
The prevalence of arthritis is expected to rise as the U.S. population ages; an estimated 60% of the U.S. population older than 65 is affected by chronic joint symptoms.2 In 2002, the Behavior Risk Factor Surveillance System (BRFSS), a state-based random digit–dialed telephone survey of the U.S. civilian population, found that 69.9 million Americans had chronic joint symptoms defined as pain, aching, or stiffness in or around the joints lasting longer than 3 months.3 Of these, 25.1 million had not seen a physician, and more than 2 million had activity limitations. The survey also found that those who had never seen a health care provider for their joint complaints were likely to be male, to have lower educational levels, and to have no health insurance.4 An estimated 25% of patients will be unable to work within 7 years of disease onset. Direct and indirect costs are estimated at 1.2% of the U.S. gross domestic product, or $128 billion.1,5 These statistics encompass all forms of arthritis and extol the pervasive societal impact and cost of arthritis and the diagnostic deficit that exists. Thus a facile and accurate approach to patients with joint symptoms is sorely needed.
Defining Polyarthritis
1. Evaluate for the most prevalent causes—trauma, osteoarthritis, and fibromyalgia.
2. Distinguish between acute and chronic polyarthritis.
3. Delineate articular from periarticular disorders.
Approach to Diagnosis
Frequent Noninflammatory Polyarticular Scenarios
It is crucial that the clinician consider the most common causes of polyarticular and widespread musculoskeletal complaints—osteoarthritis (OA) and fibromyalgia (FM). Osteoarthritis affects 12 to 27 million, and fibromyalgia and related disorders (chronic fatigue syndrome, chronic widespread pain) affects 5 to 11 million in the United States alone.1 Although these two conditions are easily distinguishable from other arthropathies on clinical grounds (without laboratory or radiographic investigation), they often are missed for several reasons. First, it is possible to have more than one condition; RA is frequently accompanied by some degree of degenerative arthritis that may be constitutive, posttraumatic, or secondary to antecedent inflammatory disease. Similarly, patients with systemic lupus erythematosus (SLE) or Sjögren’s syndrome may have secondary FM observed as uncontrolled pain and poor sleep. Second, patients who once had an arthropathy (e.g., an inflammatory arthritis such as psoriatic arthritis) may find that it evolves into another type of arthritis. For example, psoriatic arthritis may cause years of swelling, stiffness, inflammation, and joint damage, only to “burn out” years later. However, the pattern of pain and stiffness may persist owing to secondary OA or FM, even though evidence of inflammatory arthritis is limited or nonexistent. Last, a detailed and skillfully performed musculoskeletal examination is required to discern that the joint pain is articular (e.g., RA) rather than extra-articular (e.g., FM) in origin, or that the swelling is related to synovial (e.g., RA) rather than bony (e.g., OA) hypertrophy, or that widespread pain is accompanied by tender trigger points (e.g., FM) rather than enthesitis (e.g., ankylosing spondylitis).
Fibromyalgia
This condition is five times more prevalent than rheumatoid arthritis and may underlie 10% to 20% of all outpatient musculoskeletal visits.2 It affects women more so than men, usually between the ages of 30 and 60 years, but people of all ages can be affected. Few patients announce widespread pain and tender points at presentation. Instead, most present because of regional joint or muscle pain, profound fatigue, and problems with mentation, memory, or headaches. Only upon further questioning will the examiner discern the wider distribution of painful tender points, joints, muscles, and tendons with an associated recent or long history of poor sleep. FM is a pain amplification disorder, with lowered pain thresholds, that often is accompanied by other “spastic conditions,” including migraine, irritable bowel syndrome, primary dysmenorrhea, atypical chest pain (often mislabeled as costochondritis), temporomandibular joint pain (without dysfunction or damage), and low back or neck pain. Diagnostic testing (laboratory tests, radiographs) is not necessary. The syndrome is established by history and examination and can be confirmed by (1) a positive response to simple analgesics, (2) improved sleep with better sleep hygiene plus sleep aids, (3) improvement attained with a stretching exercise program (e.g., swimming, Pilates, yoga, tai chi, physical therapy), and (4) uncontrolled depression or anxiety.
Osteoarthritis
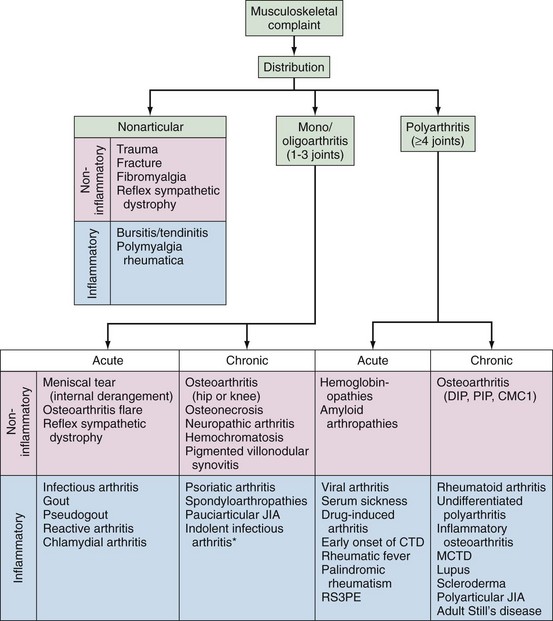
OA and FM can be considered or excluded on the basis of clinical findings. Should these not be applicable, other, more common disorders may be considered according to the chronology of the complaint (acute vs. chronic), the age of the subject, the presence of inflammatory or noninflammatory symptoms, and clues indicating high specificity (Figure 42-1).
History
The diagnosis of any polyarticular process relies heavily on the history and physical examination. When faced with a patient who presents with joint complaints, the goal of the encounter is to have answered the questions, “Is joint inflammation present?” and “Will it remit or persist?” This is important because inflammation that persists may yield significant damage or disability. In addition, it is estimated that more than half of patients who present with acute undifferentiated (often seronegative) polyarthritis will spontaneously remit. Although a 6-week history demarcates acute from chronic arthritis, persistent/chronic polyarthritis is best predicted by articular symptoms lasting 12 weeks or longer. Figure 42-1 presents an algorithm that may assist in formulating a differential diagnosis by providing answers to these questions. The algorithm considers patient demographics, symptom onset, patterns of involvement, disease course, and presence or absence of inflammation.
Demographics
Age, sex, and family background may provide clues to the type of arthritis. Gout is more common in men than in women; osteoarthritis affects older patients more often than younger counterparts, and spondyloarthritides have greater familial association than is seen with other inflammatory arthritides. Table 42-1 lists the differential diagnoses of patients who present with inflammatory arthritis according to age and sex.
Table 42-1 Differential Diagnoses of Patients Presenting with Inflammatory Arthritis*
| Age, yr | Men | Women |
|---|---|---|
| 18-30 | ||
| 30-60 | ||
| >60 |
PMR, polymyalgia rheumatica; RA, rheumatoid arthritis; RS3PE, relapsing symmetric seronegative synovitis with pitting edema.
* Spondyloarthropathies include ankylosing spondylitis, psoriatic arthritis, reactive arthritis, and enteropathic arthritis.
† Infectious arthritis includes gonococcal arthritis, Lyme arthritis, viral arthritis, and bacterial arthritis.
‡ Connective tissue disorders include systemic lupus erythematosus, scleroderma, Behçet’s disease, mixed connective tissue disease, and polymyositis/dermatomyositis.
§ Vasculitis includes polyarteritis nodosa, granulomatosis with polyangiitis (formerly Wegener’s granulomatosis), hypersensitivity vasculitis, and temporal arteritis.
Modified from Lipsky P: Algorithms for the diagnosis and management of musculoskeletal complaints, Am J Med 103:62S, 1997.
Presence of Inflammation
Evaluation for inflammation may be difficult. Studies have examined features of the history that may provide diagnostic clues to inflammation, such as morning stiffness and response to activity. Clearly, patients with all or some of the cardinal signs of inflammation (redness, warmth, swelling, pain in the morning) may have an inflammatory arthropathy. Morning stiffness (an inflammatory finding) is often confused with the “gel” phenomenon (a degenerative feature). Morning stiffness, defined as the time to maximal improvement after an extended period of inactivity (an overnight rest), typically improves with movement.6 In patients with inflammatory arthritis, the duration of morning stiffness is typically greater than 60 minutes. The gel phenomenon refers to short-lived stiffness that is brought on by short periods of rest and is common to patients with degenerative arthritis. Patients with inflammatory arthritis may present with pain without swelling, swelling without pain, or difficulty performing their activities of daily living without pain or swelling. It is important to distinguish whether inflammation is truly present as the cause of symptoms. Both arthralgia (joint pain) and arthritis (joint swelling from synovial fluid or tissue) may be present in new-onset polyarthritis; hence the joint examination is an essential component in establishing the diagnosis.
Physical Examination
Arthralgia vs. Arthritis
Characteristics that distinguish synovitis include warmth, erythema, tenderness to palpation, and synovial effusion. Any or all of these findings may accompany arthralgia. Range of motion, muscle strength, and function may be limited around the inflamed joint. In an effort to reduce joint volume and pain, the patient often will involuntarily hold the joint in a position of partial flexion. Hence, joint contractures may indicate an underlying inflammatory process (present or past). In RA, any diarthrodial joint can be affected, but the pattern of involvement typically involves the MCPs, PIPs, wrist, metatarsophalangeal joints (MTPs), and ankle joints.6 This pattern of involvement should be distinguished from osteoarthritis (DIPs, PIPs, carpometacarpal [CMC]1, knee, hip, spine), psoriatic arthritis (DIPs, PIPs, wrist, toes), and pseudogout (knee, wrist, MTPs). The accuracy of identifying synovitis depends on the skills and experience of the physician. The reproducibility of the physical examination in identifying synovitis has been a subject of concern raised in several studies.7–11 One study looked at whether rheumatologists can agree on the diagnosis of inflammatory arthritis; 24 patients were assessed by 6 rheumatologists—complete agreement was found in only 70% of cases; disagreement in the remaining 30% of cases ranged from 1 to 4 rheumatologists recognizing synovitis when others did not.12
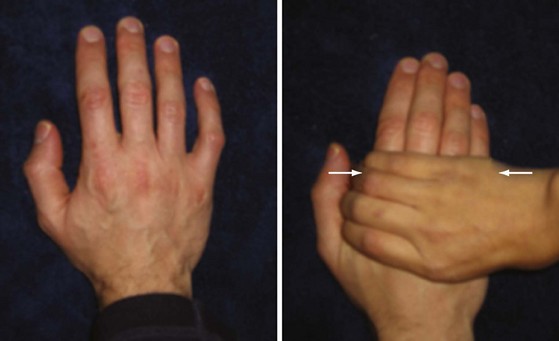
This is further illustrated by imaging studies. When the physical examination is compared with imaging, the joint examination has a reported sensitivity of 43%, specificity of 89%, and accuracy of 71% with magnetic resonance imaging (MRI) as the reference.11 Given the difficulty for many practitioners of discerning synovitis, Emery and colleagues have advocated the value of the MCP or MTP “squeeze test” (Figure 42-2). Their study found that pain upon transverse compression of the MCP or MTP joints (a positive squeeze test) has better specificity in identifying persistent arthritis than in finding arthritis in three or more joints, or symmetric arthritis.13 Currently, the joint examination is the gold standard for detection of synovitis; however, MRI and ultrasound may provide additional diagnostic evidence of synovitis in patients with chronic synovitis that is not evident on joint examination.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree